Are you feeling overwhelmed by managing your hypertension? You're not aloneâmany individuals struggle to navigate the complexities of blood pressure care. In this article, we'll break down essential strategies and tips to help you achieve better health outcomes while making the process more manageable. Join us as we explore the best practices for hypertension management and discover how simple lifestyle changes can make a significant difference.
Salutation and patient identification
Hypertension, also known as high blood pressure, poses significant health risks, often leading to serious conditions like heart disease and stroke. Accurate patient identification is crucial for effective management, ensuring that healthcare professionals have access to the patient's medical history and current medications. Various tools such as sphygmomanometers measure blood pressure, with a normal range typically being 120/80 mmHg, while readings above 130/80 mmHg indicate hypertension. Regular consultations are essential for monitoring symptoms and making necessary adjustments to treatment plans including lifestyle changes, medication, and dietary modifications. Chronic hypertension can also complicate other health issues, making comprehensive management critical.
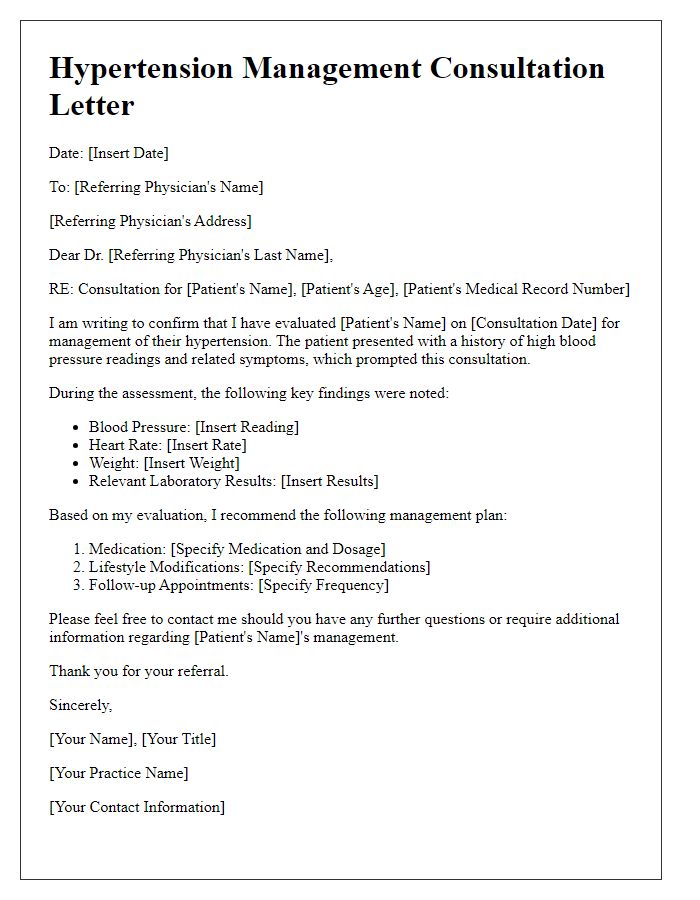
Purpose of the consultation
Hypertension management consultations focus on assessing blood pressure levels, understanding individual health conditions, and establishing effective treatment plans to reduce risks associated with high blood pressure. Typically, these consultations are aimed at patients diagnosed with hypertension, characterized by consistently elevated arterial pressure over 130/80 mmHg. The healthcare provider evaluates current medications, lifestyle factors--such as diet, exercise frequency, and stress levels--and collaborates with patients to implement lifestyle changes or adjust pharmacological therapy, potentially including medications like ACE inhibitors or diuretics. Additional assessments may involve blood tests to check cholesterol levels and kidney function, as well as dietary recommendations from specialists like registered dietitians. The ultimate goal is to control hypertension effectively and minimize complications like cardiovascular diseases or stroke.
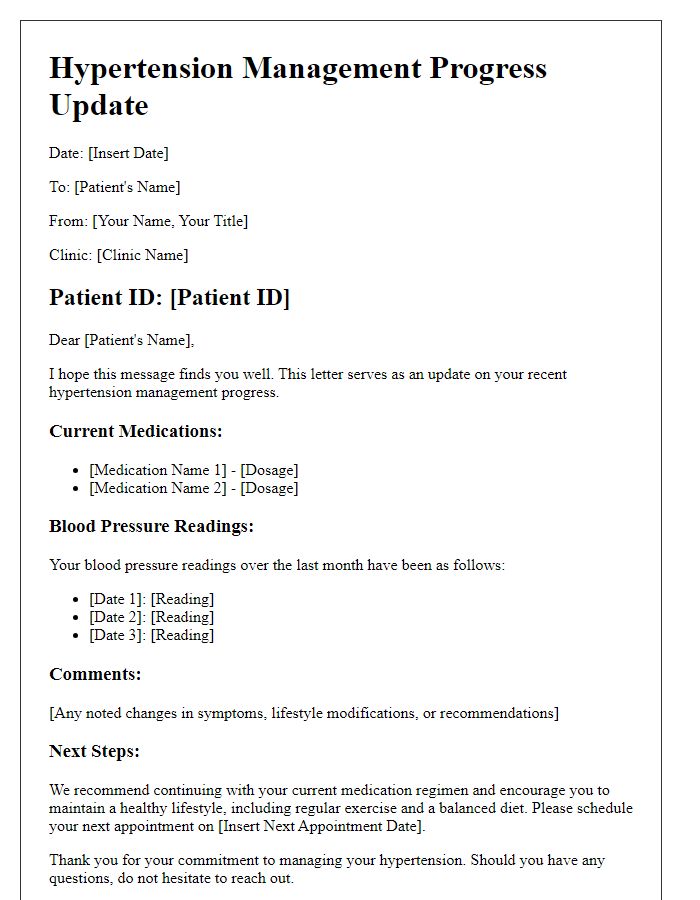
Summary of patient medical history and current condition
Hypertension management involves monitoring blood pressure levels to reduce the risk of cardiovascular diseases such as stroke and heart attack. A patient with a history of hypertension may have recorded systolic values (top number) over 130 mmHg and diastolic values (bottom number) above 80 mmHg on average during monitoring sessions. Previous medical events, including hospitalizations for hypertensive crisis, medications such as ACE inhibitors or calcium channel blockers, and lifestyle factors like a high-sodium diet or sedentary behavior, contribute to the patient's current condition. Regular follow-ups with healthcare providers and lifestyle modifications--such as implementing a low-sodium diet, increasing physical activity, and managing stress--are critical in creating a comprehensive hypertension management plan. Additionally, essential lab tests may include kidney function tests and lipid profiles to assess overall health and potential complications.
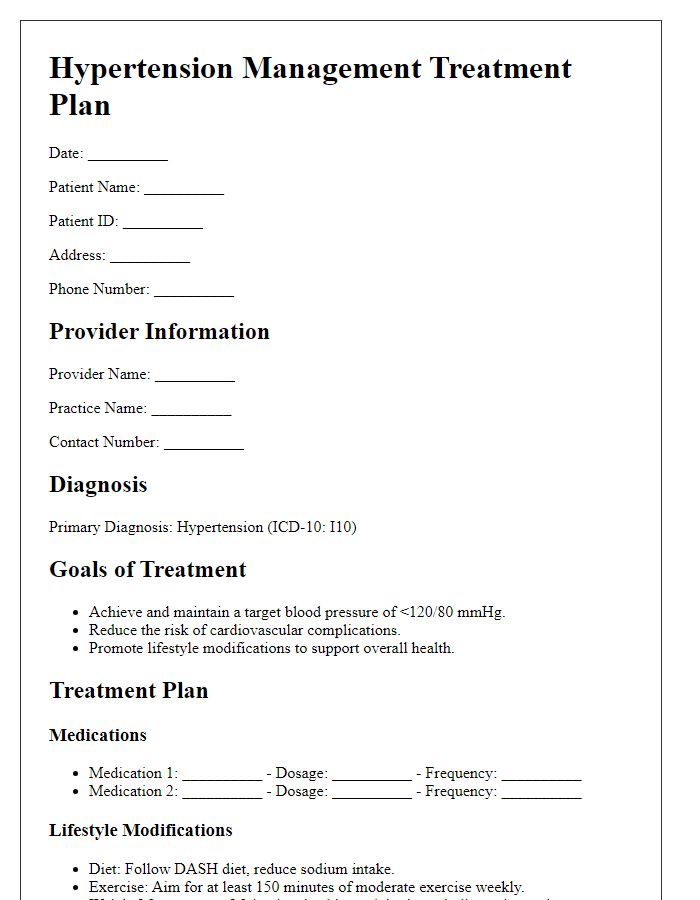
Recommended treatment plan and lifestyle changes
Hypertension (high blood pressure) management requires a comprehensive treatment plan that includes medication and lifestyle changes. Common medications prescribed include ACE inhibitors, diuretics, and beta-blockers, which target blood pressure regulation. Lifestyle modifications are essential; adopting a heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, emphasizes fruits, vegetables, whole grains, and low-fat dairy while reducing sodium intake to less than 2,300 mg daily. Regular physical activity, aiming for at least 150 minutes of moderate exercise weekly, can significantly lower blood pressure. Weight management is also critical; maintaining a healthy body mass index (BMI) under 25 can further enhance blood pressure control. Stress-reducing techniques, such as meditation or yoga, contribute positively to overall cardiovascular health. Regular monitoring of blood pressure at home is advisable, ideally to keep readings around 120/80 mmHg, while consistent follow-ups with healthcare professionals ensures the optimization of the treatment plan.
Contact information and next steps for follow-up
Hypertension management consultations involve detailed monitoring and personalized strategies to maintain optimal blood pressure levels. Effective communication channels, such as phone numbers and email addresses, are essential for establishing a reliable connection between healthcare providers and patients. Follow-up appointments typically occur every one to three months, depending on individual progress, treatment adherence, and lifestyle changes, ensuring that patients receive appropriate adjustments to their management plans. Educational materials about the DASH diet, exercise routines, and medication adherence play a critical role in empowering patients to effectively manage their hypertension. Collecting patient data during consultations, including blood pressure readings, weight, and lifestyle factors, allows healthcare professionals to tailor interventions and track overall health improvements.
Letter Template For Hypertension Management Consultation Samples
Letter template of hypertension management referral for patient evaluation
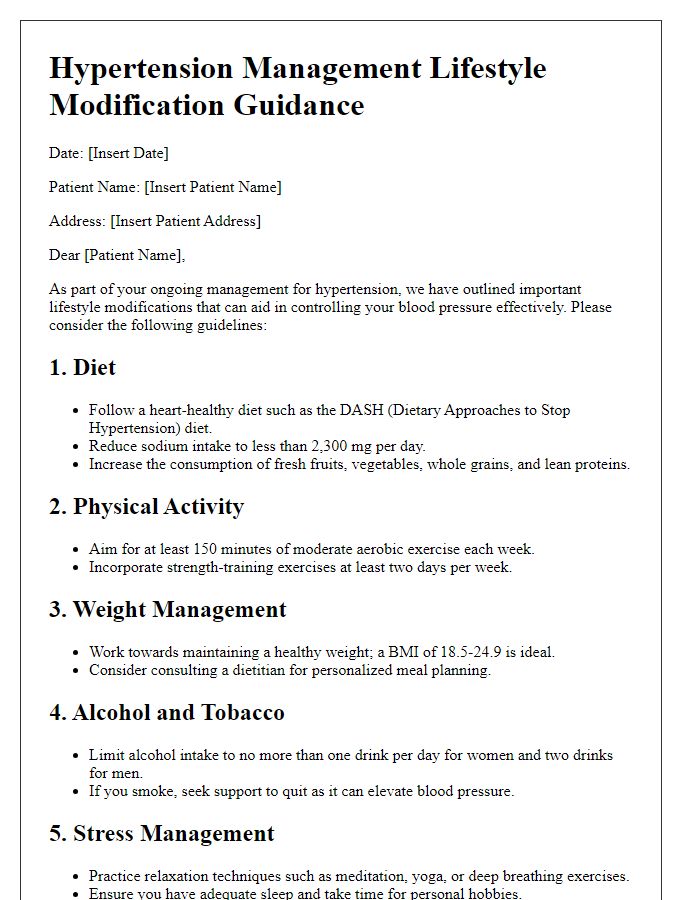
Letter template of hypertension management lifestyle modification guidance



Comments