Managing hypertension can feel overwhelming, but understanding its best practices can make all the difference. From dietary adjustments to regular exercise, there are numerous strategies that can help keep blood pressure in check. Additionally, staying informed about medication options and monitoring techniques is crucial for effective management. If you're curious about how to take control of your blood pressure health, read on for more insightful tips and resources!
Patient Information and Background
Hypertension, also known as high blood pressure, affects approximately 1.13 billion people worldwide, increasing the risk of cardiovascular diseases and stroke. Patient demographics play a crucial role in managing hypertension effectively, with factors such as age, weight, family history, and lifestyle contributing to the overall risk profile. For instance, adults aged 45 or older often exhibit higher prevalence rates, particularly in individuals who lead sedentary lifestyles or have poor dietary habits, including high sodium intake. Regular monitoring of blood pressure, ideally in a clinical setting or at home using digital sphygmomanometers, is essential for assessing treatment efficacy. Lifestyle modifications, including the DASH diet (Dietary Approaches to Stop Hypertension), rich in fruits and vegetables, and consistent physical activity (at least 150 minutes of moderate exercise weekly), are foundational practices in hypertension management. Medications, such as ACE inhibitors or calcium channel blockers, are often prescribed based on specific patient health profiles to achieve optimal blood pressure control, emphasizing the need for continuous patient education and adherence to treatment plans.
Treatment Plan and Goals
Developing an effective hypertension management plan requires a multifaceted approach focused on lifestyle modification, medication adherence, and regular monitoring of blood pressure levels. Key lifestyle changes include adopting a heart-healthy diet such as the DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes fruits, vegetables, whole grains, and lean proteins, while limiting sodium intake to less than 2,300 mg daily, or ideally 1,500 mg. Regular physical activity, such as 150 minutes of moderate aerobic exercise per week, is essential for weight management and overall cardiovascular health. Proper medication management, using antihypertensive agents tailored to individual patient needs, is crucial; common categories include ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers. Setting specific goals, such as achieving and maintaining a target blood pressure of less than 130/80 mmHg, will help guide both patients and healthcare providers in evaluating the effectiveness of the treatment plan. Ensuring regular follow-up appointments, at least quarterly, to assess blood pressure readings and adjust treatment as necessary can significantly improve outcomes for individuals living with hypertension.
Monitoring and Follow-up Schedule
Effective management of hypertension requires consistent monitoring and follow-up schedules to maintain optimal blood pressure levels. Regular check-ups, ideally every one to three months depending on patient stability, are essential to assess the effectiveness of treatment plans, including lifestyle modifications and medications. Home blood pressure monitoring devices are recommended for daily readings, helping in identifying patterns and potential fluctuations. Patient education on recognizing symptoms of hypertension, such as headaches or dizziness, plays a crucial role in proactive management. Collaboration with healthcare professionals, including primary care physicians and specialists, ensures a comprehensive approach to treatment, potentially involving dietary changes, physical activity, and adherence to prescribed antihypertensive medications like ACE inhibitors or diuretics. Utilizing tools like patient health records can facilitate tracking progress and adjusting treatment plans as needed to achieve blood pressure goals, typically below 130/80 mmHg as advised by the American College of Cardiology. Regular assessments of related health metrics, including cholesterol levels and kidney function, further enhance the effectiveness of hypertension management practices.
Lifestyle and Dietary Recommendations
Hypertension, commonly referred to as high blood pressure (120/80 mmHg is considered normal), can significantly impact overall health if not managed effectively. Incorporating regular physical activity, such as brisk walking (at least 150 minutes a week), can lower blood pressure and improve cardiovascular health. Adopting the DASH diet (Dietary Approaches to Stop Hypertension) emphasizes fruits, vegetables, whole grains, and low-fat dairy while reducing saturated fats and cholesterol. Reducing sodium intake to 2,300 milligrams or less per day can further help maintain healthy levels. Monitoring alcohol consumption is vital, with guidelines suggesting moderate intake (one drink per day for women, two for men). Emphasis on stress management techniques, such as yoga or meditation, can also play a crucial role in both mental and physical well-being. Regularly checking blood pressure and consulting healthcare providers for personalized strategies is essential for effective hypertension management.
Medication Management and Adjustments
Effective hypertension management practices involve routine medication management and strategic adjustments to ensure optimal blood pressure control. Antihypertensive medications, such as ACE inhibitors (e.g., Lisinopril) or calcium channel blockers (e.g., Amlodipine), typically require monitoring for side effects like dizziness or renal impairment. Regular blood pressure readings conducted at home or during appointments can inform necessary dosage adjustments, aiming for target levels, often below 130/80 mmHg, per guidelines from the American Heart Association. Patient adherence remains crucial, with education on the importance of lifestyle modifications, including diet changes (e.g., DASH diet) and increased physical activity (at least 150 minutes weekly). Collaboration with healthcare providers ensures timely adjustments based on individual responses and co-morbidities, enhancing overall cardiovascular health.
Letter Template For Hypertension Management Practices Samples
Letter template of recommended hypertension management strategies for healthcare providers.
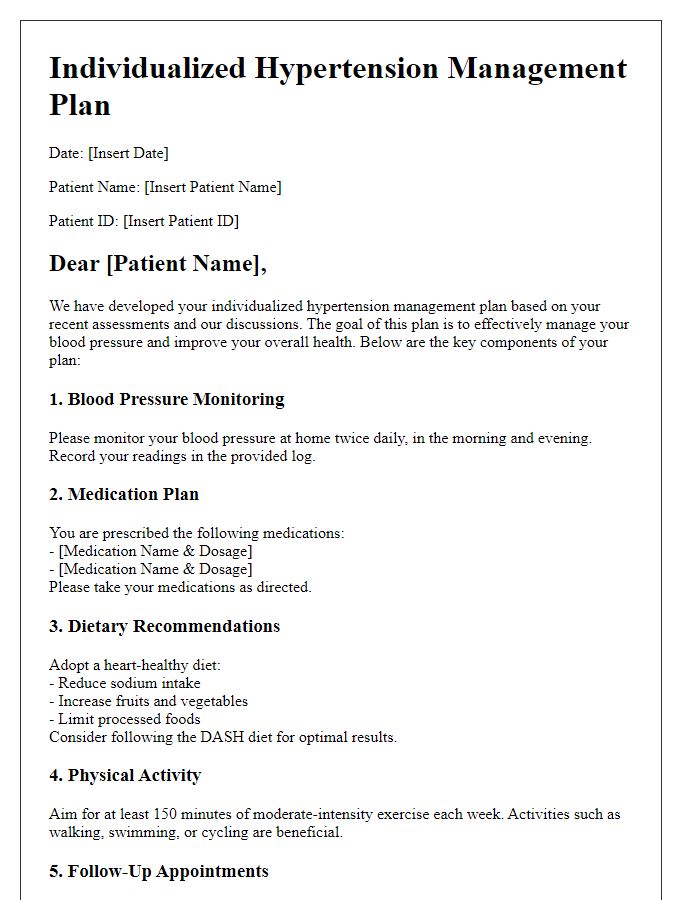
Letter template of individualized hypertension management plans for patients.
Letter template of community support initiatives for hypertension awareness.
Letter template of lifestyle modification programs for hypertensive patients.
Letter template of collaboration between primary care and cardiology for hypertension care.
Letter template of medication adherence strategies for hypertension treatment.


Comments