Are you wondering how to enhance patient mobility in your healthcare facility? Improving mobility not only boosts the overall well-being of patients but also fosters a quicker recovery process. In this article, we'll explore effective strategies and best practices that can significantly aid in promoting movement among patients. So, grab a cup of coffee and dive in as we uncover the essential steps to enhance patient mobility!
Greeting and Patient Identification
In the realm of healthcare, initiating communication is crucial for patient engagement. A greeting establishes a warm rapport, while patient identification focuses on providing tailored care. The first step might involve addressing the patient by name, fostering a personal connection. Following this, confirming essential details, such as date of birth and medical record number, ensures accurate identification within the hospital database. This approach instills a sense of trust and safety, enabling healthcare professionals to effectively discuss mobility improvement plans tailored to the patient's unique needs. Clear communication and patient-centered interactions enhance the overall quality of care provided.
Purpose of Correspondence
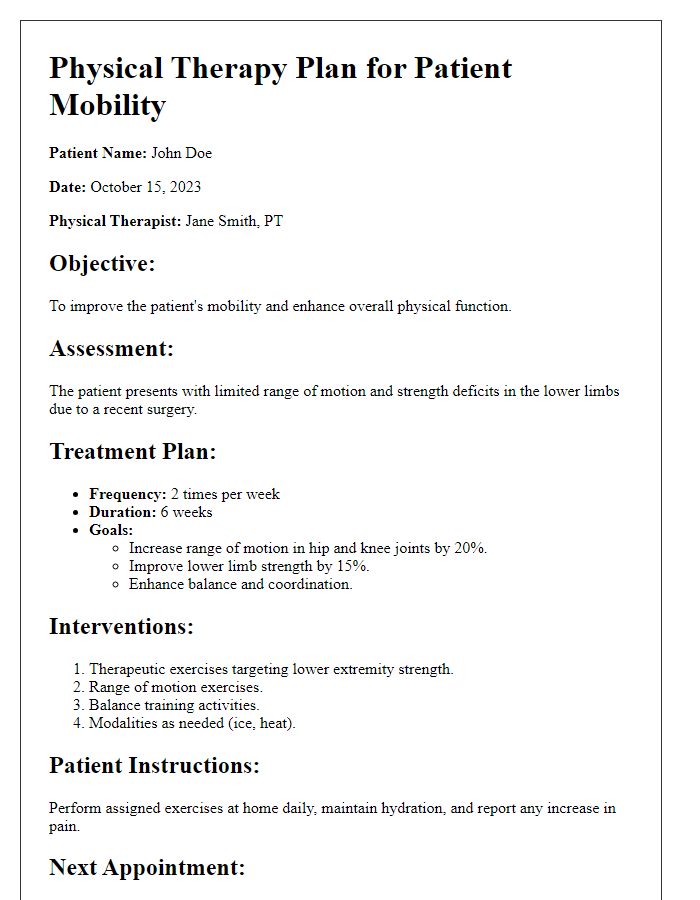
Improving patient mobility is essential for recovery and overall well-being in healthcare settings. Mobility assessment tools (such as the Timed Up and Go test) can gauge functional abilities, helping healthcare providers customize rehabilitation strategies. Evidence indicates that increased mobility reduces hospital stay durations (by as much as 2.5 days in some studies) and lowers the risk of complications (such as deep vein thrombosis). Implementing structured mobility programs in institutions like Mount Sinai Hospital can lead to significant advancements in patient outcomes. Staff training on proper lifting techniques and the use of assistive devices (like walkers or canes) enhances safety during ambulation, ensuring patient confidence and independence in movement.
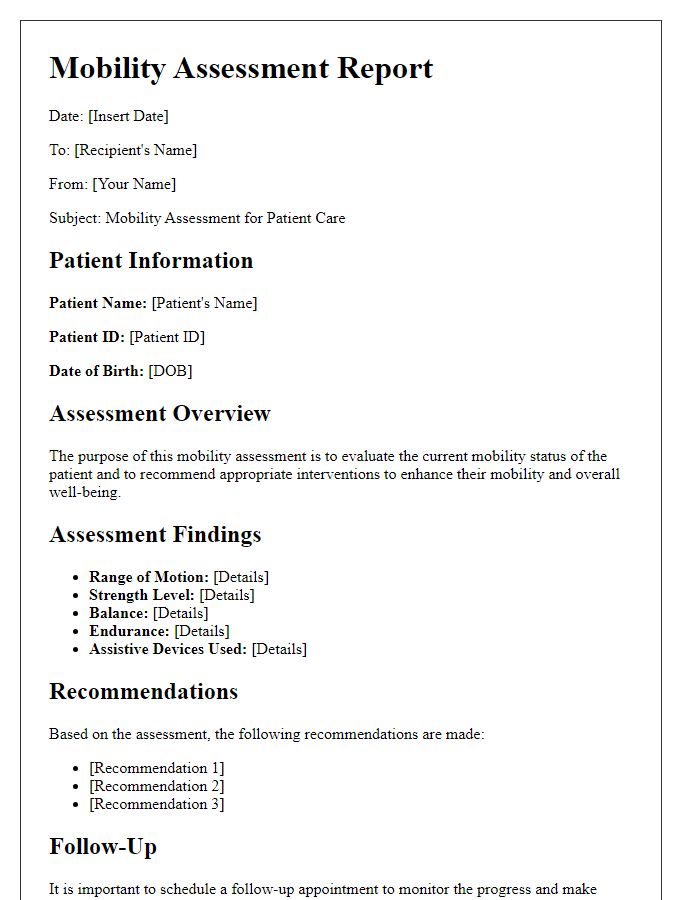
Current Mobility Assessment
Current mobility assessment reveals challenges in the patient's ability to navigate both indoor and outdoor environments. The patient demonstrates reduced ambulation with a recorded distance of approximately 50 feet using a standard walker in physical therapy sessions. Gait analysis shows an unsteady posture and potential risk for falls, particularly on uneven surfaces, such as those found in residential areas or community parks. Range of motion tests indicate limitations in hip and knee flexion, notably affecting transitions, like standing from a seated position. Strength assessments further identify weakness in lower extremities, particularly in the quadriceps and hamstrings, necessitating an individualized mobility plan aimed at gradually increasing endurance and stability. Contributing factors, including prior medical history of stroke in April 2022 and ongoing pain management for osteoarthritis, complicate the mobility trajectory. Prioritizing safety measures, like non-slip footwear and environmental modifications, is crucial in enhancing overall mobility, enabling greater independence and quality of life.
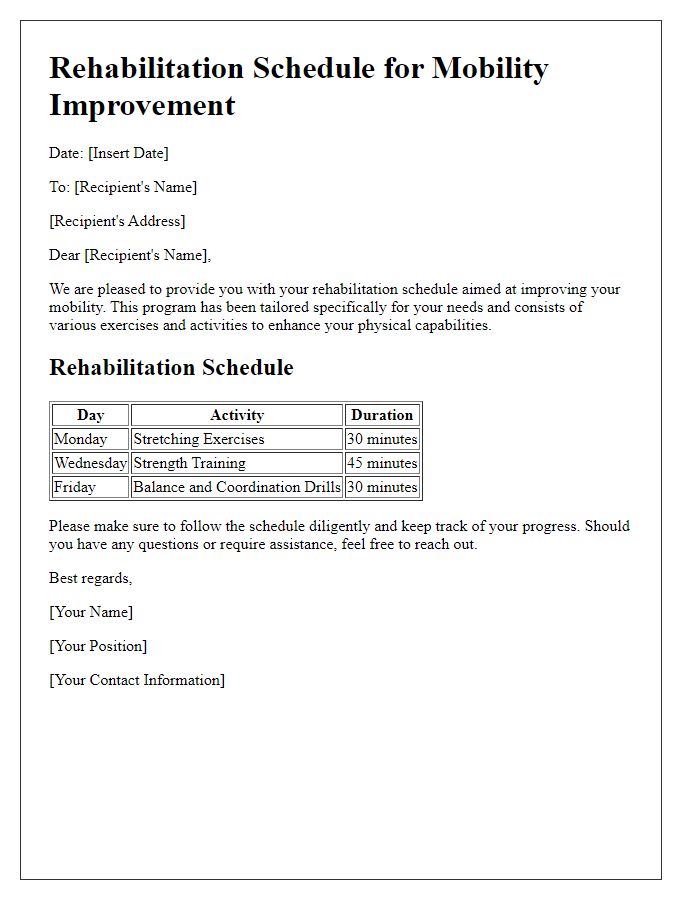
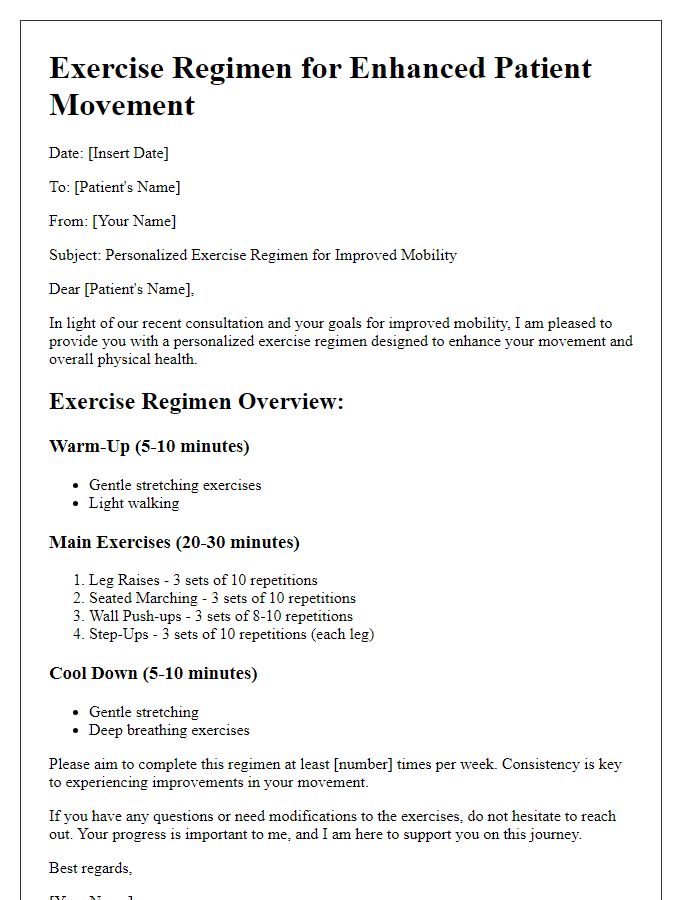
Recommended Exercises and Activities
Improving patient mobility requires a personalized approach to exercise and activity recommendations. Strength-building exercises such as resistance training with bands or weights (around 2-5 pounds for beginners) can enhance muscle strength, particularly in the lower body, crucial for activities like walking. Flexibility exercises, including stretching routines focusing on hamstrings and quadriceps, should be performed daily to increase range of motion, aiming for a duration of 15-30 seconds per stretch. Balance training activities, such as standing on one leg or using a wobble board, can decrease fall risk and improve stability, recommended for 10-15 minutes each session, 3-4 times a week. Incorporating aerobic activities like walking or cycling for at least 150 minutes weekly can significantly enhance cardiovascular endurance, vital for overall mobility. Engaging in functional activities, such as transferring from a seated position, practicing stair climbing, or using assistive devices, reinforces practical mobility skills that translate to daily living scenarios.
Follow-Up and Contact Information
Patient mobility improvement strategies can significantly enhance recovery outcomes following surgeries like hip or knee replacements. Personalized rehabilitation programs often involve physical therapy exercises designed to increase strength, flexibility, and endurance specific to the patient's needs. Studies indicate that engaging patients in these programs can lead to improved range of motion within six weeks post-operation. Follow-up appointments, typically scheduled every two to four weeks, allow healthcare providers to assess progress and adjust therapeutic techniques accordingly. Contact information for rehabilitation centers, like the prestigious Mayo Clinic in Rochester, Minnesota, or specialized physiotherapy practitioners, should be readily available to ensure support continues beyond initial recovery phases. Addressing potential barriers, such as access to mobility aids or transportation for regular sessions, is vital in facilitating ongoing improvement in patient mobility.



Comments