Managing a chronic disease can often feel overwhelming, but having a solid plan in place can make all the difference. Whether you're navigating the complexities of medication, dietary changes, or regular check-ups, understanding the right steps to take is crucial. In this article, we'll explore effective strategies and tips that can empower you to take control of your health journey. So, let's dive in and discover how you can enhance your chronic disease management experience!
Patient Information Management
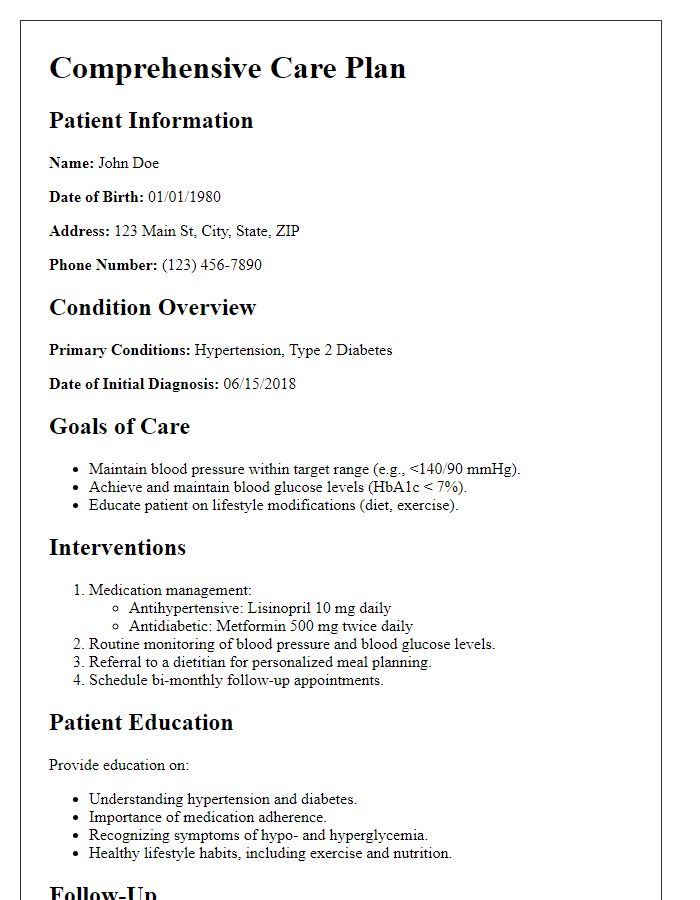
Chronic disease management programs focus on improving patient outcomes through effective information management systems. These systems, such as Electronic Health Records (EHR), facilitate seamless access to medical histories, treatment plans, and medication lists for healthcare providers. Regular updates allow tracking of vital signs (like blood pressure readings above 140/90, indicating hypertension) and lab results (for instance, HbA1c levels over 7% for diabetes management). Implementation of care coordination meetings can enhance communication among multidisciplinary teams, ensuring that specialists (like endocrinologists for diabetes and cardiologists for heart health) collaborate efficiently. Overall, structured patient information management is crucial in addressing the complexities of chronic conditions, ultimately aiming for improved healthcare delivery and patient-centered approaches.
Clear Communication of Treatment Plan
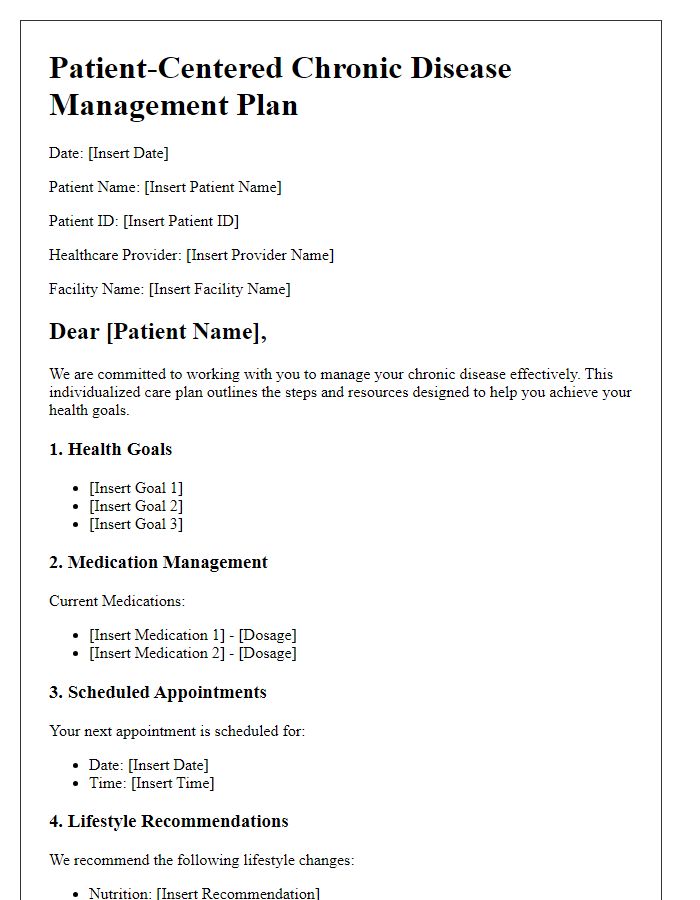
Chronic disease management requires clear communication of the treatment plan to ensure effective patient engagement and adherence. The treatment plan, tailored for each individual, must outline specific goals, such as reducing blood sugar levels in diabetes patients (targeting below 7% HbA1c) or lowering blood pressure (ideally below 130/80 mmHg). This plan should detail prescribed medications, such as Metformin for diabetes or Lisinopril for hypertension, including dosages and schedules. Education on lifestyle modifications, like a balanced diet rich in fruits and vegetables (5 servings daily) and regular physical activity (150 minutes weekly), plays a vital role in managing chronic conditions. Regular follow-up appointments, at least every three months, should be scheduled to evaluate progress, address challenges, and adjust the treatment plan as necessary. Comprehensive documentation, including patient preferences and concerns, ensures transparency and fosters a collaborative relationship between healthcare providers and patients.
Proactive Appointment Scheduling
Proactive appointment scheduling plays a crucial role in effective chronic disease management, particularly for conditions such as diabetes, hypertension, and asthma. Regular follow-up appointments, ideally every three to six months, allow healthcare professionals to monitor disease progression and adjust treatment plans accordingly. This process ensures patients remain engaged in their health journey, improving adherence to prescribed medications and lifestyle modifications. Clinics often utilize electronic health record systems to send automated reminders and facilitate scheduling, significantly enhancing patient compliance. Additionally, studies indicate that proactive management reduces hospitalizations and emergency room visits, ultimately lowering healthcare costs while improving quality of life for individuals suffering from chronic conditions.
Medication Adherence Strategies
Effective medication adherence strategies are crucial for managing chronic diseases, including diabetes and hypertension. Implementing reminders through smartphone applications can enhance adherence rates significantly, with studies indicating a 30% increase in compliance. Educational workshops hosted at local healthcare facilities, like the Community Health Center in Springfield, aim to empower patients with knowledge about their disease and the importance of medication. Support groups facilitate peer accountability and encouragement, fostering a sense of community among patients who understand each other's struggles. Regular follow-ups by healthcare providers ensure personalized adjustments, addressing barriers to adherence such as side effects or complex dosing schedules. Overall, integrating these strategies can improve health outcomes and quality of life for individuals living with chronic conditions.
Lifestyle Modification Suggestions
Chronic diseases, such as diabetes and hypertension, require significant lifestyle modifications to manage effectively. Regular physical activity, such as 150 minutes of moderate aerobic exercise weekly, can greatly enhance cardiovascular health. Dietary changes, like adopting a Mediterranean diet rich in fruits, vegetables, whole grains, and healthy fats, can lower cholesterol levels and improve blood sugar control. Monitoring daily caloric intake and maintaining a body mass index (BMI) within the healthy range (18.5-24.9) is crucial. Stress management techniques, such as mindfulness meditation or yoga, can reduce emotional triggers associated with chronic conditions. Adequate sleep, ideally 7-9 hours per night, can improve overall well-being and immune function, supporting disease management. Regular check-ups with healthcare providers are necessary to evaluate progress and adjust treatment plans effectively.
Letter Template For Chronic Disease Management Samples
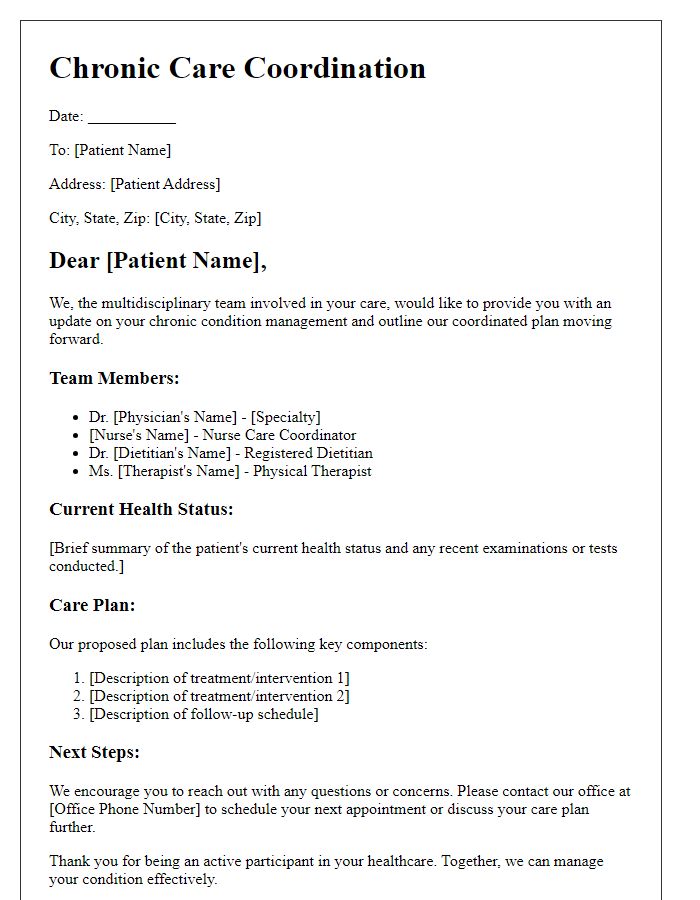
Letter template of multidisciplinary team for chronic care coordination.


Comments