When it comes time to transition from hospital care to home, clear discharge instructions are crucial for a smooth recovery. These guidelines serve as your roadmap, outlining medications, follow-up appointments, and self-care strategies to ensure your healing process remains on track. Understanding your discharge instructions can seem overwhelming, but with a little guidance, you can navigate this important step with confidence. Ready to learn how to make the most of your hospital discharge? Read more!
Patient Information and Identification
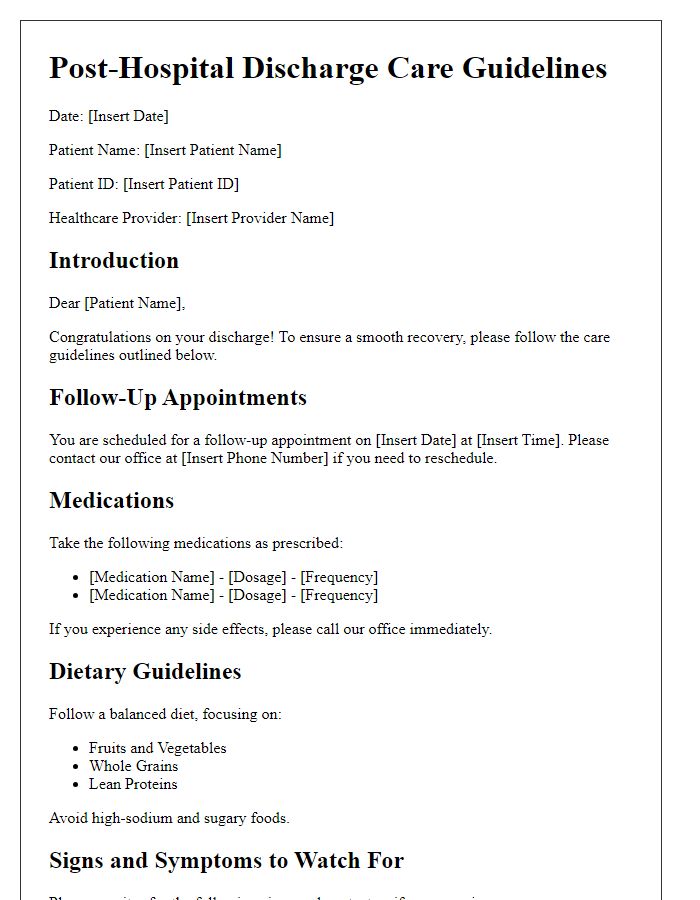
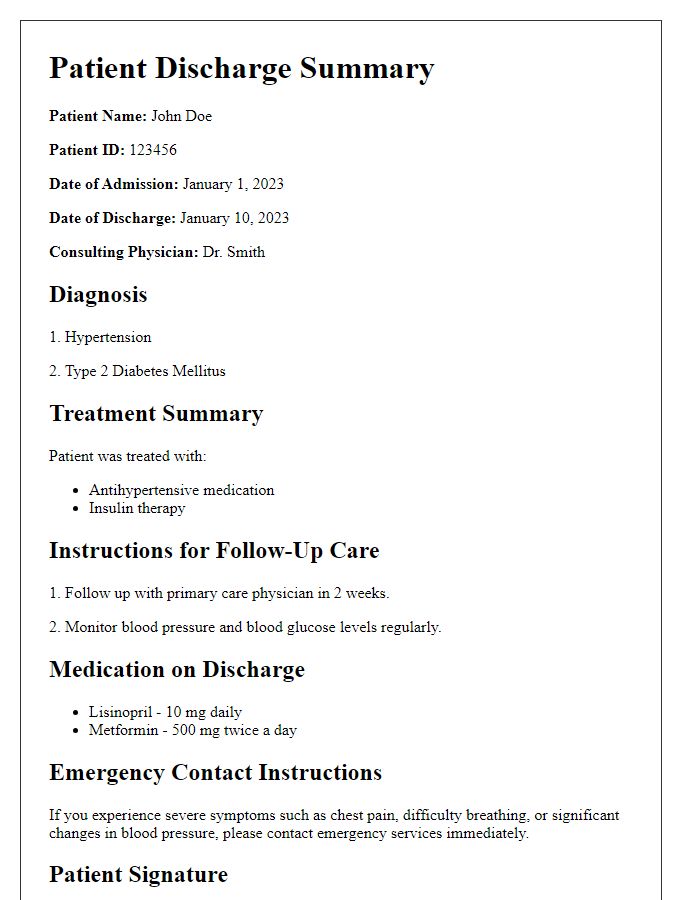
Patient discharge instructions are critical for ensuring a smooth transition from hospital to home care. Each set of instructions typically includes vital patient information such as full name (e.g., John Smith), date of birth (e.g., January 15, 1980), hospital identification number (e.g., 123456), and primary diagnosis (e.g., pneumonia). Additional details may encompass the attending physician's name (Dr. Jane Doe), discharge date (April 1, 2023), and follow-up appointment time (April 15, 2023, at 10:00 AM). Contact information for the hospital (e.g., 123 Main St, Springfield), as well as a list of prescribed medications with dosages (e.g., Amoxicillin 500mg three times daily), would also be included to ensure the patient understands their ongoing care regimen.
Discharge Diagnosis and Condition
Discharge diagnosis signifies the medical condition leading to a patient's hospitalization, such as congestive heart failure, pneumonia, or a surgical procedure. Understanding the specific diagnosis helps ensure that proper post-discharge care is followed. The condition refers to the patient's status at the time of discharge, potentially including details such as stability, ongoing symptoms, or limitations in activity. For example, a specific diagnosis like Type 2 Diabetes may come with recommendations for ongoing blood sugar monitoring and dietary adjustments. Similarly, a patient recovering from knee surgery might be instructed about mobility restrictions and rehabilitation exercises. Documentation should include key details about medications prescribed, follow-up appointments at local clinics or the hospital, and warning signs that would necessitate immediate medical attention.
Medication Instructions and Schedule
Medication instructions and schedule are critical for post-discharge recovery from a hospital stay. Patients need clear guidelines on prescribed medications, including names, dosages, and frequency of administration. For example, if a patient is prescribed amoxicillin (500 mg), it should be taken every 8 hours for 7 days to effectively treat bacterial infections. Additionally, it's essential to identify potential side effects, such as dizziness or nausea, allowing patients to monitor their responses. Timely medication should be tracked; using a pill organizer or setting reminders on mobile devices can enhance compliance. Regular follow-up appointments with healthcare providers, typically within one to two weeks post-discharge, ensure that the efficacy of the medications is evaluated and necessary adjustments are made for optimal health outcomes.
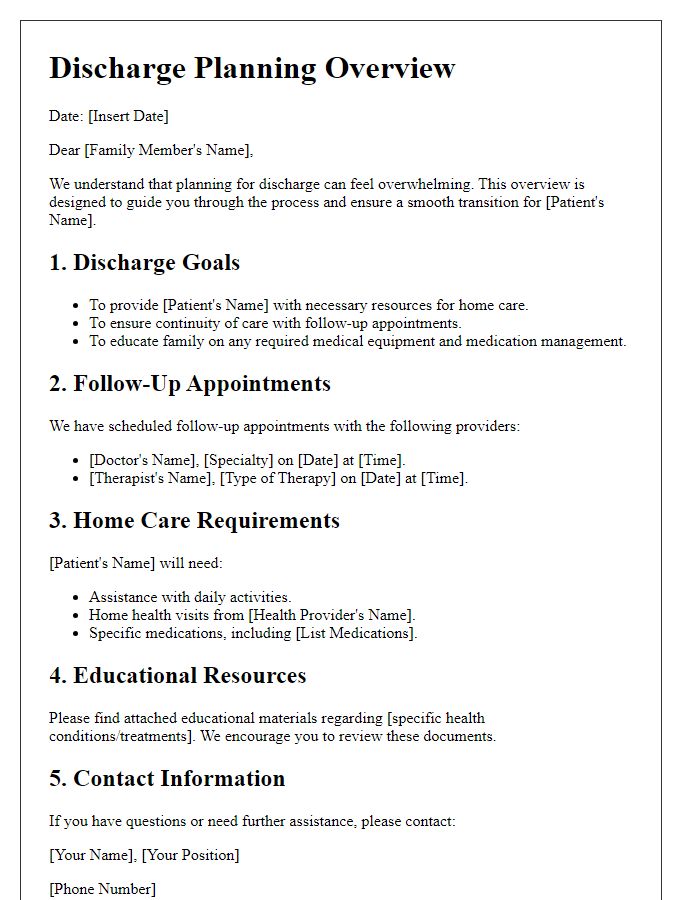
Follow-up Appointments and Contacts
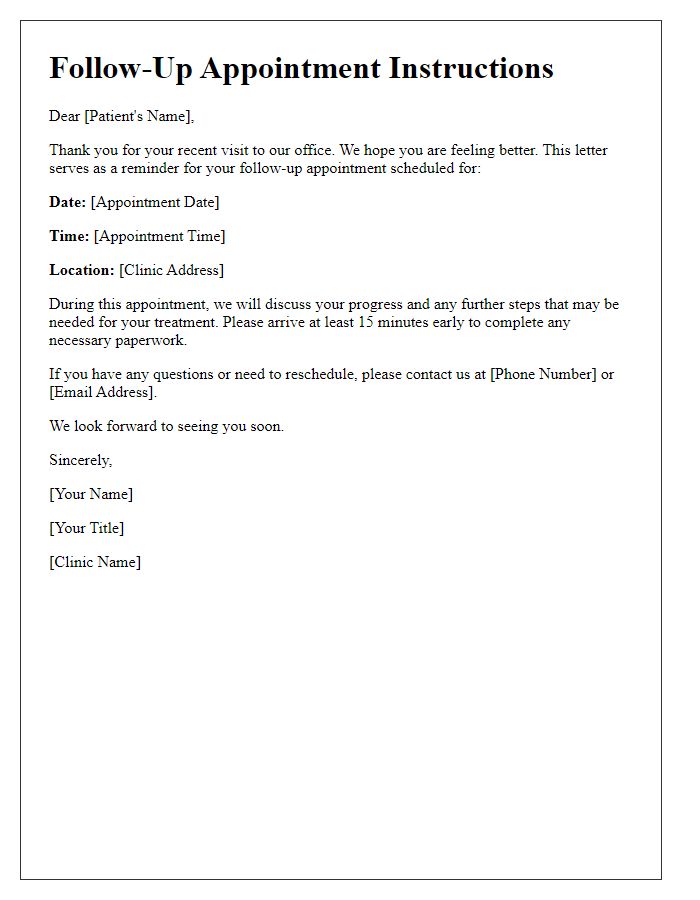
Hospital discharge instructions should include detailed follow-up appointments and vital contact information to ensure continuity of care. Patients must be aware of their next appointment scheduled with their primary care physician within seven days post-discharge for evaluation of recovery progress. Additionally, specialists involved in the patient's care (such as cardiologists or endocrinologists) may require follow-up within two weeks. Important contact numbers must be provided, including the hospital's outpatient clinic number (555-123-4567) for scheduling concerns and urgent care facility (555-765-4321) for immediate questions related to health issues. Emergency contact, such as the local emergency room at City Hospital (which operates 24/7), is crucial for acute situations. Ensure that patients understand the importance of adhering to these appointments for optimal recovery and ongoing health management.
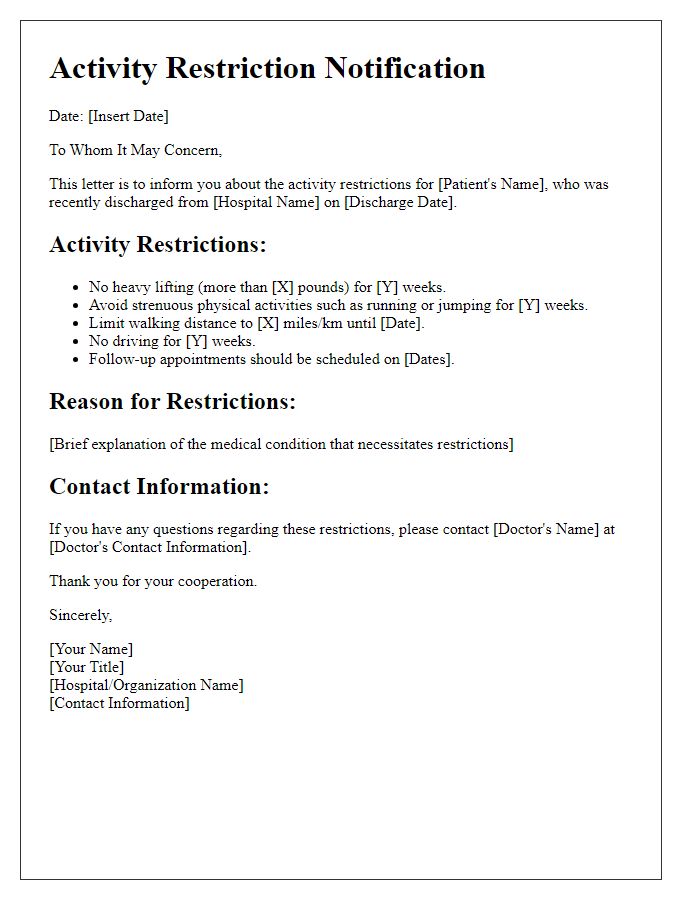
Activity and Dietary Guidelines
Hospital discharge instructions are critical for ensuring a smooth transition from a clinical environment to home recovery. Activity guidelines emphasize gradual resumption of normal activities based on individual recovery progress, typically starting with light walking after surgery (within 48 hours or as advised by a physician). It's crucial to avoid heavy lifting (more than 10 pounds) and strenuous exercise for at least 4 to 6 weeks, allowing the body adequate time to heal. Dietary guidelines often focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, promoting healing and supporting immune function. Specific recommendations may include increased fluid intake (aim for 8 cups per day) and limiting processed sugars and saturated fats. Monitoring for symptoms such as elevated heart rate, unusual pain, or severe fatigue during activity is essential for assessing recovery progress and should prompt immediate medical consultation.



Comments