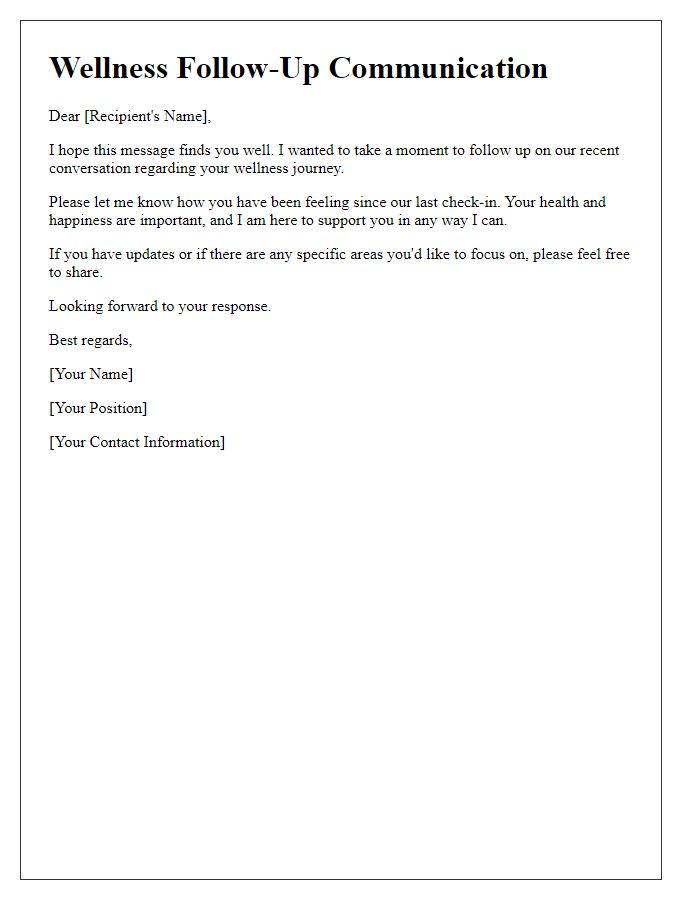
Hey there! We all know that recovery is a journey, and keeping track of your progress can make all the difference. Whether you're bouncing back from surgery or managing a chronic condition, monitoring your health can help you stay motivated and on the right path. Ready to learn more about effective recovery monitoring techniques? Let's dive in!
Patient Information and Identification
Patient information and identification play a crucial role in effective recovery monitoring within healthcare systems. Accurate patient records, including full names, unique identification numbers, and date of birth, facilitate personalized care during recovery. Detailed medical history, including previous diagnoses, treatments received, and allergies, ensures healthcare providers can make informed decisions. Additionally, regular updates on vital signs, such as heart rate and blood pressure, are essential for tracking recovery progress. For example, a patient from Seattle, diagnosed with pneumonia on October 1, 2023, may need daily monitoring of oxygen saturation levels to ensure proper healing. Utilizing electronic health record systems helps maintain organized and accessible patient information, which is vital for both immediate care and long-term recovery strategies.
Monitoring Schedule and Frequency
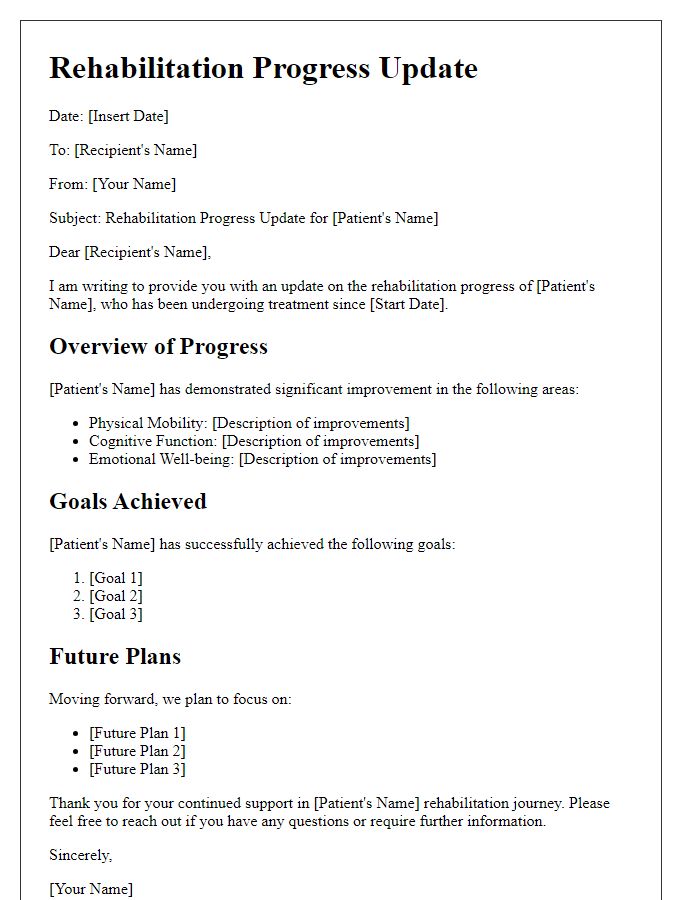
Regular patient recovery monitoring is essential for ensuring optimal healing and timely interventions. A structured monitoring schedule may involve daily assessments in the initial phase, particularly within the first week post-surgery or treatment, to closely observe vital signs, pain levels, and overall physical well-being. Following the acute phase, bi-weekly evaluations may be sufficient to track progress and address any emerging concerns. Locations for these assessments often include hospitals, outpatient clinics, or home care settings, depending on the patient's needs. Utilizing standardized recovery metrics, such as pain scales, mobility assessments, and wound evaluations, can enhance monitoring consistency and effectiveness. Frequent monitoring not only facilitates prompt identification of complications but also encourages patient engagement in the recovery process.
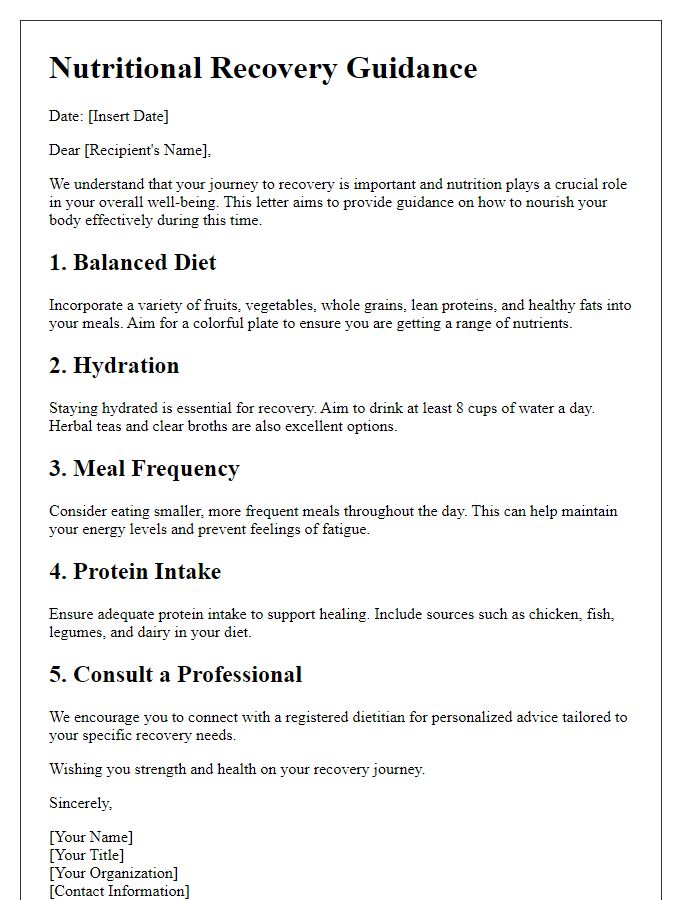
Health Metrics and Improvement Indicators
Monitoring patient recovery involves several key health metrics and improvement indicators that guide medical professionals in assessing progress. Vital signs, such as heart rate (typically between 60-100 beats per minute) and blood pressure (ideally around 120/80 mmHg), provide essential insights into cardiovascular health. Additionally, pain levels, often rated on a scale from 0 to 10, inform caregivers about the effectiveness of pain management strategies during rehabilitation. Functional mobility assessment includes tests like the Timed Up and Go (TUG), measuring the time taken to rise from a chair, walk three meters, and return, critical for evaluating recovery in geriatric patients. Laboratory tests, such as complete blood counts (CBC), can reveal immune function and detect signs of infection, while patient-reported outcome measures (PROMs) assess quality of life and overall satisfaction with health improvements. These metrics collectively aid in formulating personalized care plans, ensuring timely interventions and enhancing the recovery process at designated healthcare facilities like hospitals or rehabilitation centers.
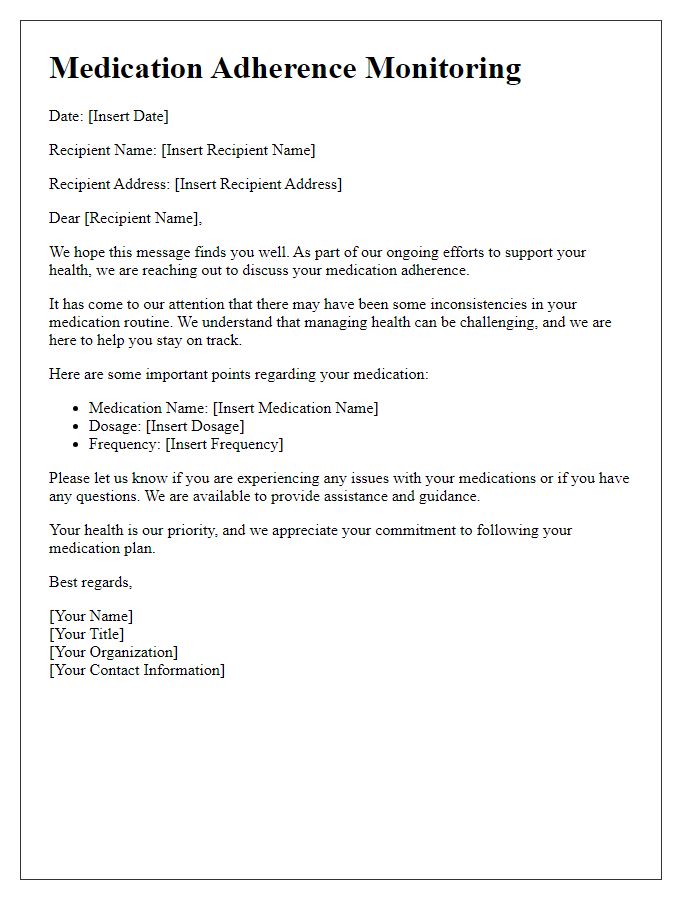
Medication and Treatment Plan
Monitoring patient recovery involves implementing a structured medication and treatment plan, vital for effective healing. Medications, such as antibiotics (e.g., Amoxicillin), are often prescribed to prevent infections and may require dosage adjustments based on patient response. Regular assessment of vital signs (temperature, blood pressure) is necessary to track recovery progress, ideally measured daily. Treatment plans may also include physical therapy sessions scheduled three times a week to enhance mobility and strengthen affected areas. Follow-up appointments, typically two weeks post-treatment (e.g., scheduled on November 15, 2023), ensure ongoing evaluation and adjustment of both medication and therapy strategies. Proper documentation of patient feedback and side effects is crucial for optimizing care.
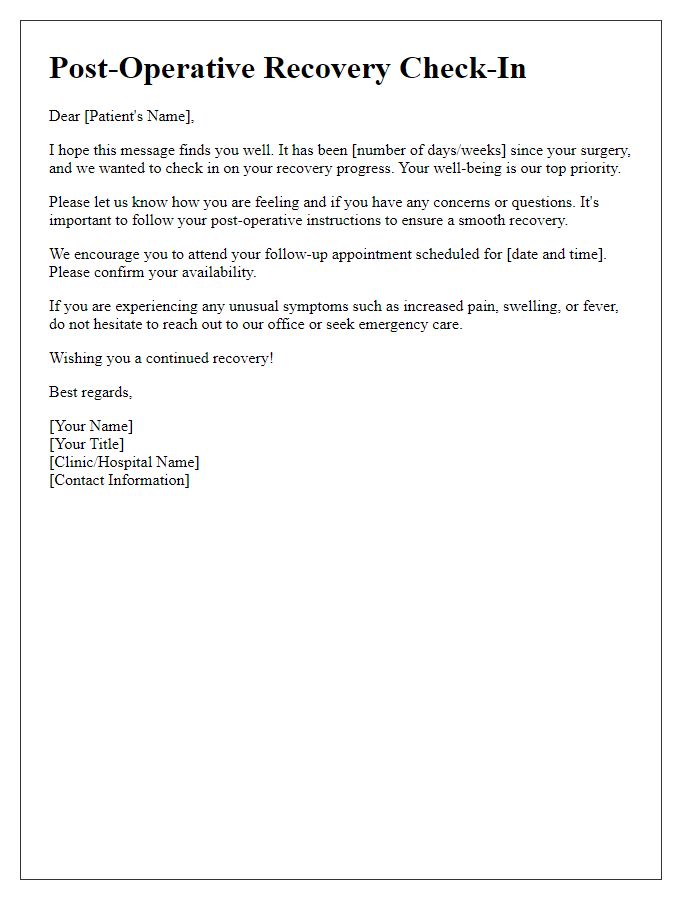
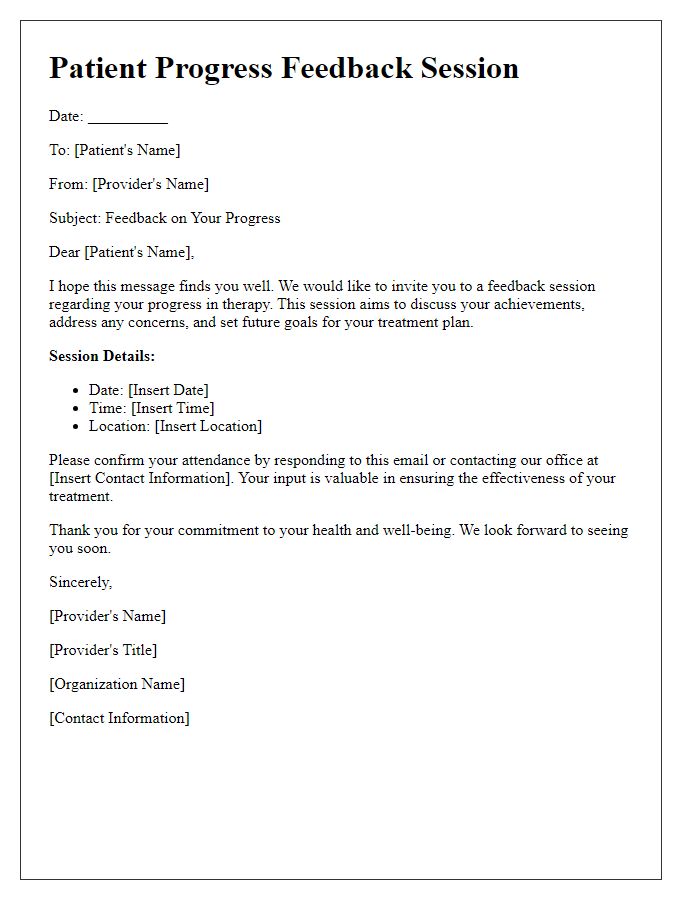
Communication Channels and Contact Information
Effective patient recovery monitoring relies on clear communication channels and readily available contact information. Healthcare providers utilize various methods, including telephone, email, and patient portals, to facilitate timely updates on recovery progress. For instance, a dedicated hotline allows patients to speak directly with care coordinators, enhancing the support experience. Email communications, tailored to individual treatment plans, provide detailed instructions regarding medications, appointments, and lifestyle adjustments essential for recovery. Patient portals, such as MyChart, enable secure access to health records, lab results, and direct messaging with healthcare teams, promoting active participation in recovery. Ensuring patients have access to this information fosters a collaborative approach to health management, ultimately leading to improved outcomes.


Comments