When it comes to caring for our tiniest patients, having a solid neonatal care plan is essential for their well-being and development. This summary not only highlights the critical aspects of our approach but also emphasizes the importance of personalized care tailored to each newborn's unique needs. By detailing interventions, outcomes, and goals, we ensure that our medical team remains aligned and efficiently coordinates the best practices. So, if you're interested in learning more about how we create and implement these vital care plans, keep reading!
Patient Information
Neonatal care plans are essential for the healthy management of newborns, especially those in specialized units like NICU (Neonatal Intensive Care Unit). The patient information section includes details such as birth date (e.g., January 1, 2023), gestational age (e.g., 32 weeks), weight at birth (e.g., 1,500 grams), and any immediate medical conditions (e.g., respiratory distress syndrome). Additionally, details concerning parental information, such as caregiver names and contact numbers, play a crucial role in establishing a holistic support network. The care plan should also document specific interventions, such as feeding routines or medication schedules, alongside observation notes detailing vital signs, such as heart rate (typically 120-160 beats per minute for newborns) and temperature (normal range between 36.5 to 37.5 degrees Celsius). This comprehensive approach ensures appropriate monitoring and proactive support for the neonate's health and development.
Medical History
The medical history for a neonatal care plan includes critical information about the infant's birth, such as the gestational age (measured in weeks) at delivery, which provides insights into the infant's developmental stage, and any complications that occurred during labor and delivery, such as meconium aspiration or birth asphyxia. Information is also gathered on the mother's health during pregnancy, including any maternal infections like Group B Streptococcus or conditions such as gestational diabetes. Additional data on the infant's Apgar scores at one and five minutes post-delivery assesses immediate health status, while any congenital anomalies or genetic disorders identified through screening can inform the ongoing care approach, ensuring all medical needs are addressed systematically in the care plan.
Current Treatment Plan
A comprehensive neonatal care plan encompasses vital assessments and interventions in the unit, specifically designed for premature infants such as those born under 32 weeks of gestation. Routine monitoring priorities include oxygen saturation levels and heart rate, with specific parameters set to maintain stable vital signs, typically above 90% for oxygen saturation. Nutritional support involves providing fortified breast milk or formula to meet calorie intake goals, often targeting a range of 100-120 kcal/kg/day for optimal growth. Regular assessments for jaundice, especially bilirubin levels exceeding 12 mg/dL, necessitate phototherapy sessions to prevent complications. Care team collaboration, including neonatologists and pediatric nurses, ensures tailored interventions, frequently adjusting ventilator settings for infants requiring respiratory support to maintain appropriate peak inspiratory pressures. Additionally, skin-to-skin contact, or kangaroo care, is encouraged to promote bonding and thermoregulation, enhancing overall developmental outcomes for these vulnerable infants.
Clinical Progress and Observations
Neonatal care plans are crucial in monitoring the clinical progress and observations of premature infants. For instance, a baby born at 28 weeks (gestational age) may require specialized interventions, including respiratory support (such as CPAP machines) and temperature regulation through incubators. Daily assessments include monitoring vital signs (heart rate, respiratory rate, and temperature) to ensure stability, aiming for normal ranges (heart rate: 120-160 beats per minute). Nutritional support, often initiated with parenteral nutrition (IV feeding) before transitioning to enteral feeds, plays a key role in growth and development. Observations regarding skin integrity and potential infections are critical, particularly for infants with low birth weight or those in phototherapy for jaundice management. Regular multidisciplinary team meetings (including neonatologists and NICU nurses) facilitate ongoing evaluation and adjustment of the care plan, ensuring optimal outcomes for vulnerable patients.
Recommendations and Follow-up Care
Neonatal care plans are essential for the health and wellbeing of premature infants or those with health complications at birth. Recommendations for follow-up care should include regular pediatric evaluations (at least every 2-3 weeks for the first six months) to monitor growth, development, and any potential health issues. Nutritional support is crucial, with guidelines suggesting breast milk as the primary source of nutrients, fortified for premature infants. Vaccination schedules must adhere to current CDC guidelines to prevent infectious diseases. Specialized therapies may be needed, such as physical therapy for developmental delays or services from early intervention programs to support cognitive and motor skills development. Additionally, frequent communication with healthcare providers ensures holistic care, addressing both medical needs and family support resources, essential for nurturing the infant's emotional and psychological health.
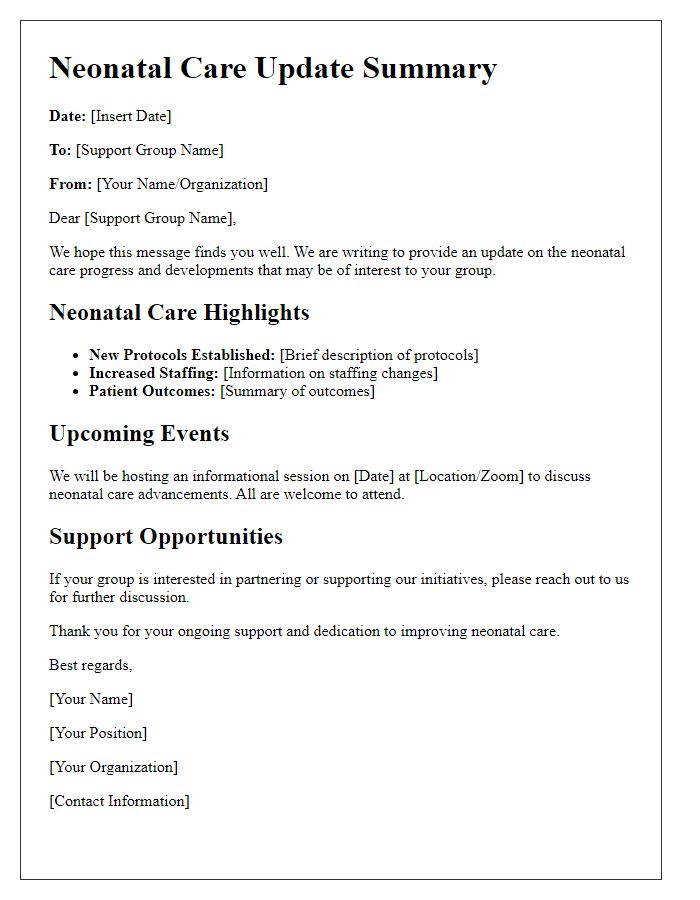
Letter Template For Neonatal Care Plan Summary Samples
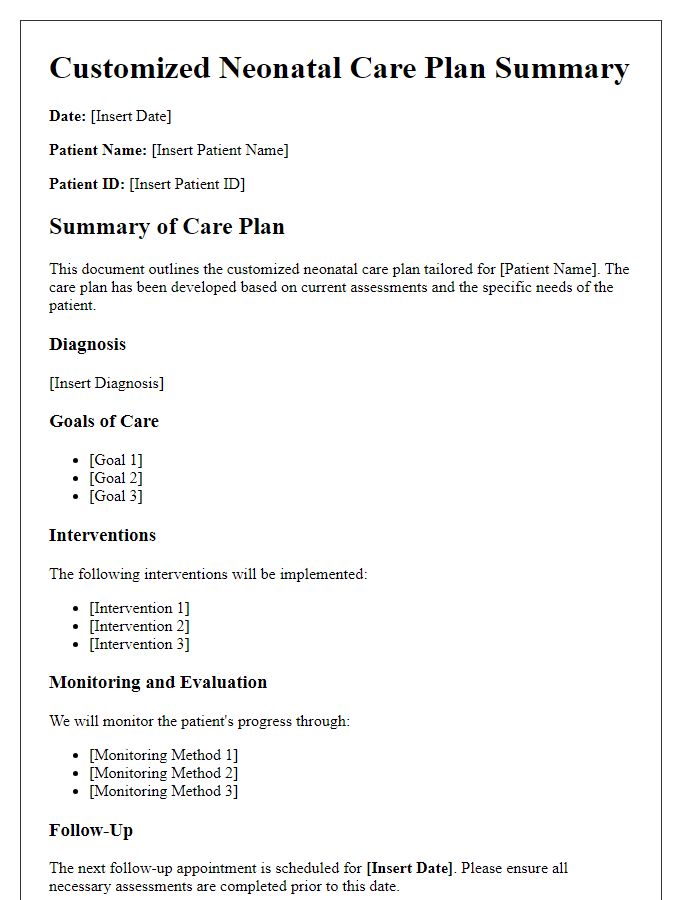
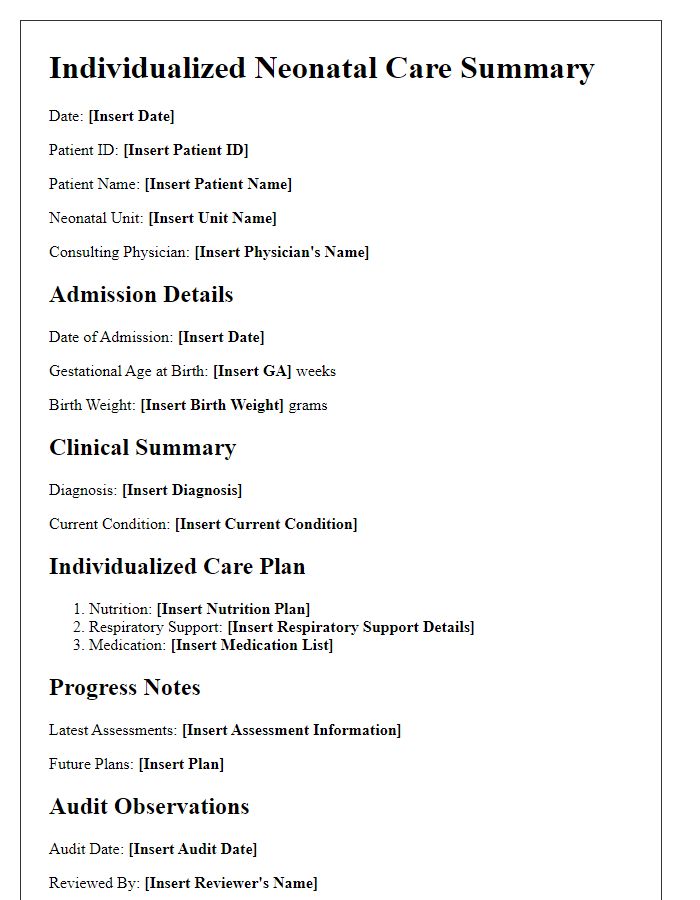
Letter template of customized neonatal care plan summary for specialists.
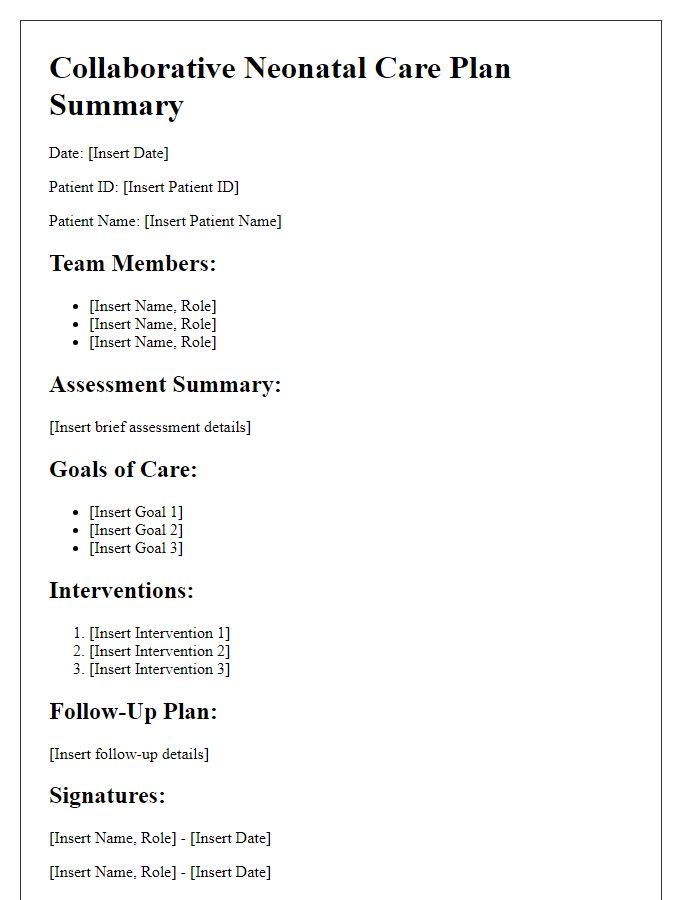
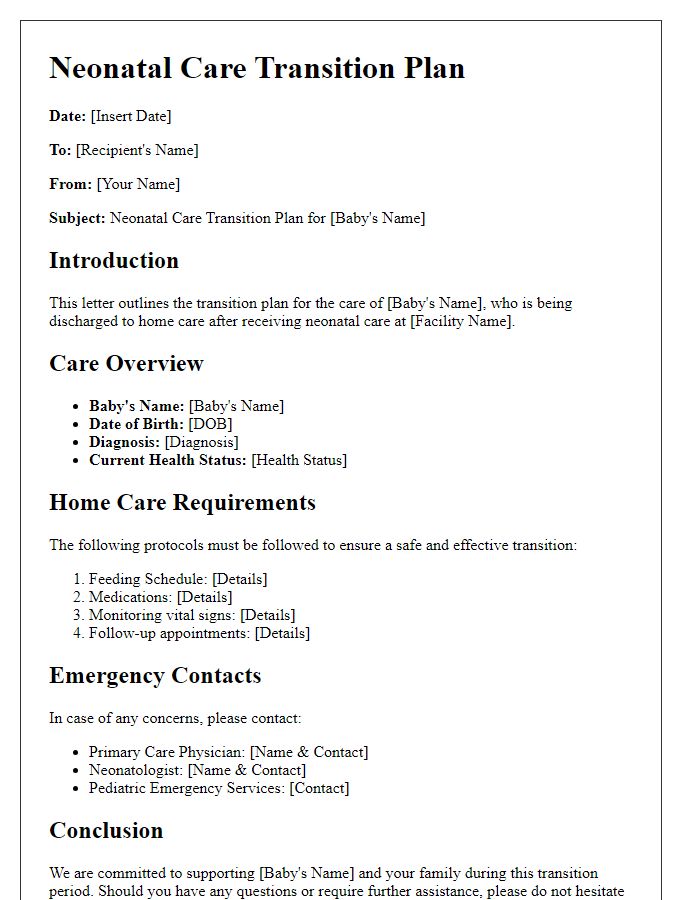
Letter template of collaborative neonatal care plan summary for multidisciplinary teams.


Comments