Managing pain can be a challenging journey, but having a clear plan can make all the difference. In this article, we'll explore essential components of an effective pain management strategy tailored to individual needs. We'll cover various approaches, from medication options to lifestyle changes that promote overall well-being. So, if you're ready to take control of your pain and improve your quality of life, read on to discover more!
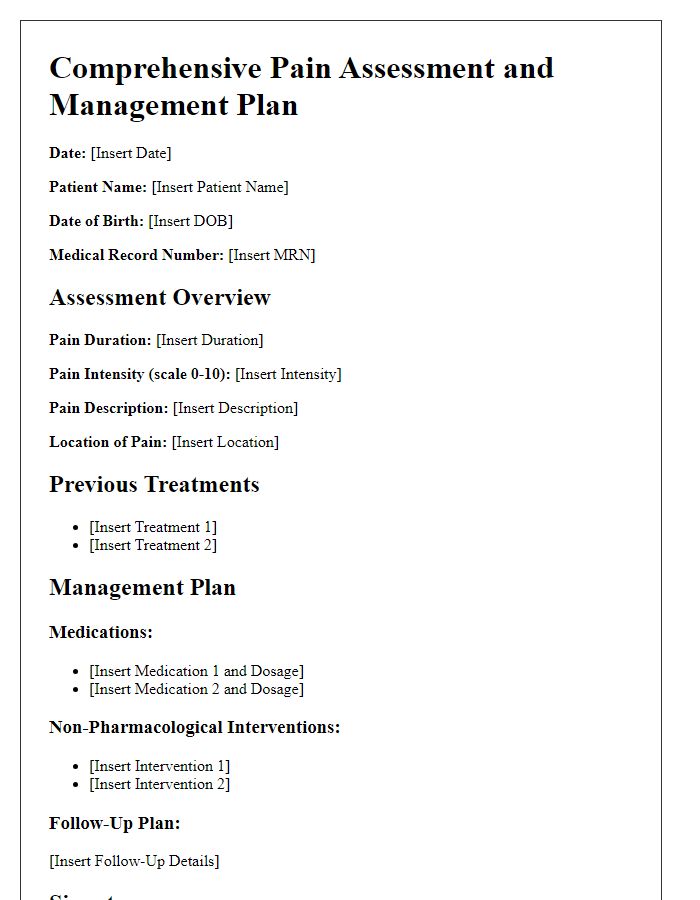
Patient Identification Information
Patient identification information, including full name, date of birth, and medical record number, is crucial for effective pain management planning. Accurate demographic details, such as contact information and address, ensure streamlined communication between healthcare providers and the patient. Additionally, clinical information like primary diagnosis, pain assessment scores (measured on a scale of 0-10), and medication allergies plays a vital role in tailoring individual pain management strategies. Furthermore, understanding the patient's medical history, including previous treatments and responses to pain interventions, is essential for creating an effective and personalized pain management plan.
Comprehensive Pain Assessment
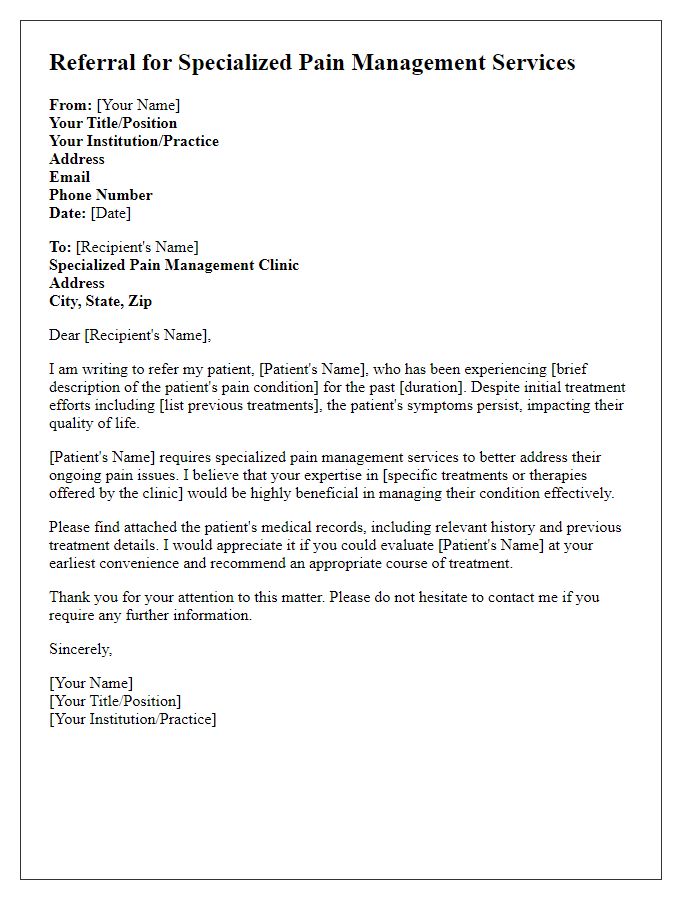
Comprehensive pain assessment involves gathering detailed information about an individual's pain experience, which includes the pain's intensity, duration, and characteristics. Tools such as the Visual Analog Scale (VAS), rating pain from 0 (no pain) to 10 (worst pain imaginable), provide quantifiable measures. Specific locations of pain, often marked on diagrams, help identify patterns and potential underlying causes. Identifying pain triggers and alleviating factors, such as certain activities, medications, or environmental conditions, adds context. Psychological assessments also consider the emotional impact of pain, including anxiety and depression levels. A thorough review of medical history, including surgeries and previous treatments, alongside current medication regimens, ensures a holistic understanding. Collaboration with multidisciplinary teams, including physical therapists and psychologists, can enhance management strategies tailored to individual patient needs.
Personalized Treatment Goals
A personalized pain management plan focuses on identifying specific treatment goals tailored to the unique needs of the patient. Comprehensive assessments highlight factors such as pain intensity (measured on a scale from 0 to 10), location (e.g., lower back, knee), and duration (acute or chronic). In addition, the plan includes strategies to improve daily functioning, enhancing quality of life, and minimizing reliance on medication, like opioids. Supportive therapies, such as physical therapy exercises or cognitive behavioral therapy, may be introduced to address both physical and psychological aspects of pain. Regular follow-ups (scheduled every 4-6 weeks) assess progress, allowing for adjustments in treatment approaches to ensure effectiveness and patient satisfaction. Education regarding self-management techniques plays a crucial role in empowering patients toward achieving their objectives.
Medication and Dosage Plan
Effective pain management is essential for enhancing the quality of life, particularly for patients suffering from chronic conditions like arthritis or post-surgical recovery. An individualized medication plan typically involves Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), such as Ibuprofen (up to 800 mg every 8 hours) or Acetaminophen (maximum 3000 mg per day), to reduce inflammation and alleviate discomfort. Opioids, like Oxycodone (prescribed in doses varying from 5 mg to 15 mg every 4 to 6 hours as needed for severe pain), may be considered for acute or severe pain management, though careful monitoring for dependency or side effects is crucial. Adjunctive therapies, including Gabapentin (starting at 300 mg at bedtime, increasing as tolerated), can help manage neuropathic pain. Regular follow-up appointments should be scheduled, ideally every 4 to 6 weeks, to assess efficacy, adjust dosages, and monitor for potential adverse drug reactions.
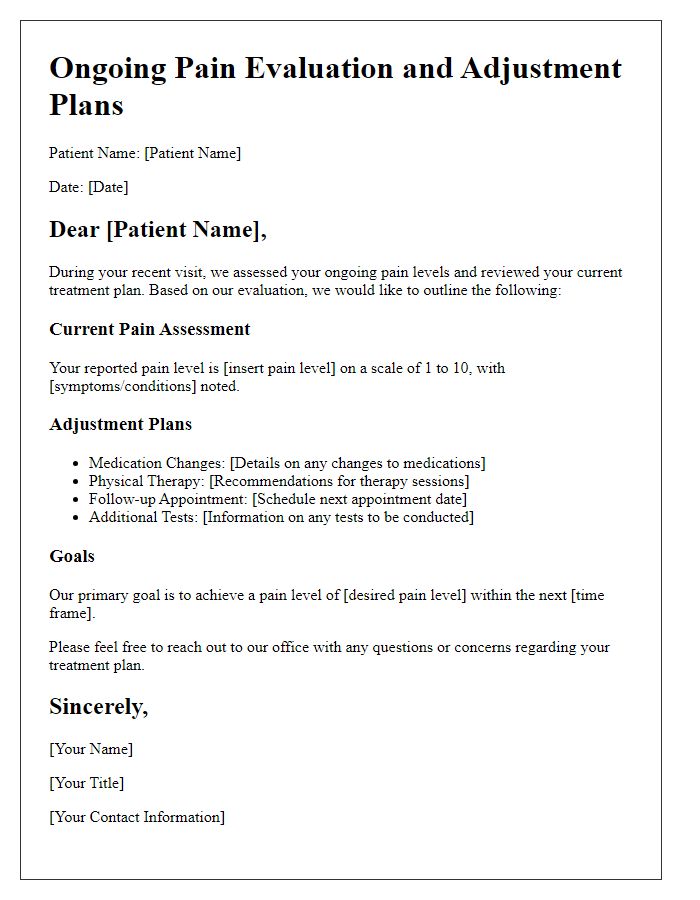
Monitoring and Follow-up Schedule
A comprehensive pain management plan requires careful monitoring and follow-up to ensure the effectiveness of treatments. Regular assessments, typically scheduled every four to six weeks, are crucial to evaluate the patient's pain levels (using scales like the Numeric Rating Scale from 0 to 10), medication efficacy, and any side effects experienced. These appointments also provide an opportunity to adjust medications or therapy modalities, including physical therapy sessions or cognitive behavioral therapy techniques tailored to the individual's specific conditions, such as osteoarthritis or fibromyalgia. Documentation of progress, including pain diaries and functional assessments, plays a vital role in this process, allowing healthcare providers to make informed decisions based on the patient's responses. Emphasis on open communication about pain experiences fosters a collaborative approach between the patient and healthcare team, enhancing overall pain management outcomes.
Letter Template For Patient Pain Management Plan Samples
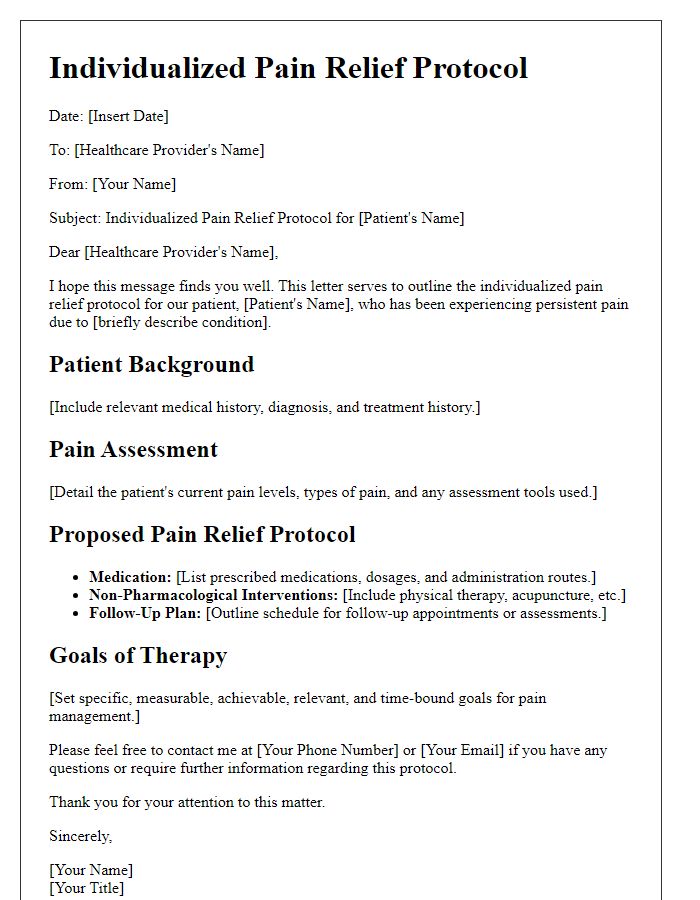
Letter template of individualized pain relief protocols for healthcare providers
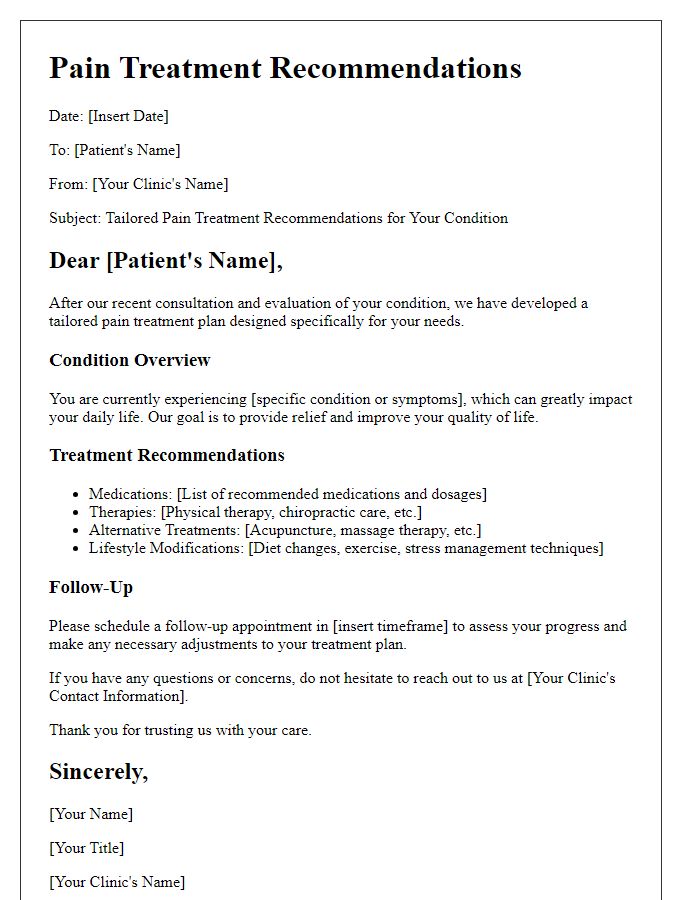
Letter template of tailored pain treatment recommendations for specific conditions
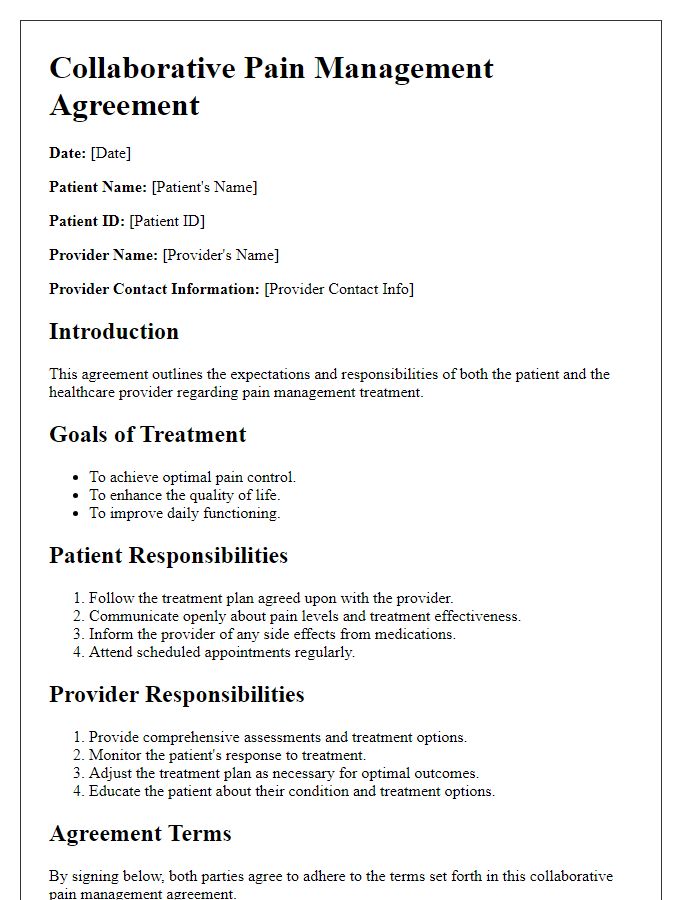
Letter template of collaborative pain management agreements between practitioners and patients
Letter template of educational resources for patients on pain management options
Letter template of follow-up strategies for effective pain control solutions


Comments