Navigating the conversation around end-of-life care preferences can often feel overwhelming, but it doesn't have to be. It's important to approach this sensitive topic with compassion and clarity, allowing everyone involved to express their thoughts and wishes openly. By initiating this dialogue, you can ensure that your loved one's desires are understood and respected, ultimately guiding their care in a way that aligns with their values. So, let's explore how to facilitate this essential conversation in a gentle and constructive mannerâkeep reading to discover valuable tips and insights!
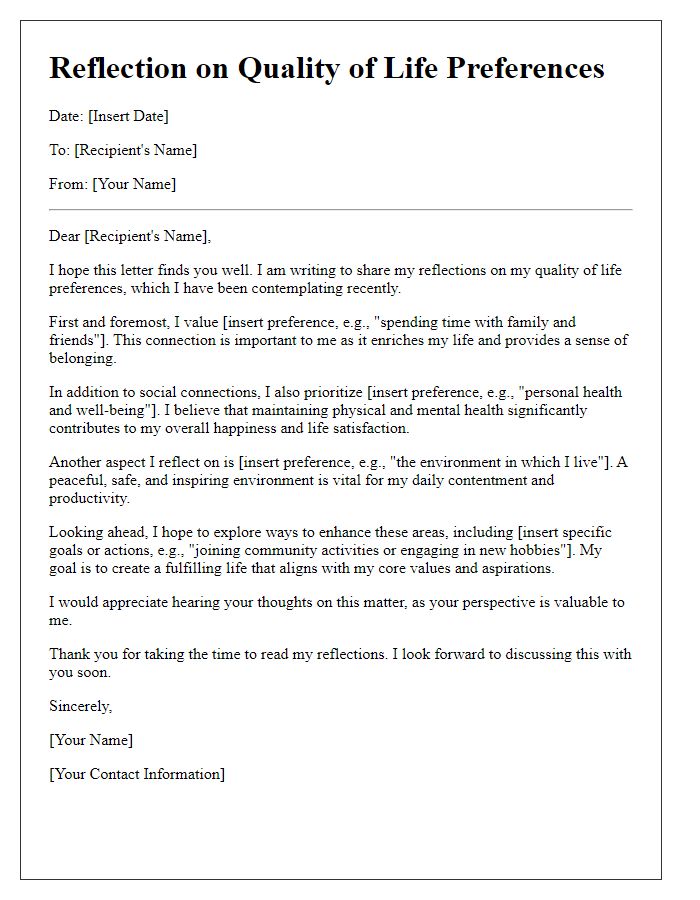
Personal Values and Beliefs
In discussions about end-of-life care preferences, personal values and beliefs hold significant importance in shaping decisions regarding treatment options, quality of life, and pain management. Many individuals may prioritize comfort over aggressive interventions when facing terminal illnesses such as cancer (with a projected 1.9 million new cases in the U.S. in 2022). Cultural beliefs can influence choices about medical procedures, with some valuing family involvement versus personal autonomy. Religious perspectives (ranging from Christianity to Buddhism) often provide guidelines on how to approach suffering and death, leading to differing views on euthanasia and palliative care. Additionally, the impact of individual experiences and relationships shapes these preferences, emphasizing the need for conversations that explore not only medical desires but also emotional and spiritual needs during the final stages of life. Such thoughtful discussions lead to a deeper understanding of a person's unique wishes, ensuring that care aligns with their core values.
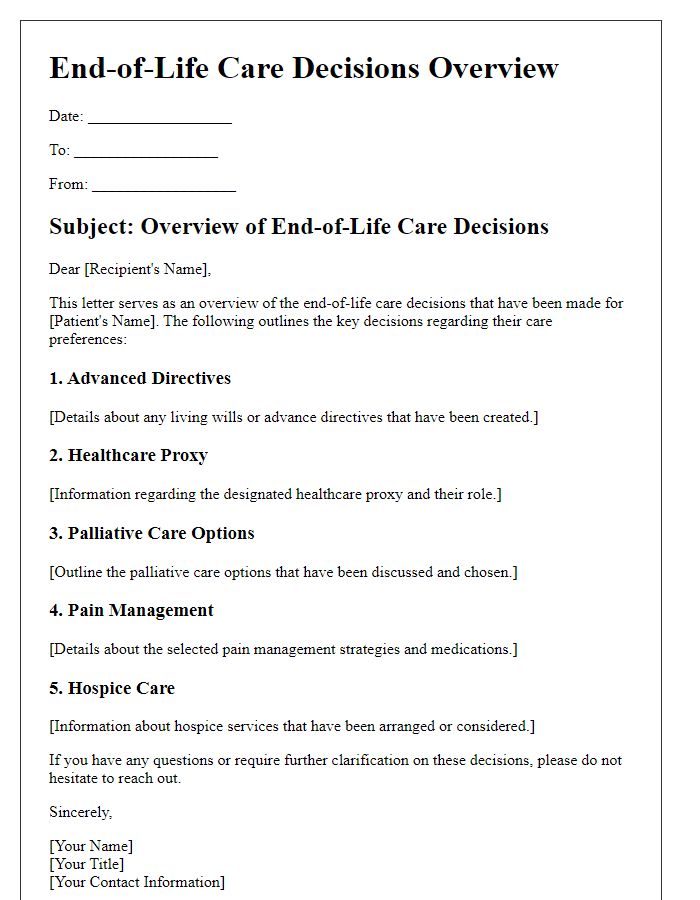
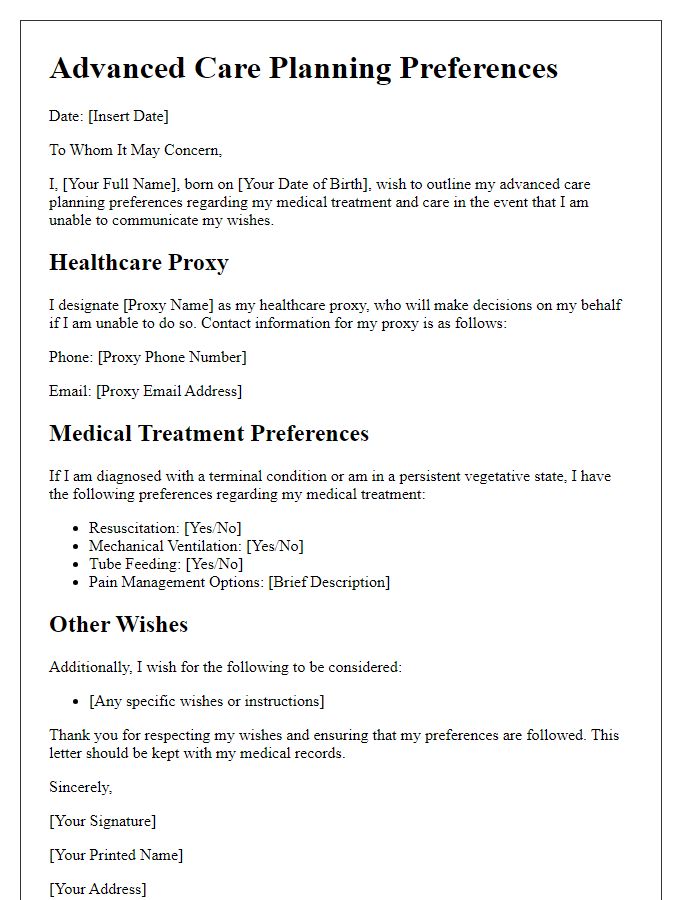
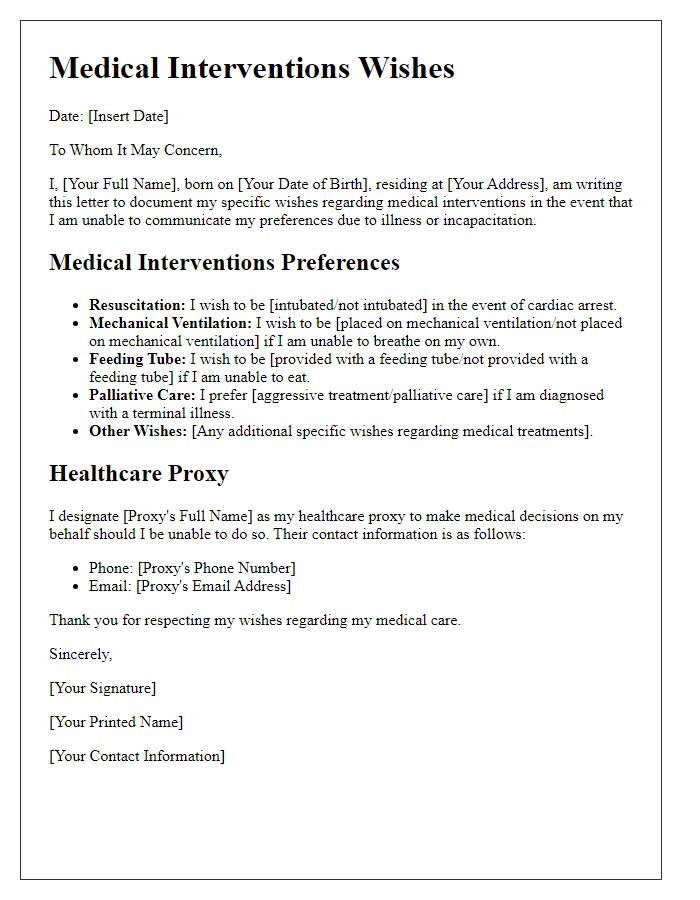
Medical Treatment Preferences
End-of-life care preferences encompass a critical aspect of individual healthcare decisions, focusing on the values and wishes regarding medical interventions during the final stages of life. Individuals, along with their families and healthcare providers, should discuss specific medical treatment preferences, which may include resuscitation efforts (such as CPR), ventilation support, and palliative care measures aimed at enhancing comfort. Important settings for these discussions can be hospice facilities, hospitals like Cleveland Clinic or Johns Hopkins, or even home environments. Each person's preferences can reflect unique beliefs, cultural backgrounds, and prior experiences with healthcare, guiding decisions that prioritize dignity and quality of life. Documentation of these preferences through tools like advance directives or living wills ensures that wishes are respected and communicated effectively to all members of the healthcare team.
Designated Healthcare Proxy
During the end-of-life care preferences discussion, identifying a designated healthcare proxy is essential for ensuring that personal medical decisions align with the patient's wishes. A healthcare proxy is an individual, often a family member or trusted friend, who is authorized to make medical decisions on behalf of the patient in instances where they cannot communicate their desires. Key considerations include discussing preferred medical interventions, pain management options, and the extent of life-sustaining treatments such as resuscitation or mechanical ventilation, which can guide the proxy's actions. Proper documentation through advance directives or living wills is crucial, providing legal weight to the healthcare proxy's decisions. Furthermore, choosing a proxy who understands the patient's values, beliefs, and healthcare priorities is invaluable, as it fosters open communication regarding preferences while ensuring that emotional support is available during challenging times.
Comfort and Support Measures
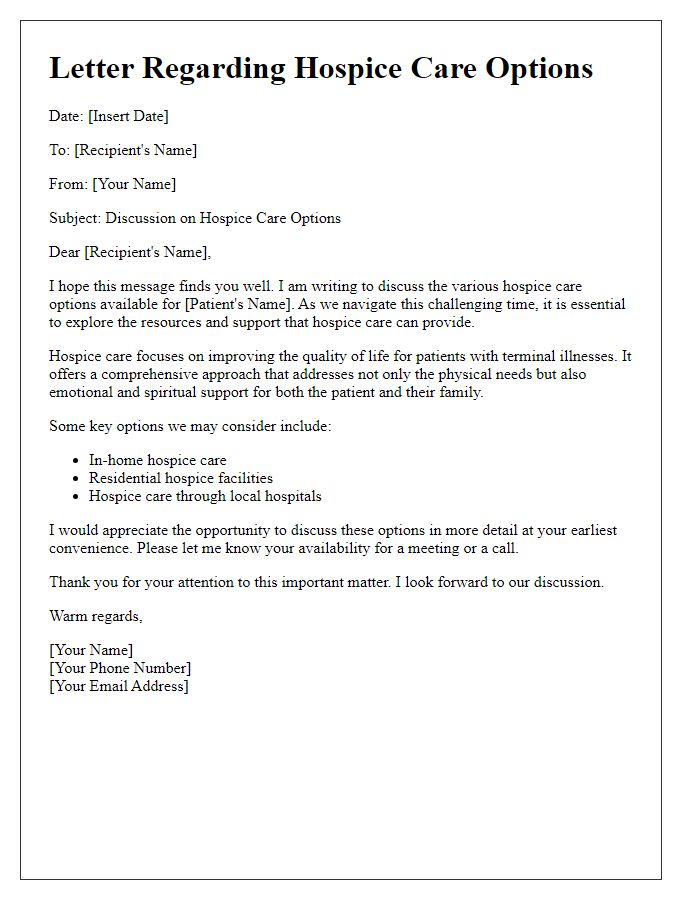
End-of-life care preferences encompass crucial decisions surrounding comfort and support measures for individuals facing terminal illnesses. Palliative care focuses on alleviating distress symptoms, ensuring the physical well-being of patients such as pain relief through medications like opioids or nonsteroidal anti-inflammatory drugs (NSAIDs). Psychological support is equally important, facilitated by mental health professionals, offering counseling to cope with emotional and existential challenges. Advanced care planning includes discussions of Do Not Resuscitate (DNR) orders, ensuring patients' wishes are respected, particularly regarding life-sustaining treatments. Environmental considerations, such as the option for home hospice care, create a familiar and comforting setting, maximizing emotional support from family and friends, enhancing the quality of life in one's final days. Communication with healthcare providers ensures alignment with patients' values and desires in these critical moments.
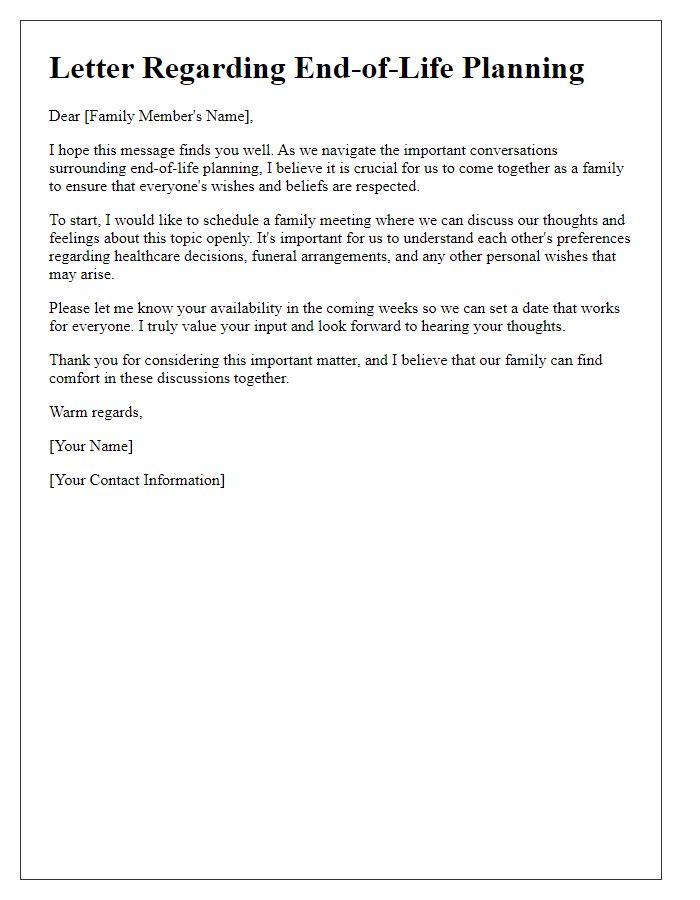
Communication with Family and Caregivers
End-of-life care preferences discussion plays a crucial role in ensuring that individuals receive the care they desire as they approach life's final stages. Advanced Care Planning (ACP) encourages open dialogues between patients, family members, and caregivers regarding medical decisions and emotional needs. This communication should ideally take place in a calm and supportive environment, allowing family members to share their thoughts and concerns. Key aspects to consider in this conversation include the patient's wishes for hospice care, preferences for pain management, and decisions regarding life-sustaining treatments. Locations such as hospitals, home settings, or assisted living facilities often influence these discussions, as they may impact care options available. Moreover, understanding the legal elements, such as living wills and healthcare proxies, can provide clarity and support for loved ones during difficult times.


Comments