When it comes to ensuring a smooth transition from hospital to home, a well-crafted patient discharge summary is essential. This communication not only summarizes the patient's care journey but also outlines important next steps for continued recovery. By providing clear instructions and important health information, you empower patients to take charge of their health after discharge. Curious about how to create an effective discharge summary? Read on to discover our comprehensive template!
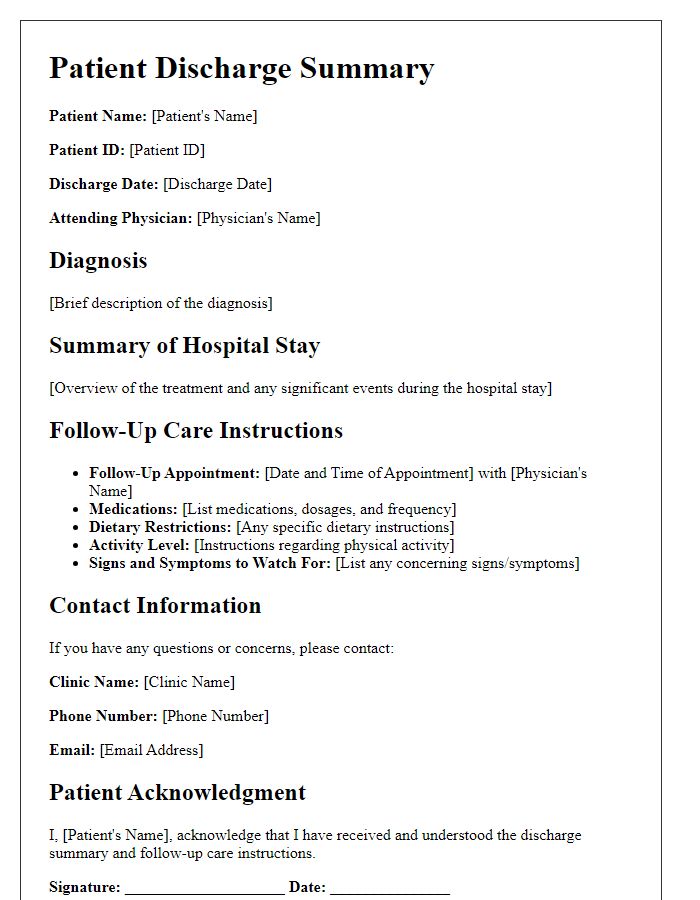
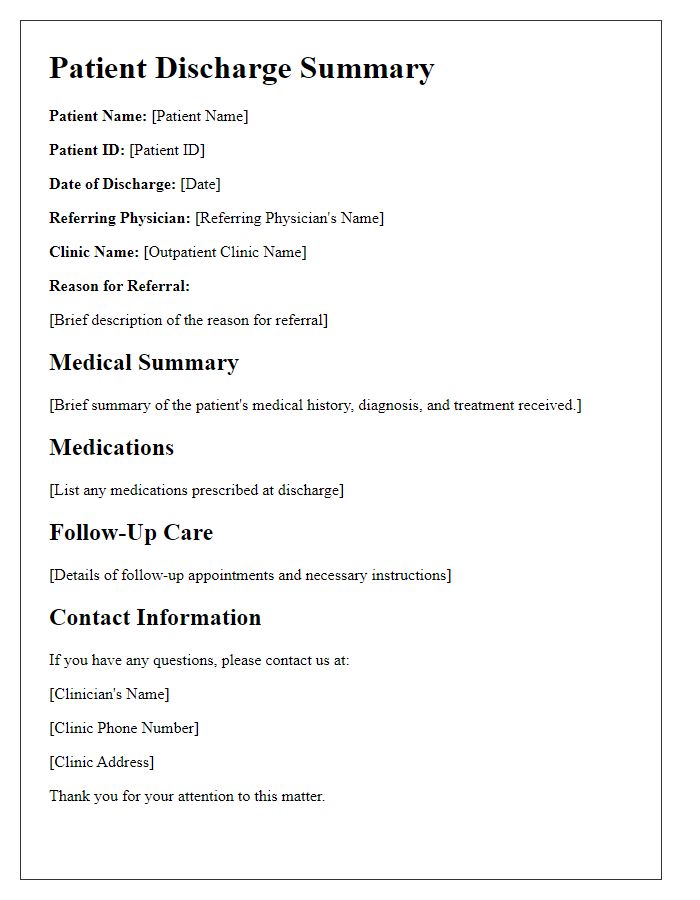
Patient Identification Information
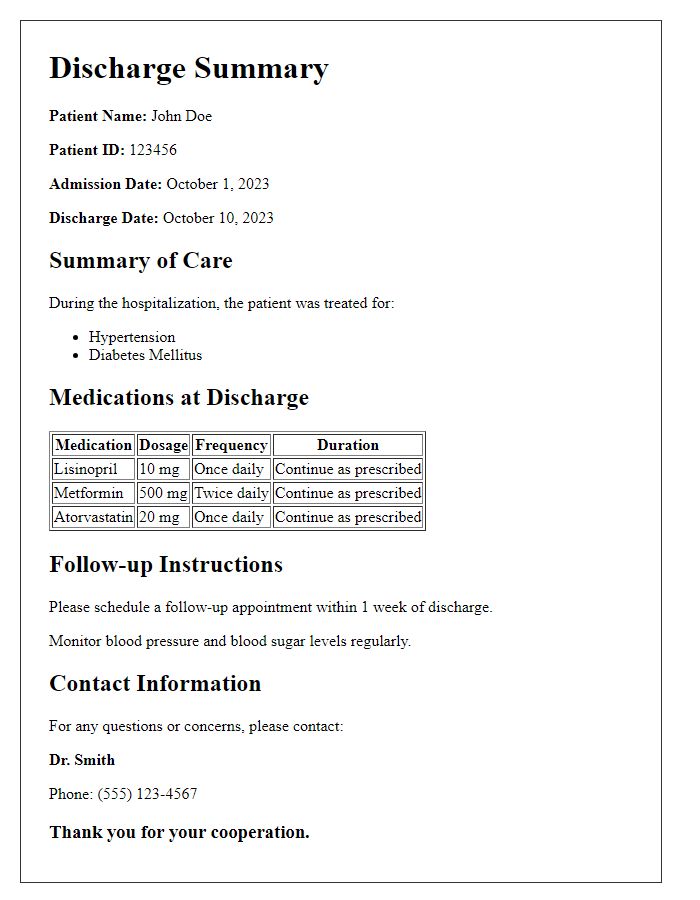
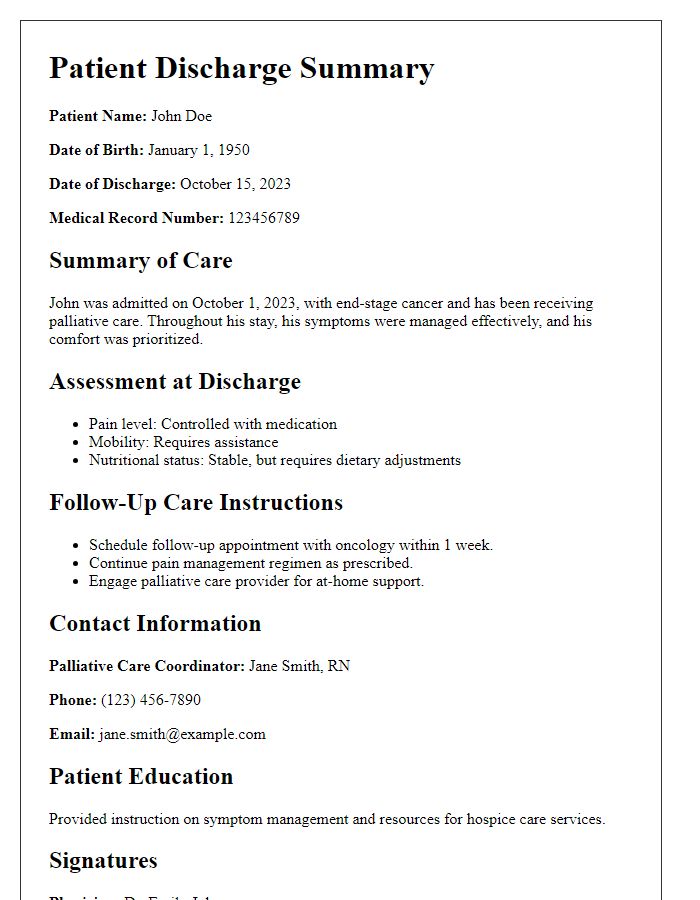
The patient identification information includes critical details that ensure proper documentation and continuity of care. The patient's full name, such as Emily Johnson, along with the date of birth, for instance, August 15, 1985, is essential for accurate identification. The medical record number, say MRN 123456789, serves as a unique identifier within the healthcare system. Additionally, the admission date, for example, October 10, 2023, and discharge date, such as October 17, 2023, provide context for the patient's hospital stay duration. Contact information, including the patient's phone number and address in Springfield, IL, ensures follow-up communication is effective. The insurance details, such as Blue Cross Blue Shield policy number 987654321, facilitate billing processes and coverage verification. These components create a comprehensive patient identification profile that is vital for the discharge summary.
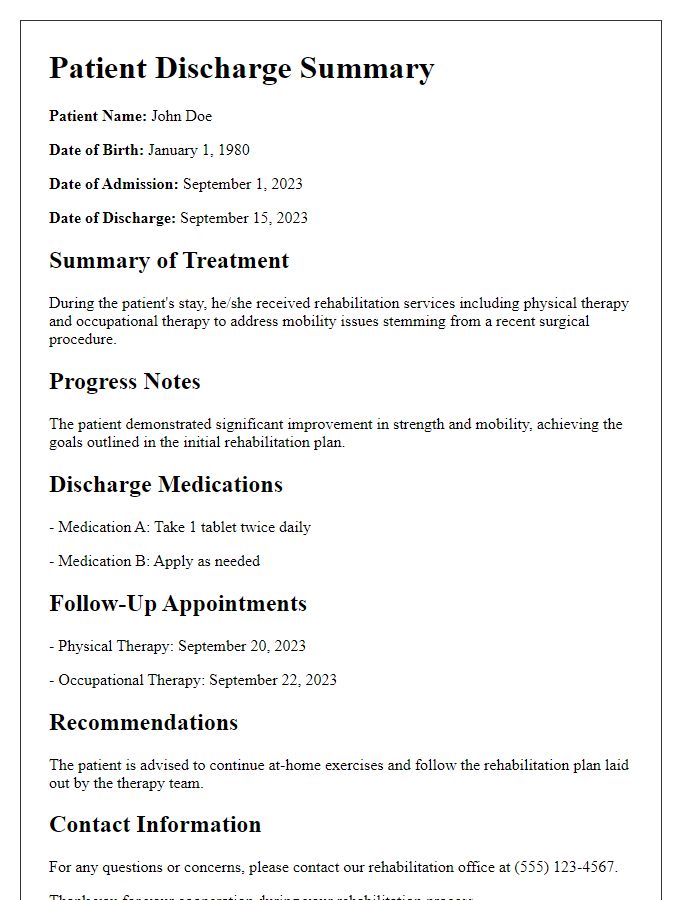
Summary of Hospital Stay
A patient discharge summary concisely outlines critical information following a hospital stay. The summary typically includes patient demographics such as name, age, and hospital identification number. It details the admission date, discharge date, diagnosis (including any primary and secondary conditions), and key treatments received. Notable procedures performed, such as surgeries or diagnostic tests, are also documented alongside results. Medication prescriptions upon discharge must indicate dosages and administration routes. Follow-up appointments (with specific dates and involved healthcare providers) ensure continuity of care. Additionally, any patient education materials, lifestyle recommendations, or warning signs to monitor post-discharge should be included for comprehensive patient understanding.
Diagnosis and Treatment Provided
Patient discharge summaries are critical for ensuring continuity of care and must include essential information regarding the patient's diagnosis and treatment. The primary diagnosis, such as pneumonia or heart failure, should be clearly stated, along with any relevant diagnostic tests, like chest X-rays or blood tests, performed during hospitalization. Details about treatments provided, including medication regimens like antibiotics or anticoagulants, surgical interventions, and therapies (e.g., physical or occupational therapy), should be comprehensively documented. It is vital to note any changes in the patient's condition throughout their stay, the treatment response, and any follow-up appointments scheduled, such as those at local clinics or specialist offices, ensuring the patient's ongoing recovery and health management.
Follow-up Instructions and Medications
After discharge from the hospital, patients must adhere to follow-up instructions for optimal recovery. Follow-up appointments should take place within one week, scheduled with primary care providers (PCPs) or specialists, depending on the condition treated. Medications prescribed, such as antibiotics for infection or pain relief like ibuprofen, must be taken as directed--dosage, frequency, and duration should be clearly outlined. Patients should monitor for side effects, including nausea or dizziness, and report any concerns to their healthcare team promptly. Furthermore, lifestyle adjustments, including increased hydration and dietary changes, are crucial for recovery, especially for those who underwent surgery or experienced chronic illnesses. Regular communication with healthcare professionals via designated hotlines or patient portals is encouraged to ensure a smooth transition from hospital to home care.
Contact Information for Healthcare Provider
When transitioning from hospital to home, clear communication is essential for patient safety and continuity of care. The healthcare provider's contact information should detail the name of the facility, such as St. Mary's Hospital, plus the names and qualifications of doctors or nurses involved in care, including the attending physician, Dr. John Smith, a board-certified internal medicine specialist. Additionally, provide a direct phone number, like (555) 123-4567, and an email address, such as info@stmaryshospital.com, to facilitate follow-up questions or concerns. Include office hours, typically Monday through Friday, 8 AM to 5 PM, to inform patients when they can seek assistance. Emergency contact options, like local urgent care or emergency services (911), should also be noted to reinforce access to urgent care.
Letter Template For Patient Discharge Summary Communication Samples
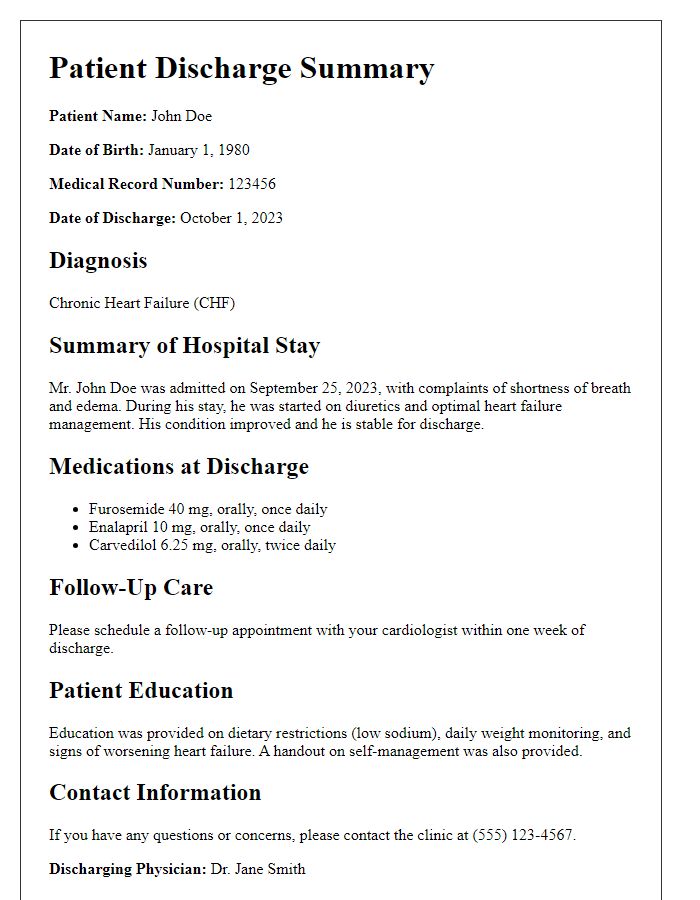
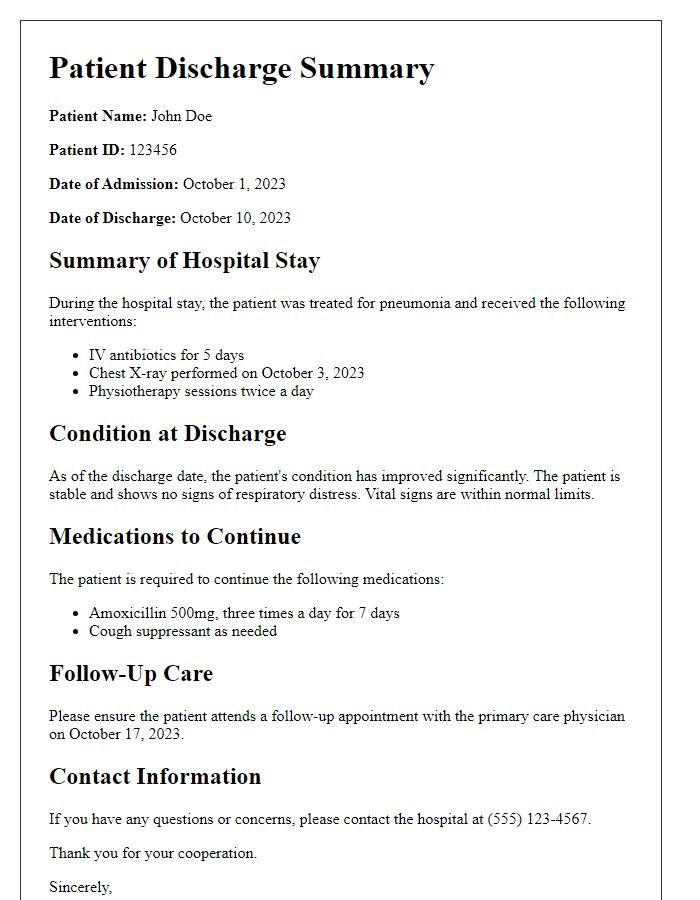
Letter template of patient discharge summary for follow-up care instructions.
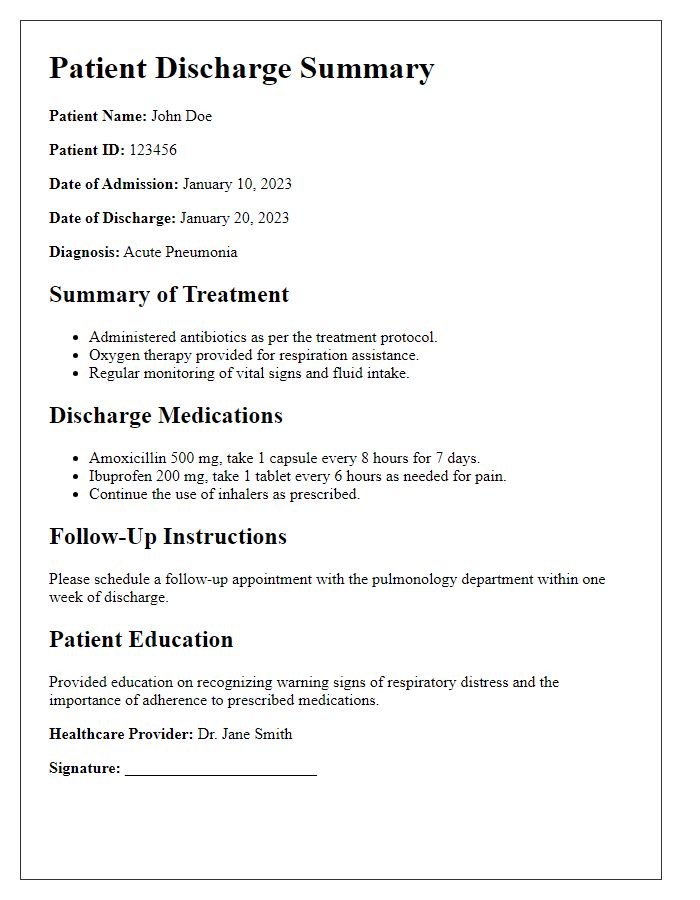
Letter template of patient discharge summary for rehabilitation services.
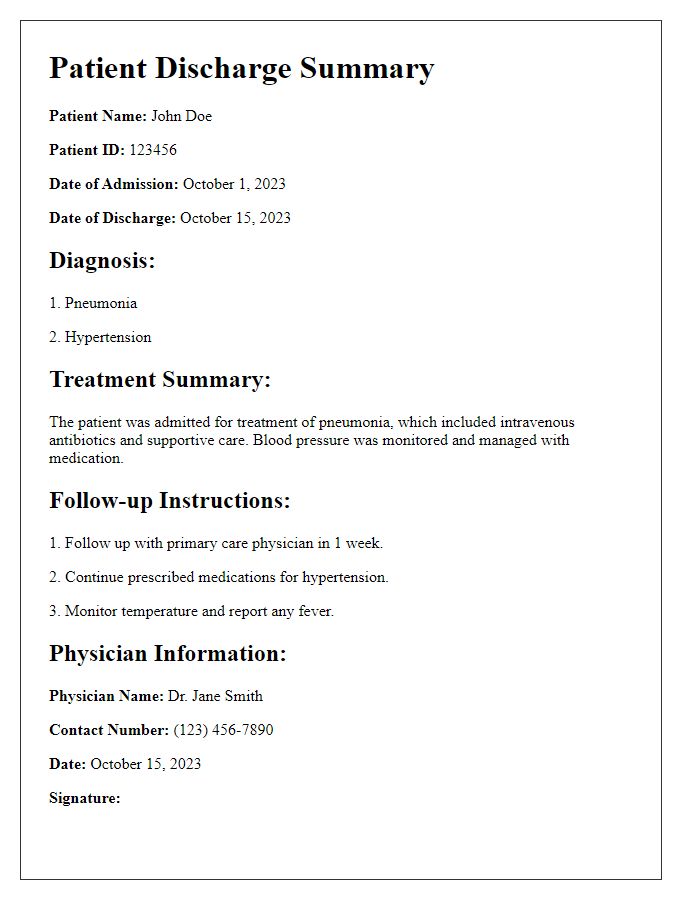
Letter template of patient discharge summary for outpatient clinic referral.
Letter template of patient discharge summary for chronic condition management.



Comments