Are you struggling to understand the prognosis of a dermatological condition? Many individuals feel uncertain when navigating the complexities of skin health and treatment options. This article aims to shed light on what you can expect from various skin conditions and how they may develop over time. Join us as we explore insights and tips that can help you manage your dermatological experience more effectively.
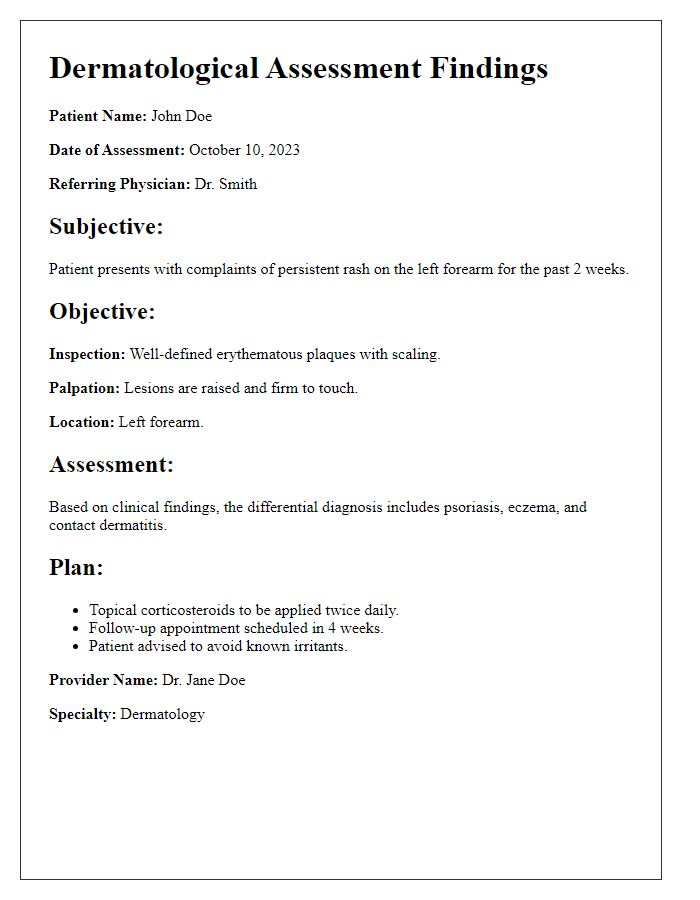
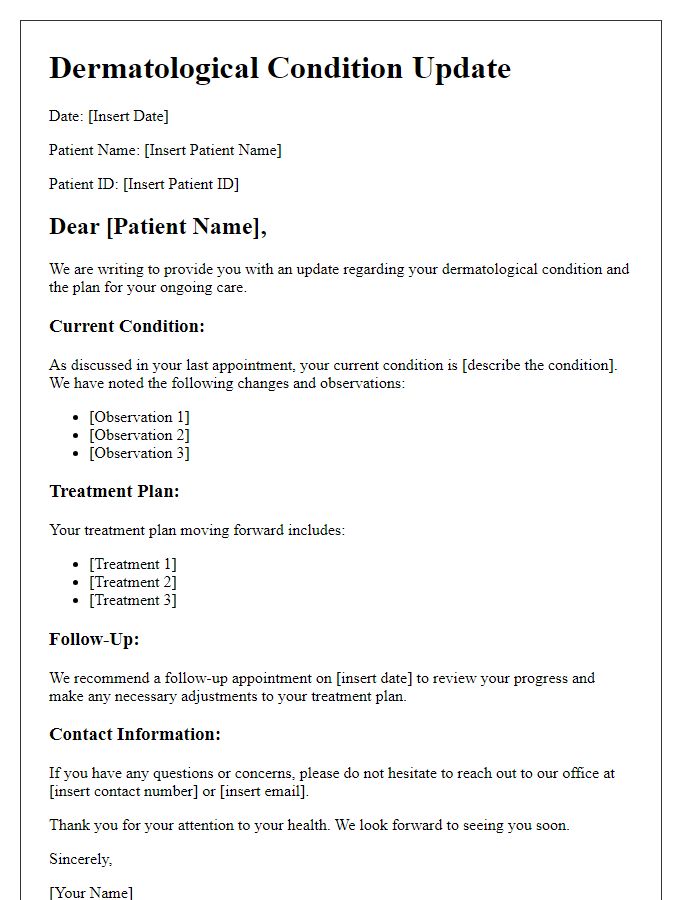
Patient Details
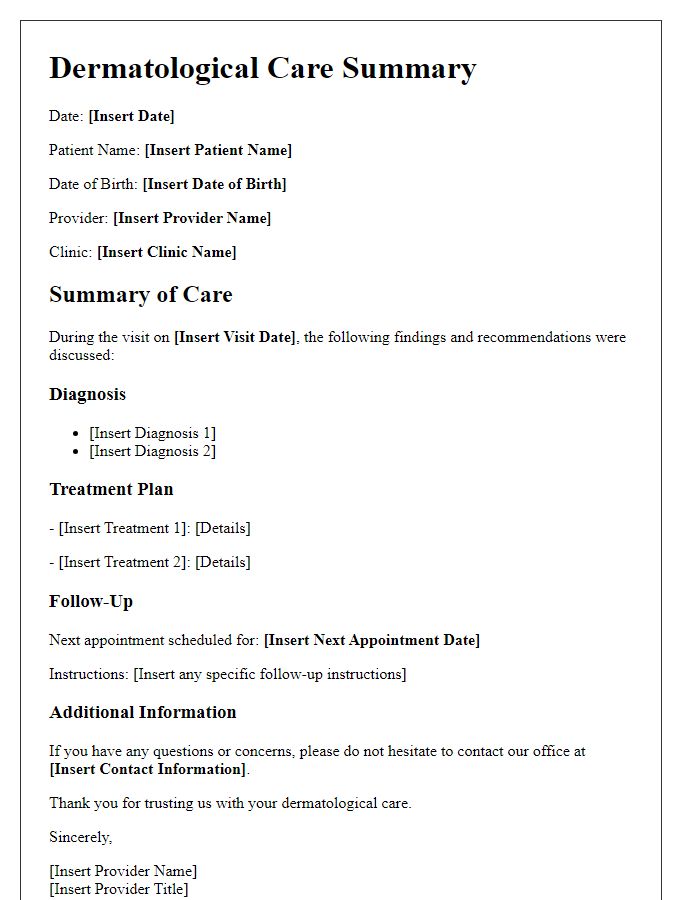
The dermatological condition prognosis for patients involves an evaluation of their skin health, focusing on various factors such as age, genetics, and UV exposure. For instance, patients diagnosed with acne vulgaris, commonly affecting adolescents between ages 12 and 24, often observe fluctuations in severity based on hormonal changes. Patients with chronic conditions like psoriasis, affecting approximately 2% of the global population, may experience episodic flare-ups triggered by stress or environmental factors. Key prognostic indicators include treatment history, family history of skin disorders, and adherence to prescribed therapies. A comprehensive assessment is essential for tailored management plans, aiming to improve the patient's quality of life and skin appearance.
Diagnosis Summary
Seborrheic dermatitis is a chronic inflammatory skin condition often affecting areas with high sebaceous (oil-producing) glands, such as the scalp, face, and upper back. This condition can manifest as red, flaky patches and greasy, yellowish scales, measuring approximately 0.5 to 2 centimeters in diameter. Commonly influenced by factors such as stress and hormonal changes, seborrheic dermatitis can lead to significant discomfort and self-esteem issues. Treatment typically involves antifungal agents like ketoconazole and topical corticosteroids to alleviate symptoms and control inflammation. Regular follow-up appointments are essential for monitoring the condition and adjusting treatment plans, particularly as individual responses may vary. It's important to maintain good skin hygiene and avoid triggers for effective management of this dermatological condition.
Prognosis Explanation
Dermatological conditions can significantly impact quality of life, with varied prognoses depending on the specific condition and individual factors. For instance, psoriasis, a chronic autoimmune disorder affecting approximately 7.5 million people in the United States, often results in red, scaly patches on the skin. With appropriate treatment, including biologics or topical therapies, many patients experience significant symptom relief and improved skin clearance. In contrast, dermatitis, such as atopic dermatitis, may present with recurrent flare-ups influenced by environmental allergens, necessitating a long-term management plan. Factors such as genetics, age, and comorbid conditions, like obesity or diabetes, also play crucial roles in determining overall prognosis. Recognizing the importance of early diagnosis and tailored treatment plans can substantially enhance patient outcomes, promoting healthier skin and improved mental well-being. Education on lifestyle modifications, including moisturizing routines and potential triggers, further supports managing these conditions effectively.
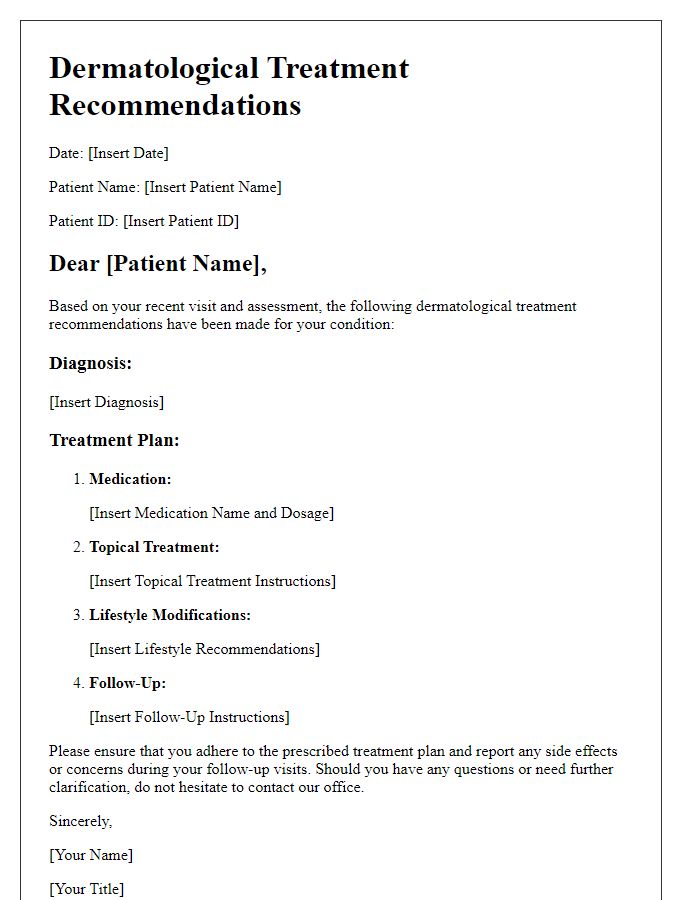
Treatment Plan
A comprehensive treatment plan for individuals experiencing dermatological conditions, such as psoriasis (chronic autoimmune disorder affecting skin), includes several key components. Topical therapies containing corticosteroids (anti-inflammatory agents) are commonly prescribed to reduce inflammation and alleviate itching. Systemic medications, like methotrexate (immunosuppressant), may be considered for moderate to severe cases. Phototherapy, utilizing ultraviolet light (such as UVB or PUVA treatments), is effective in managing symptoms by targeting affected skin areas. Regular follow-ups at dermatology clinics (specialized medical facilities) ensure treatment efficacy and adjustment based on patient response. Maintaining a skincare routine with hydrating moisturizers can further support recovery and enhance skin barrier function.
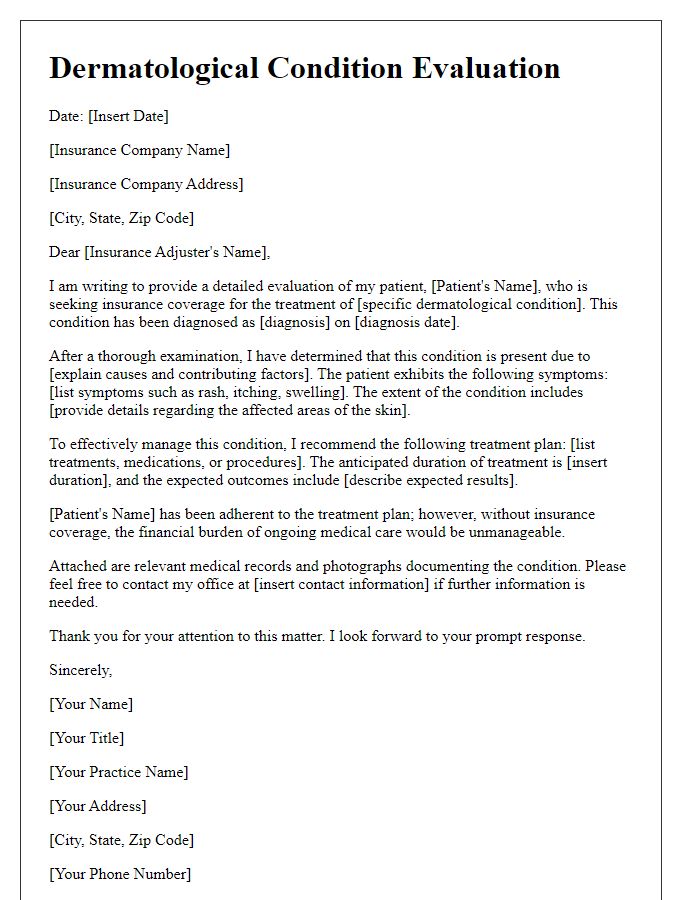
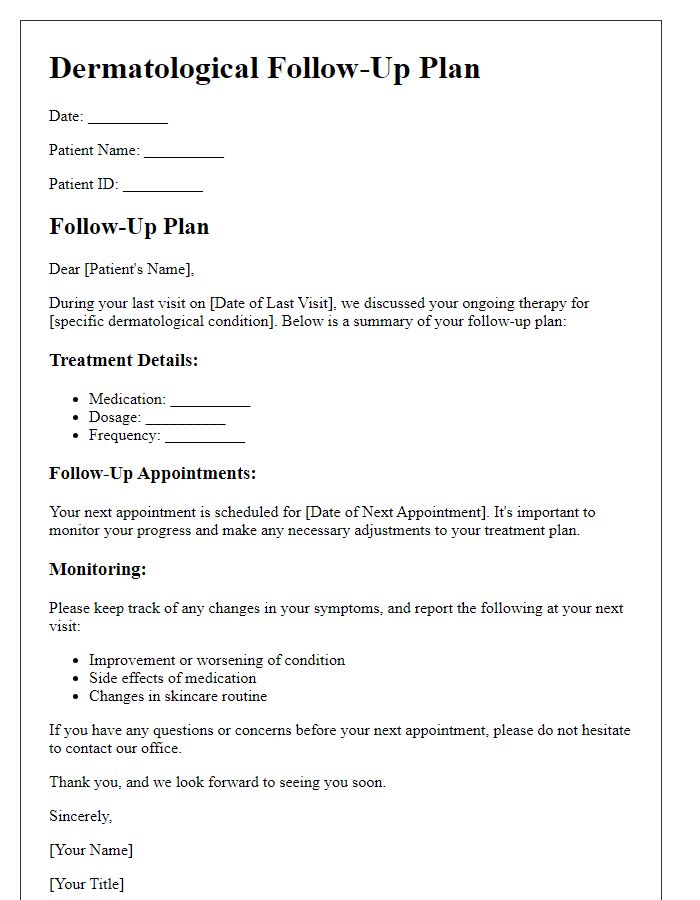
Follow-up Recommendations
Follow-up recommendations for managing a dermatological condition, such as psoriasis, typically involve regular assessments by a dermatologist. Treatment frequency may vary, depending on severity; for moderate cases, bi-monthly visits are suggested. Skin examination focuses on affected areas, including elbows and knees, where symptoms like redness, scaling, and discomfort are common. Topical therapies, such as corticosteroids or Vitamin D analogs, may be adjusted based on observed effectiveness. Phototherapy sessions, conducted in specialized clinics, typically occur two to three times weekly. Patients should maintain a symptom diary detailing flare-ups and triggers, like stress or environmental factors. Moisturization practices are crucial; patients should apply emollients frequently to manage dryness and prevent exacerbations. Discussion on lifestyle modifications, such as dietary changes and sun exposure, can further enhance skin health. Regular follow-ups aim to optimize treatment plans tailored to individual responses and improve overall quality of life.
Letter Template For Dermatological Condition Prognosis Samples
Letter template of dermatological assessment findings for medical records.
Letter template of dermatological treatment recommendations for patient management.
Letter template of dermatological condition evaluation for insurance purposes.
Letter template of dermatological referral information for specialist consultation.
Letter template of dermatological condition progress report for healthcare team.
Letter template of dermatological diagnosis confirmation for patient education.
Letter template of dermatological symptom description for clinical documentation.


Comments