Are you curious about how to effectively assess your cardiovascular risk? Understanding your cardiovascular health is crucial, and knowing the right factors can make a significant difference in prevention and management. In this article, we'll explore the essential components of a cardiovascular risk factor assessment, from cholesterol levels to lifestyle habits. So, let's dive in and discover what you need to know to take charge of your heart health!
Patient Information Collection
Cardiovascular risk factor assessment focuses on identifying specific health metrics and lifestyle choices that contribute to heart disease risk. Blood pressure readings (normal: below 120/80 mmHg) help evaluate hypertension's role, while cholesterol levels (preferably total below 200 mg/dL) indicate lipid profile and atherosclerosis risk. Body Mass Index (BMI), calculated from weight and height measurements, determines obesity status (BMI over 30 indicates high risk). Smoking status significantly impacts cardiovascular health, with smokers facing double the risk of heart disease compared to non-smokers. Physical activity frequency and dietary habits, including saturated fat intake (should be less than 10% of total calories), are crucial for assessing lifestyle factors. Family history of cardiovascular diseases, particularly cases before age 55 for males and 65 for females, strengthens the likelihood of individual risk. Age and gender additionally play critical roles, with age over 45 for men and 55 for women being significant risk indicators. Comprehensive assessment ensures personalized treatment plans and preventive strategies in clinical practice.
Medical History Review
Cardiovascular risk factor assessment requires a thorough review of individual medical history, focusing on key health indicators such as hypertension (high blood pressure over 130/80 mmHg), diabetes (elevated blood glucose levels above 126 mg/dL), and hyperlipidemia (elevated cholesterol levels exceeding 240 mg/dL). Additional consideration should be given to lifestyle factors including smoking status (current, former, or never), physical activity levels (recommendation of 150 minutes of moderate exercise weekly), and body mass index (BMI, a measure of body fat based on height and weight). Family medical history also plays a crucial role, particularly the presence of premature cardiovascular disease in first-degree relatives before age 55 for men and 65 for women. All these elements together provide valuable insights into an individual's cardiovascular health and potential risks.
Lifestyle and Dietary Habits Analysis
Cardiovascular risk factor assessments highlight the significance of lifestyle and dietary habits in heart health. Regular physical activity, such as brisk walking (preferably 150 minutes weekly), significantly reduces the risk of heart diseases. Key dietary elements include the intake of saturated fats, trans fats, and high-sodium foods, all common in processed foods, which can lead to hypertension. Nutritionists recommend a diet rich in fruits, vegetables, whole grains, and fatty fish, contributing omega-3 fatty acids for better heart function. Monitoring body mass index (BMI) rates, ideally between 18.5 and 24.9, plays a crucial role in evaluating obesity levels that correlate with increased cardiovascular risks. Furthermore, alcohol consumption should be moderated, ideally limiting intake to one drink per day for women and two for men. Enhancing awareness of stress management techniques is also vital, as chronic stress can lead to unhealthy coping mechanisms, such as overeating or smoking, further elevating cardiovascular risk.
Physical Examination and Measurements
A comprehensive cardiovascular risk factor assessment requires careful physical examination and precise measurements to evaluate overall health. Blood pressure readings (e.g., 120/80 mmHg as normal) reveal vital information about heart health, while body mass index (BMI) calculations help assess obesity levels (a BMI over 30 indicates obesity). Waist circumference measurements (greater than 94 cm for men and 80 cm for women) highlight central obesity, a significant risk factor. Cholesterol levels, particularly low-density lipoprotein (LDL) and high-density lipoprotein (HDL), play crucial roles; optimal LDL levels should be below 100 mg/dL, and HDL should be above 60 mg/dL for optimal cardiovascular health. Additionally, assessing resting heart rate (normal range 60-100 beats per minute) can provide insights into cardiovascular fitness. Smoking status, dietary habits, and physical activity levels are also taken into account, with sedentary lifestyles contributing to increased risk. Such meticulous evaluations help in identifying individuals at high risk for cardiovascular diseases and guide appropriate interventions.
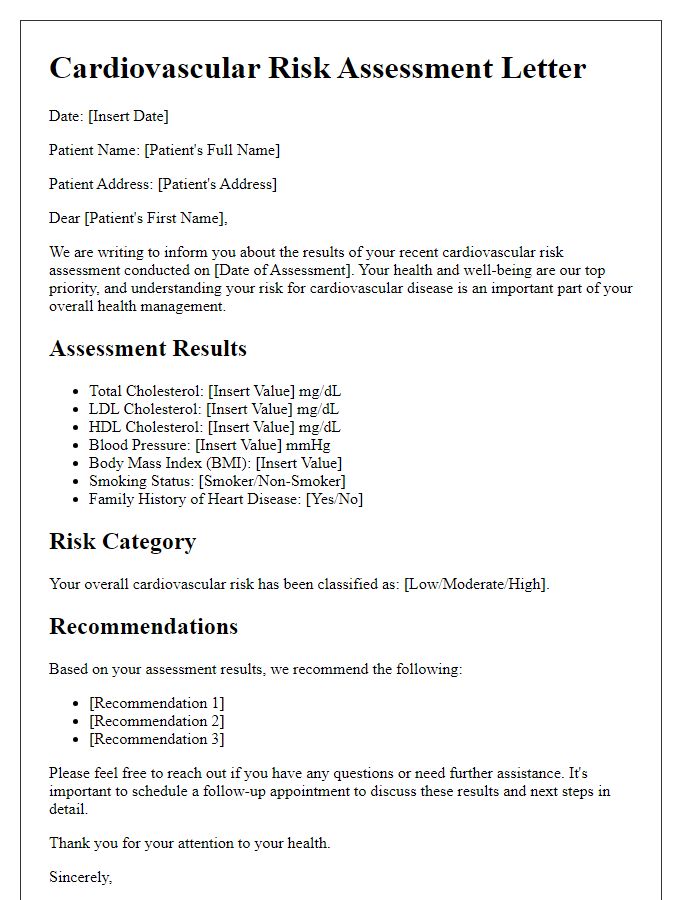
Assessment Results and Recommendations
Cardiovascular risk factor assessment involves evaluating parameters such as blood pressure, cholesterol levels, body mass index (BMI), and lifestyle habits like diet and exercise frequency to determine an individual's risk for heart disease. Elevated blood pressure, above 140/90 mmHg, significantly increases risk, as does a high LDL cholesterol level (greater than 160 mg/dL). A BMI over 30 categorizes an individual as obese, heightening the risk of vascular complications. Regular physical activity, defined as at least 150 minutes of moderate exercise weekly, is critical for reducing these risks. In addition, dietary patterns characterized by high saturated fats and low fiber intake contribute negatively to cardiovascular health. Recommendations may include lifestyle modifications such as dietary adjustments to include more fruits and vegetables, regular cardiovascular exercise, and monitoring of blood pressure and cholesterol levels to manage and mitigate risks effectively.
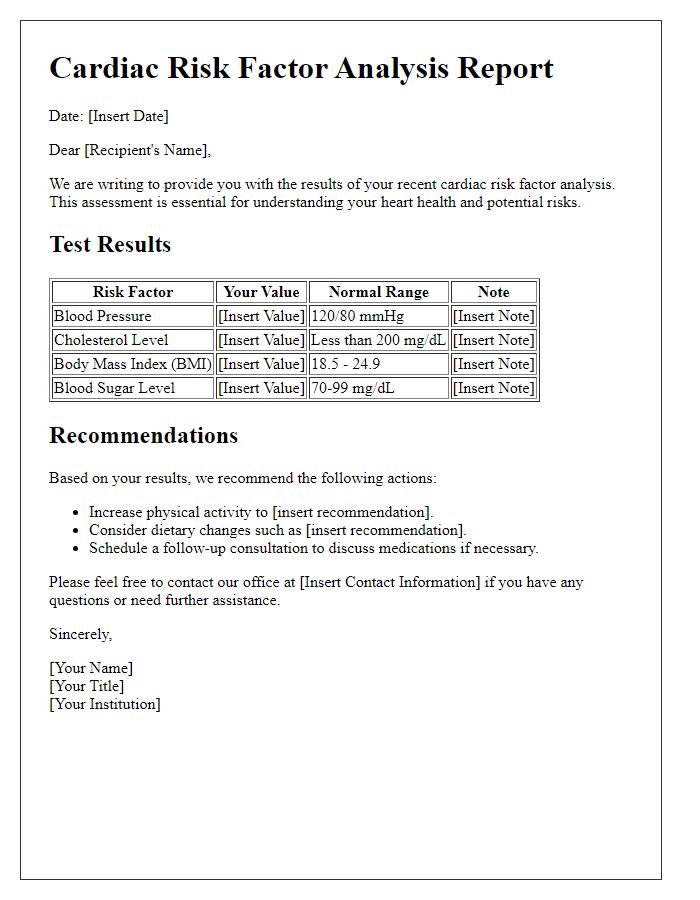
Letter Template For Cardiovascular Risk Factor Assessment Samples
Letter template of cardiovascular screening notification for community members
Letter template of cholesterol and blood pressure risk assessment for adults



Comments