Are you navigating the sometimes tricky waters of insurance pre-authorization requests? Understanding the essential elements of a well-crafted letter can make all the difference in getting the approval you need. A strong letter not only outlines the medical necessity of a treatment but also clearly communicates with the insurance provider. So, if you want to ensure your request hits all the right notes, keep reading for a detailed guide on creating the perfect pre-authorization letter!
Patient's personal and insurance information
When submitting an insurance pre-authorization request, providing detailed information about the patient is crucial for a smooth process. This typically includes the patient's full name, date of birth, and insurance policy number, ensuring accurate identification and coverage confirmation. It's important to include the insurance provider's name and contact information, along with the policyholder's relationship to the patient, which could be a parent or guardian. Additionally, detailing the specific medical procedure or service being requested, along with the corresponding CPT codes and diagnosis codes, helps in clearly communicating the necessity of the pre-authorization. Accurate submission of these details can significantly improve the likelihood of timely approval and avoid potential delays in patient care.
Detailed description of medical necessity
Pre-authorization requests for medical procedures involve a comprehensive understanding of the patient's medical history, specific diagnoses, and the proposed treatment plan. For example, a surgical intervention like a total knee arthroplasty may be medically necessary for patients with severe osteoarthritis, characterized by joint pain and dysfunction. Patients often experience a reduction in quality of life when conservative treatments such as physical therapy or anti-inflammatory medications fail, evidenced by significant disability scores reflecting impaired mobility. The necessity for pre-authorization stems from ensuring the procedure aligns with insurance criteria, such as the minimum range of motion required and the duration of conservative management attempted. Documentation should include diagnostic imaging results like X-rays and MRIs, which reveal joint degeneration, alongside a clear outline of the treatment pathway illustrating why surgery is the recommended course of action to remediate debilitating symptoms.
Comprehensive CPT/ICD codes
Requesting a pre-authorization for insurance can involve complex procedures and coding. CPT (Current Procedural Terminology) codes categorize medical services, while ICD (International Classification of Diseases) codes identify specific health conditions. For instance, CPT codes such as 99213 for established patient office visits or 27652 for ankle joint injection may be necessary to document the services required. ICD codes, like M17.11 for unilateral primary osteoarthritis of the knee, provide context for the medical necessity of those services. Precise coding is critical to ensure that insurance providers correctly assess the request, leading to timely approvals for necessary treatments or diagnostic procedures. Comprehensive documentation should include patient details, service dates, and healthcare provider information to facilitate the pre-authorization process.
Physician's credentials and contact information
In insurance pre-authorization requests, detailed physician credentials and contact information play a crucial role. Credentials include the physician's full name, board certifications, and medical license number, showcasing qualifications and expertise in a specific field such as cardiology or orthopedics. Contact information consists of the office address, telephone number, and fax number, ensuring efficient communication for follow-up inquiries. This information aids insurance providers in validating the physician's practice and understanding the medical necessity of prescribed treatments or procedures, facilitating smoother approval processes. Complete and accurate details can significantly impact timely authorization, benefiting patient care.
Supporting medical documentation and evidence
Medical pre-authorization requests for insurance coverage require thorough documentation and compelling evidence to support the necessity of specific treatments or procedures. Essential elements include physician letters detailing diagnosis codes from the International Classification of Diseases (ICD) corresponding to the patient's condition. Medical records documenting the patient's treatment history, including previous interventions, test results, and response to therapies, provide context for the requested procedure. Imaging studies such as MRI or CT scans must be included where relevant, demonstrating the need for further action. Additionally, clear explanations of the proposed treatment plans, outlining expected benefits and potential risks, enhance the justification. Standardized forms from the insurance company, completed with accurate policy numbers, can streamline the pre-authorization process. Comprehensive compilations of this information can significantly improve the chances of approval and ensure timely access to necessary care.
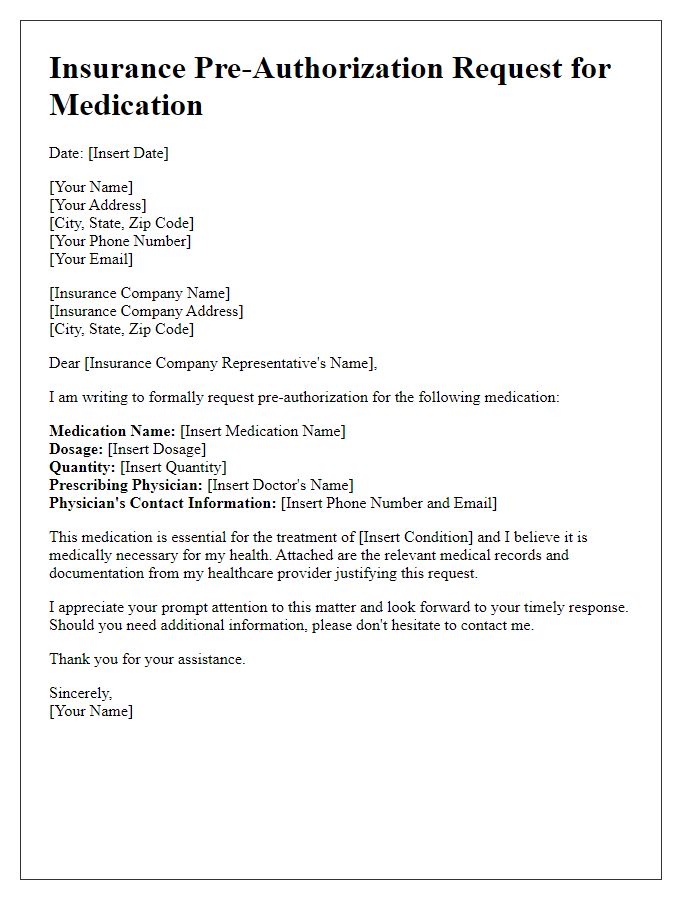
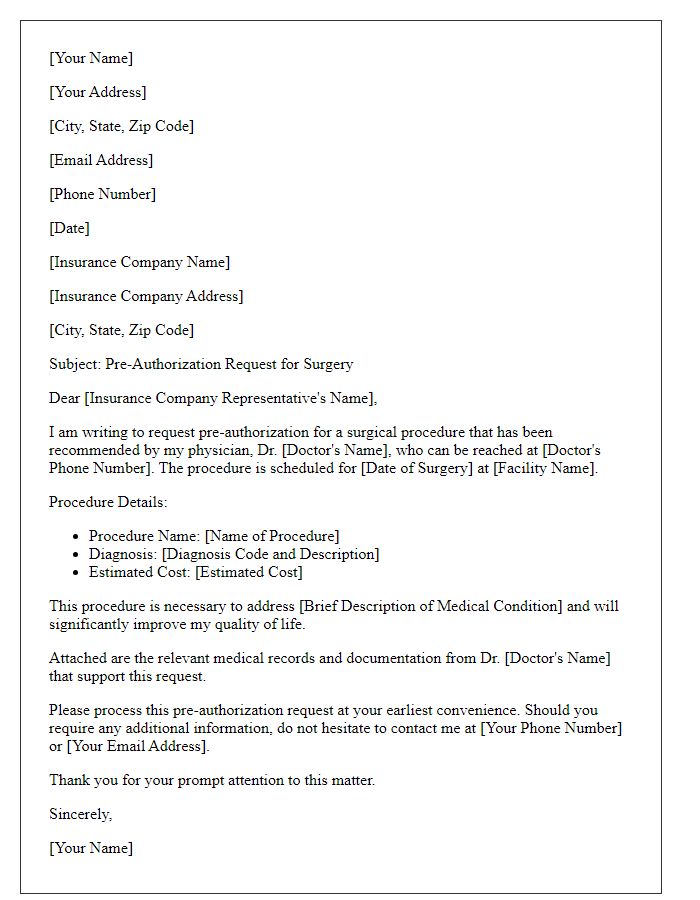
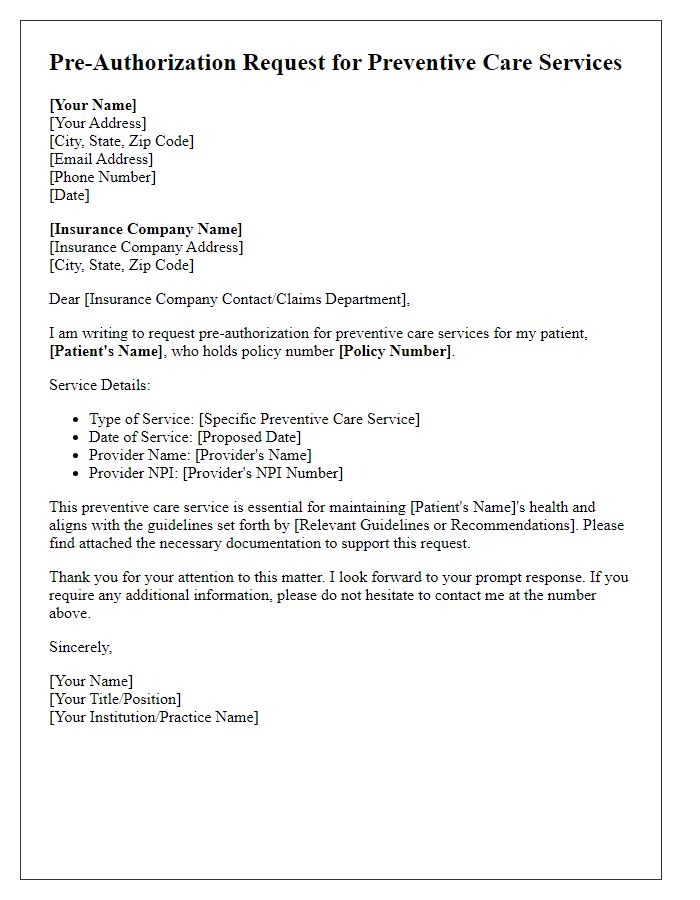
Letter Template For Insurance Pre-Authorization Request Samples
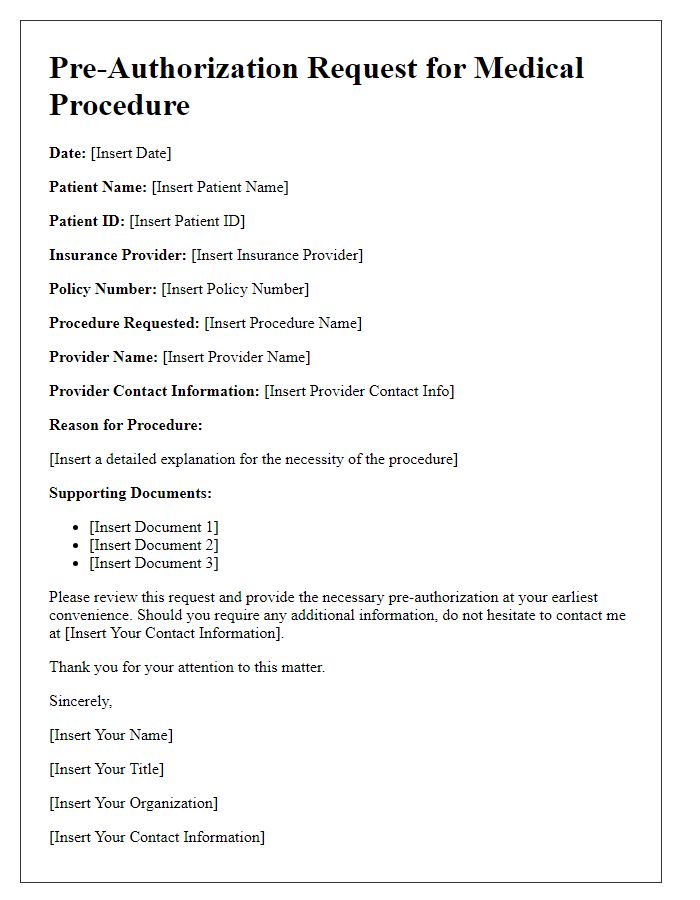
Letter template of insurance pre-authorization request for medical procedure
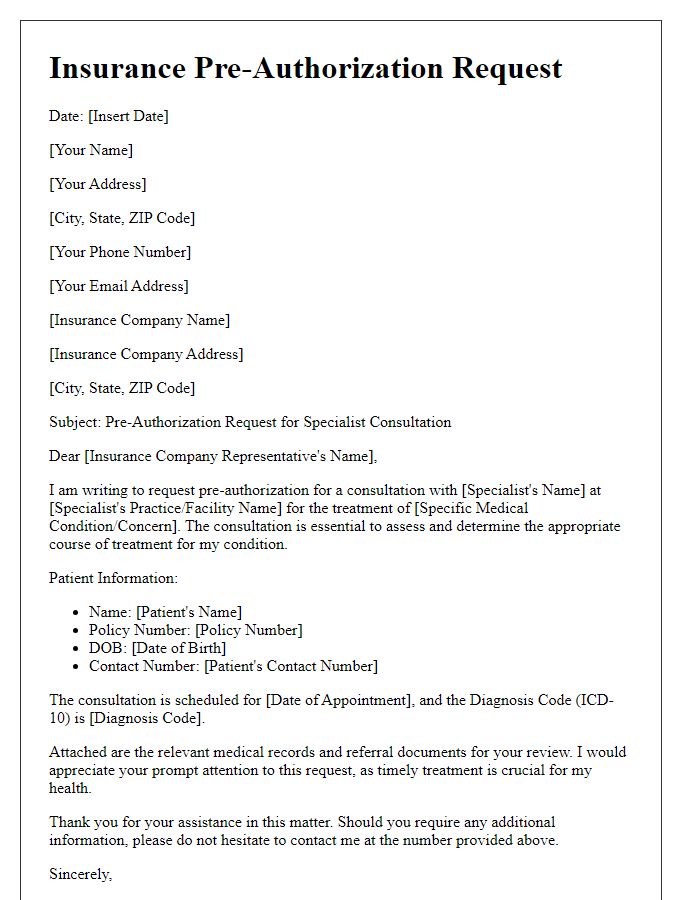
Letter template of insurance pre-authorization request for specialist consultation
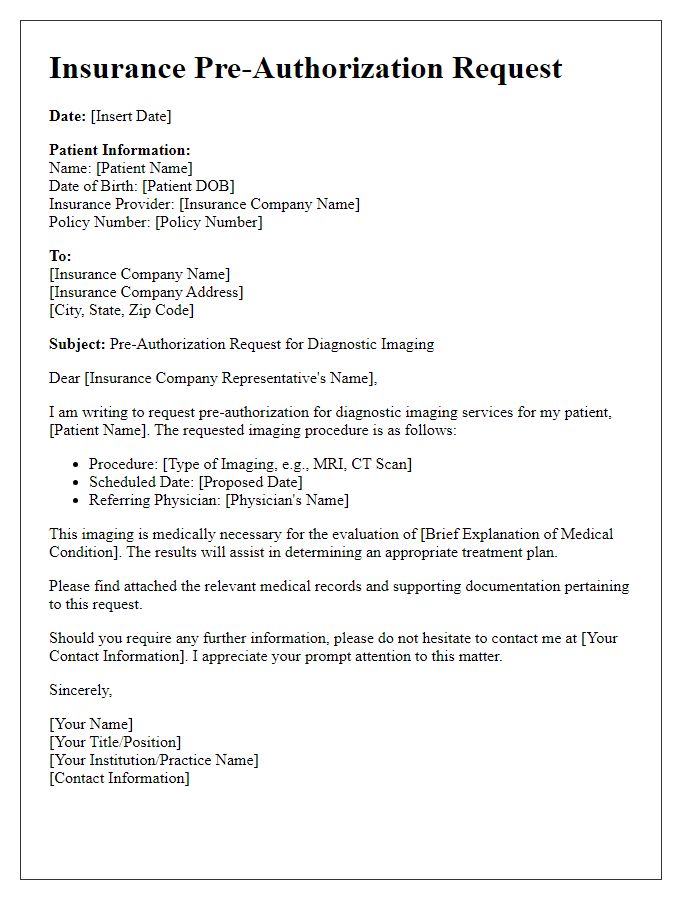
Letter template of insurance pre-authorization request for diagnostic imaging
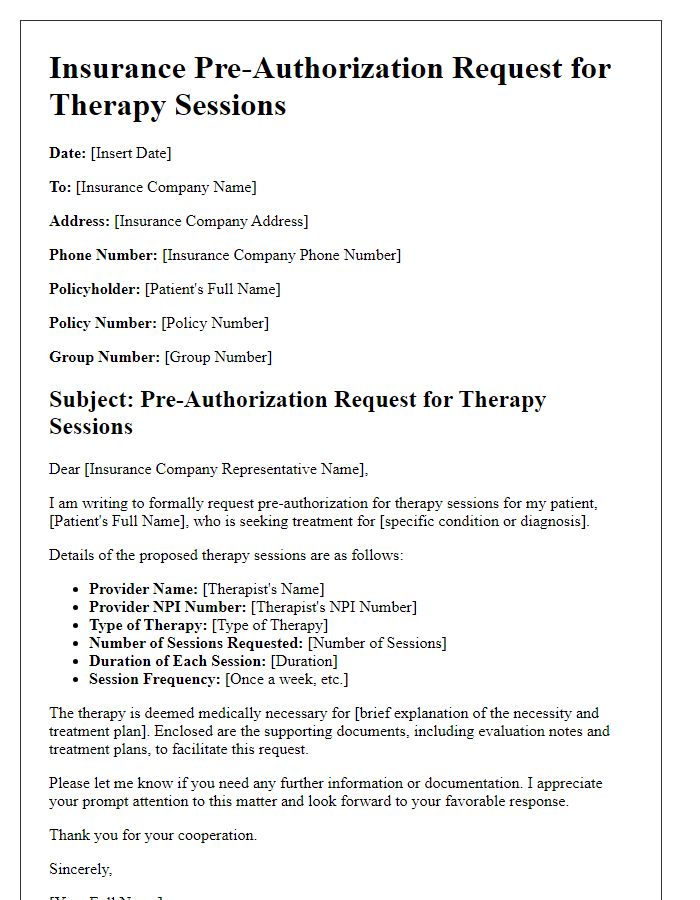
Letter template of insurance pre-authorization request for therapy sessions
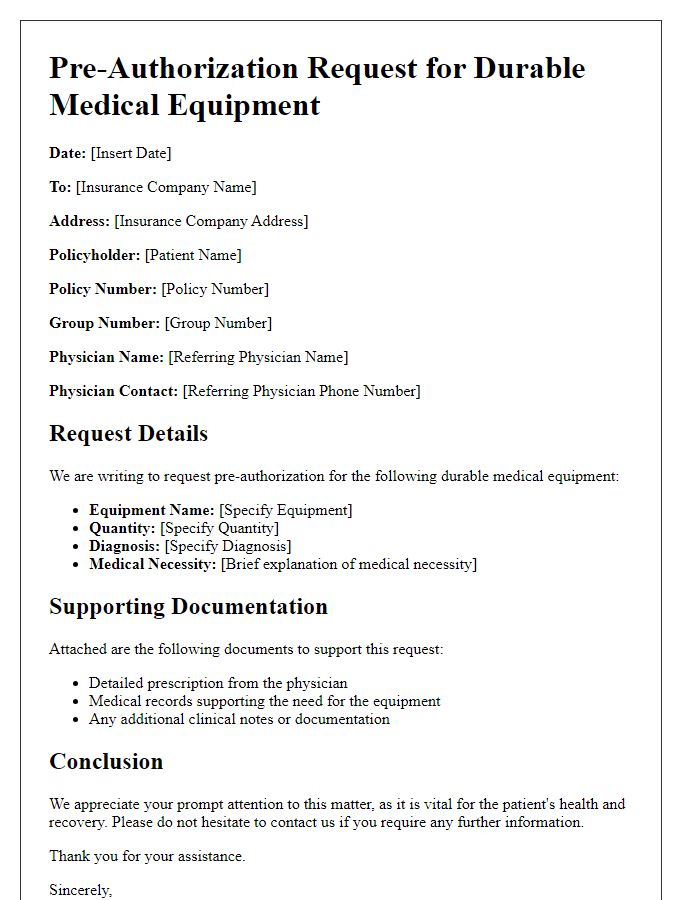
Letter template of insurance pre-authorization request for durable medical equipment
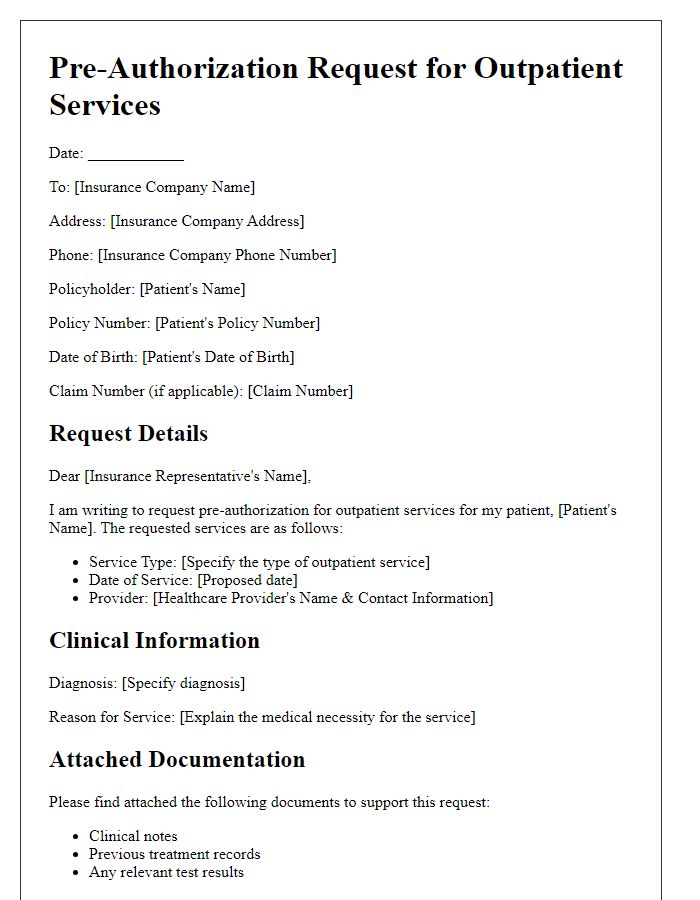
Letter template of insurance pre-authorization request for outpatient services
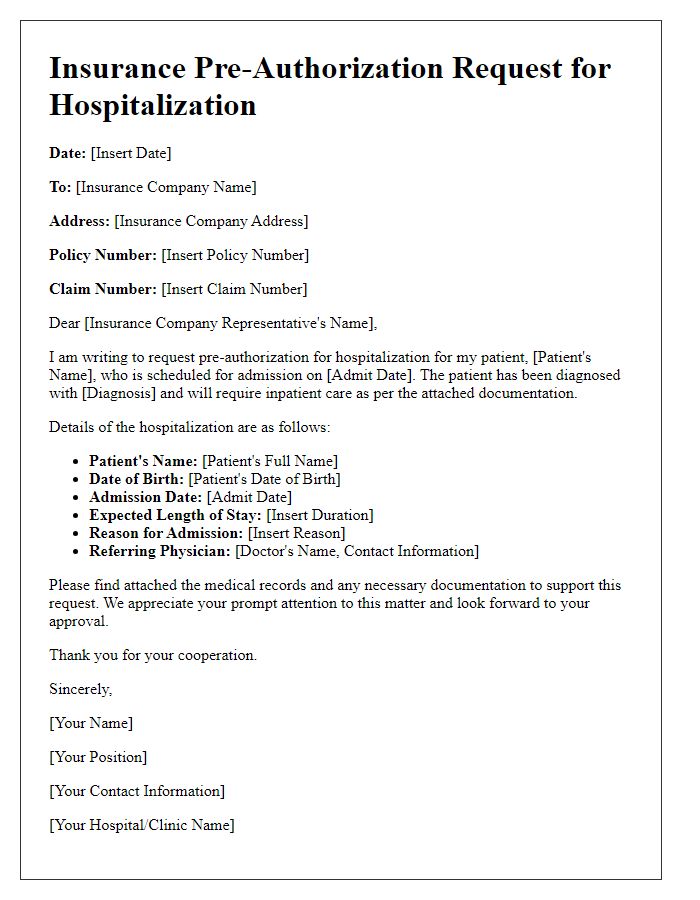
Letter template of insurance pre-authorization request for hospitalization


Comments