In today's world, where personal information is more vulnerable than ever, ensuring patient confidentiality is paramount for healthcare providers. This agreement serves as a foundation for trust between you and your healthcare team, paving the way for open and honest communication. By safeguarding your sensitive information, we prioritize your privacy and uphold the highest standards of care. Curious about how this agreement works and what it means for your treatment? Read on to discover the details!
Purpose of Agreement
A patient confidentiality agreement serves a crucial role in protecting sensitive health information for individuals, ensuring compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States. This agreement outlines the responsibilities of healthcare providers, institutions, and their employees to safeguard personal and medical details, ensuring that data remains confidential and is only shared with authorized parties for treatment, payment, or healthcare operations. Violations of this agreement can lead to legal repercussions and loss of trust, highlighting the significance of maintaining patient confidentiality as a fundamental ethical obligation in the medical field.
Definitions and Terms
A patient confidentiality agreement is a vital document that outlines the responsibilities of healthcare providers in safeguarding sensitive medical information. Key terms include "Protected Health Information (PHI)," which encompasses any data that can identify an individual, such as medical histories, treatment records, and personal identifiers inherent in Electronic Health Records (EHR) systems. "Confidentiality" refers to the ethical and legal duty to keep patient information private, in accordance with regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the United States, established in 1996. The term "disclosure" signifies the act of releasing or sharing PHI with third parties, which should only occur under specific conditions, such as patient consent or legal requirements. Furthermore, "breach" indicates an unauthorized access or disclosure of patient information, necessitating immediate reporting and remediation actions per institutional protocols. Awareness and understanding of these terms ensure compliance and foster trust in the patient-provider relationship within healthcare settings.
Obligations and Responsibilities
In the realm of healthcare, patient confidentiality agreements serve as a critical framework that governs the obligations and responsibilities of medical providers and their staff. Such agreements are designed to protect sensitive patient information, including medical histories, diagnoses, and treatment plans, ensuring compliance with laws like the Health Insurance Portability and Accountability Act (HIPAA) established in 1996. Healthcare personnel must maintain the confidentiality of patient records, safeguarding access to data only for authorized individuals involved in the patient's care or billing processes. Violations of these commitments may lead to significant legal repercussions, including fines reaching thousands of dollars for breaches. Upon signing, healthcare providers acknowledge their duty to train employees on privacy practices, ensuring that all personal health information (PHI) remains secure and confidential, thus fostering trust in the patient-provider relationship. Regular audits and assessments enhance compliance, further fortifying the integrity of patient privacy within healthcare settings.
Duration and Termination
This confidentiality agreement outlines the duration of the obligations concerning patient information and the conditions under which the agreement may be terminated. The confidentiality obligations shall remain in effect for a period of five years from the date of disclosure of the patient information. Upon expiration of this period, the parties may elect to renew or terminate the agreement, with written notice required at least thirty days in advance. Termination may also occur due to breach of terms, with immediate effect upon written notice. Any patient information retained must continue to be protected according to applicable laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), even after the termination of this agreement.
Consequences of Breach
A breach of patient confidentiality can lead to serious ramifications, impacting both the healthcare provider and the patient. Legal repercussions may include hefty fines imposed by regulatory bodies such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, where violations can range from $100 to $50,000 per incident, depending on the level of negligence. Patients may experience emotional distress and loss of trust towards healthcare professionals, potentially affecting their willingness to share vital information necessary for effective treatment. Additionally, the healthcare organization may face reputational damage, leading to decreased patient enrollment and funding challenges. Compliance training programs for staff may also become mandatory to prevent future breaches, adding to operational costs. Safeguarding patient information, therefore, is essential not only for legal compliance but also for maintaining the integrity of the patient-provider relationship within clinical settings.
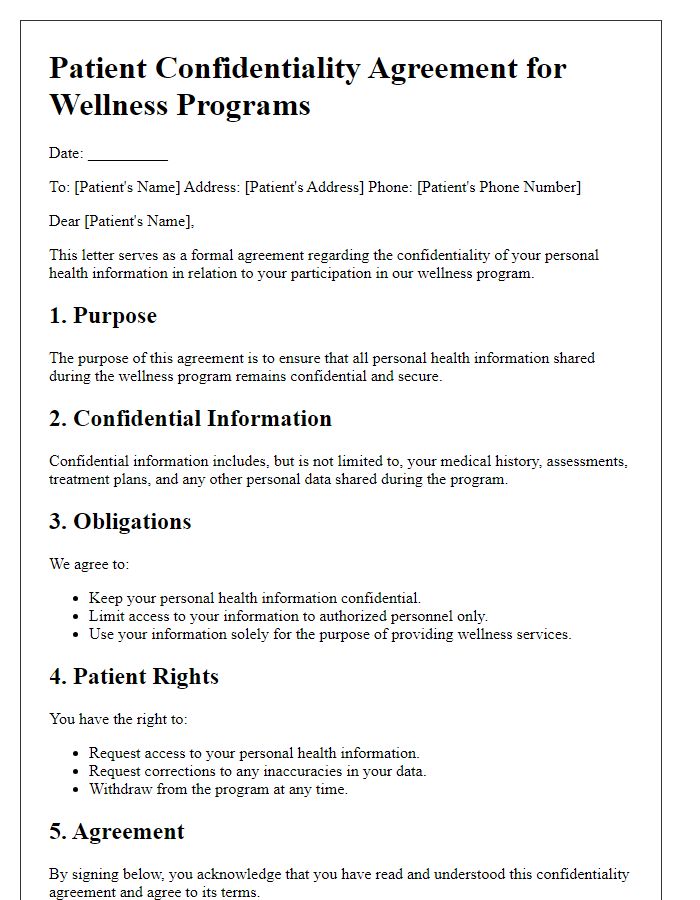
Letter Template For Patient Confidentiality Agreement Samples
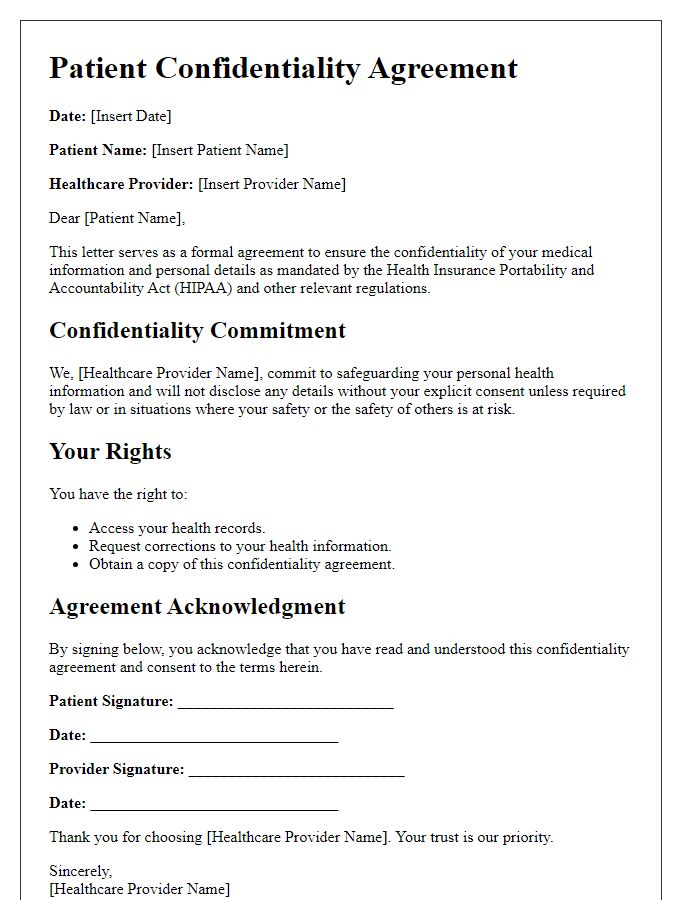
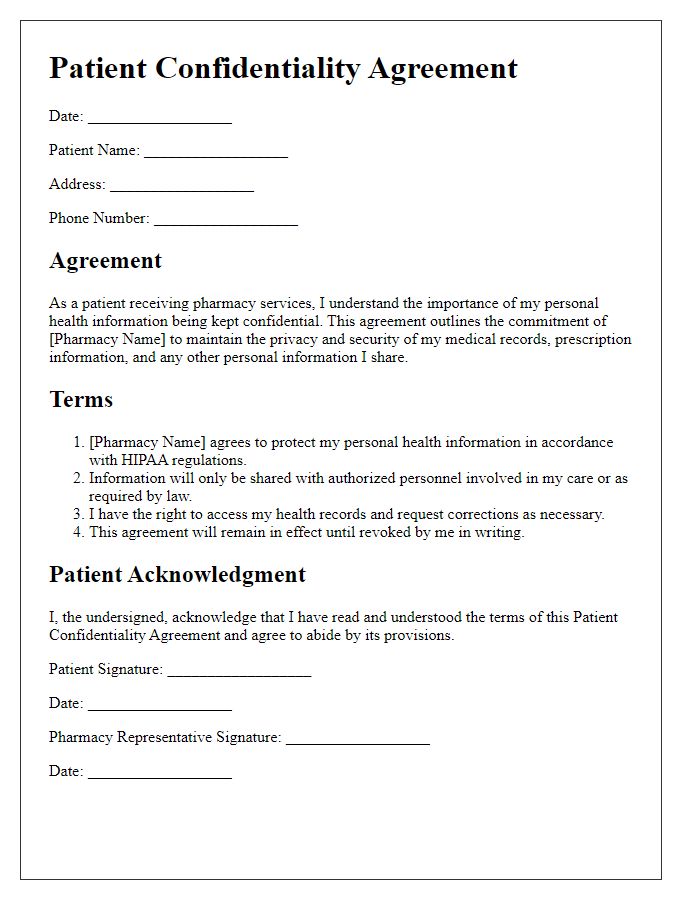
Letter template of patient confidentiality agreement for healthcare providers.
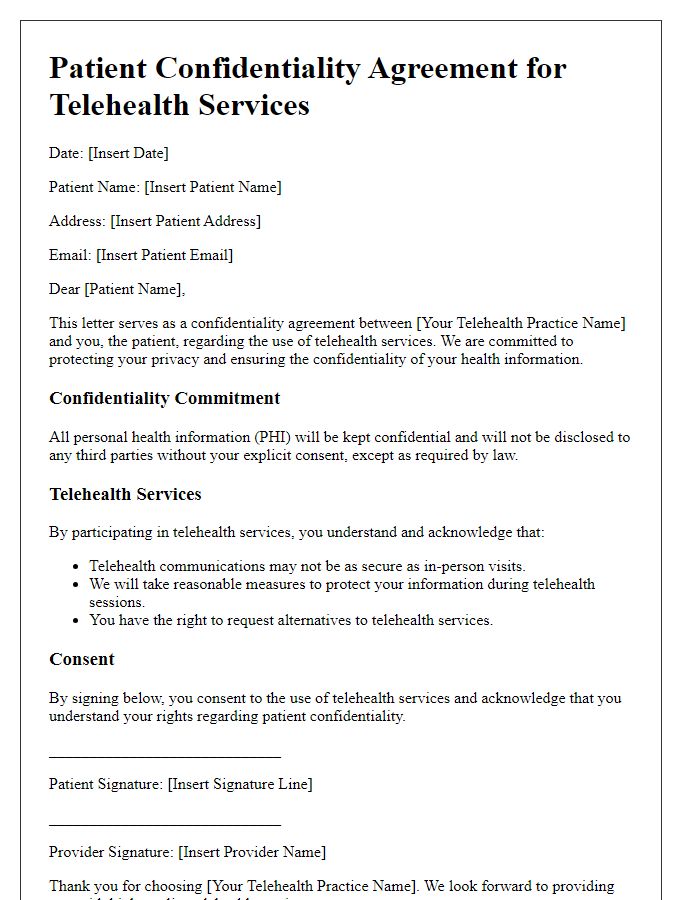
Letter template of patient confidentiality agreement for telehealth services.
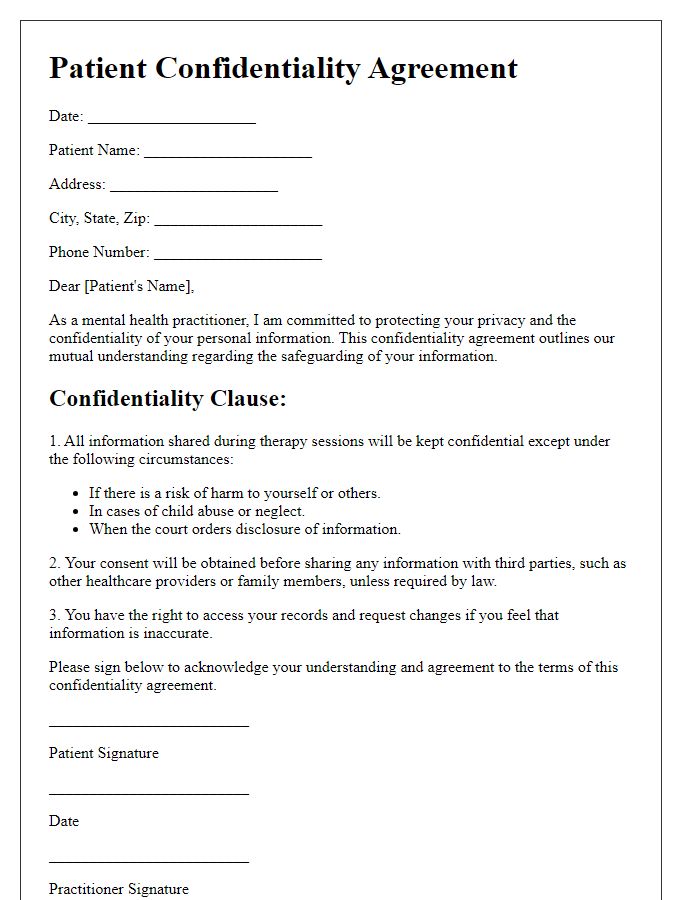
Letter template of patient confidentiality agreement for mental health practitioners.
Letter template of patient confidentiality agreement for dental practices.
Letter template of patient confidentiality agreement for physical therapy clinics.
Letter template of patient confidentiality agreement for individual practitioners.
Letter template of patient confidentiality agreement for hospital settings.
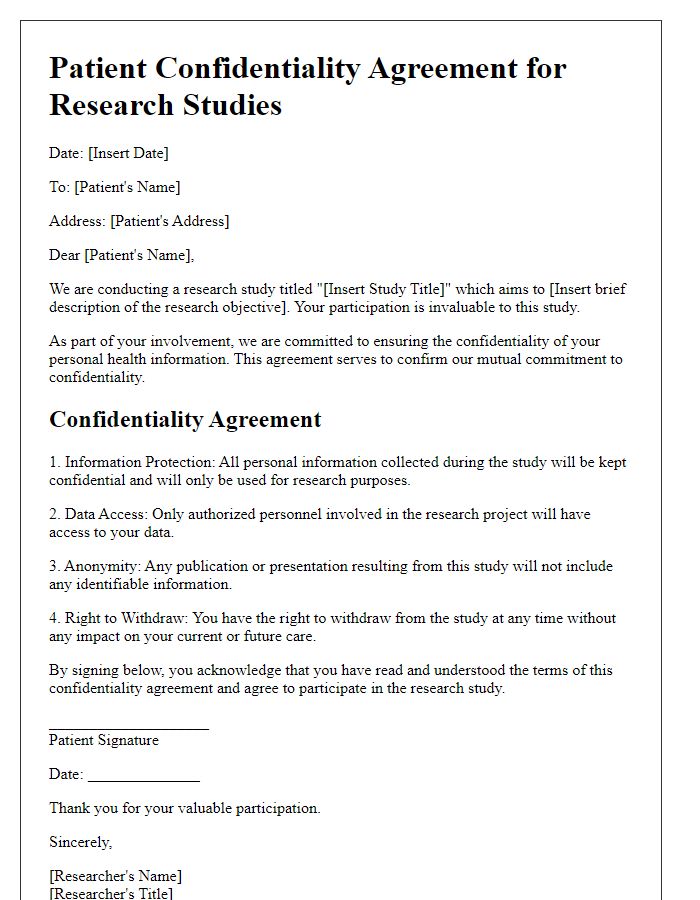
Letter template of patient confidentiality agreement for research studies.


Comments