Creating a pain management plan can feel overwhelming, but it's a crucial step toward reclaiming your comfort and well-being. In this guide, we'll walk you through the essential components of an effective pain management strategy that caters to your unique needs. From understanding your pain triggers to exploring various treatment options, we'll help demystify the process and empower you to take charge of your health. Ready to take the next step? Read on to discover more about developing your personalized pain management plan!

Patient Identification and Personal Information
Patient identification for a pain management plan involves compiling essential personal information, including full name, age, date of birth, and contact information such as phone number and email. Additionally, medical history details, including any previous diagnoses (like fibromyalgia or arthritis), previous treatments (such as physical therapy or medication), and current medications (like opioids or anti-inflammatories), are crucial. Understanding the patient's primary source of pain, its intensity (measured on a scale of 1 to 10), and location (specific body areas like lower back or knees) provides vital context. Furthermore, noting lifestyle elements such as occupation (sedentary or active) and any relevant family medical history aids in tailoring a personalized pain management strategy. This comprehensive approach ensures a holistic view of the patient's situation for effective treatment planning.
Comprehensive Pain Assessment
A comprehensive pain assessment is essential for developing an effective pain management plan tailored to individual needs. This assessment often includes evaluation methods like the Visual Analog Scale (VAS), allowing patients to quantify their pain on a scale from 0 to 10. Additionally, a review of the patient's medical history is crucial, focusing on previous diagnostic tests, treatments, and medication responses. Key factors such as pain duration, intensity fluctuations, and location (e.g., lower back, knee, or neck) contribute to understanding the pain's nature. Psychological components may also be assessed, using tools like the Brief Pain Inventory to measure how pain affects daily activities and emotional well-being. Incorporating input from multidisciplinary teams, including physiotherapy and psychology, provides a holistic view that enhances the pain management plan's effectiveness.
Treatment Goals and Objectives
Patients with chronic pain often require a comprehensive pain management plan to alleviate discomfort and improve quality of life. Treatment goals may include achieving a pain level reduction from a baseline score of 8 to a target score of 3 on a 10-point pain scale, enhancing daily functionality through physical therapy, and minimizing reliance on opioid medications by 50% within six months. Objectives can encompass implementing a multidisciplinary approach involving physicians, physical therapists, and psychologists, fostering regular exercise routines, and integrating mindfulness-based stress reduction techniques. Regular assessments, such as bi-weekly pain diaries and monthly follow-up appointments, can facilitate critical evaluations of progress and necessary adjustments to the management strategy. Emphasis on patient education regarding pain mechanisms and self-management strategies is essential for long-term success.
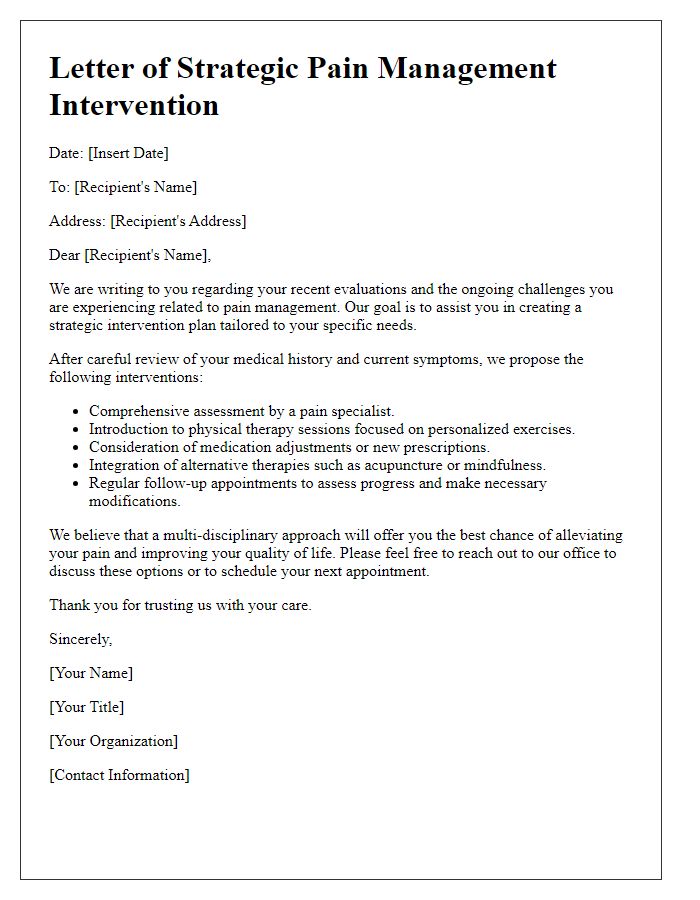
Proposed Treatment and Medication Plan
Chronic pain management relies on a comprehensive treatment and medication plan tailored to individual needs. Patients often receive non-steroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen or Acetaminophen for mild to moderate pain relief. For severe pain, opioids like Oxycodone may be prescribed, potentially coupled with adjunct therapies, including physical therapy (often conducted bi-weekly), cognitive-behavioral therapy (around eight sessions), or acupuncture treatments (approximately six sessions). Additionally, lifestyle modifications, including regular exercise, proper hydration, and a balanced diet rich in omega-3 fatty acids, can significantly enhance pain management outcomes. Follow-up consultations at designated clinics, typically scheduled every four to six weeks, are essential to monitor progress and adjust the treatment plan as required.
Monitoring and Follow-Up Schedule
Effective pain management requires a structured monitoring and follow-up schedule to assess progress and make necessary adjustments. Regular assessments every four weeks (or as clinically indicated) allow healthcare providers to evaluate pain levels, functional improvements, and medication effectiveness. Utilizing standardized pain scales, such as the Numeric Rating Scale (0-10), provides quantifiable data for ongoing treatment evaluation. The inclusion of multidisciplinary team meetings, involving pain specialists, physical therapists, and psychologists, fosters comprehensive care and ensures all aspects of the patient's well-being are addressed. Additionally, scheduling follow-up appointments at relevant intervals, such as every three months, can help identify potential side effects and medication interactions, ensuring patient safety and optimal therapeutic outcomes.



Comments