As we navigate the journey of caring for our beloved elderly patients, it's essential to keep them and their families informed about any updates to their care plans. Regular communication not only fosters trust but also ensures that everyone is on the same page regarding health goals and treatment strategies. In this article, we'll explore the key components of an effective letter template designed for keeping caregivers and family members updated on their loved ones' progress. So, stick around and discover the best practices for crafting these important messages!
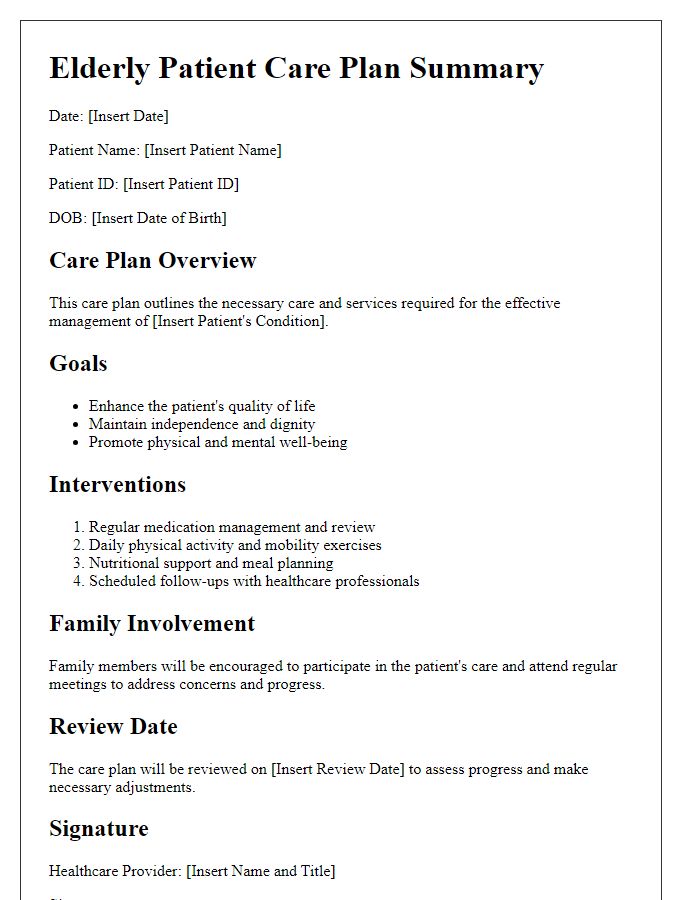
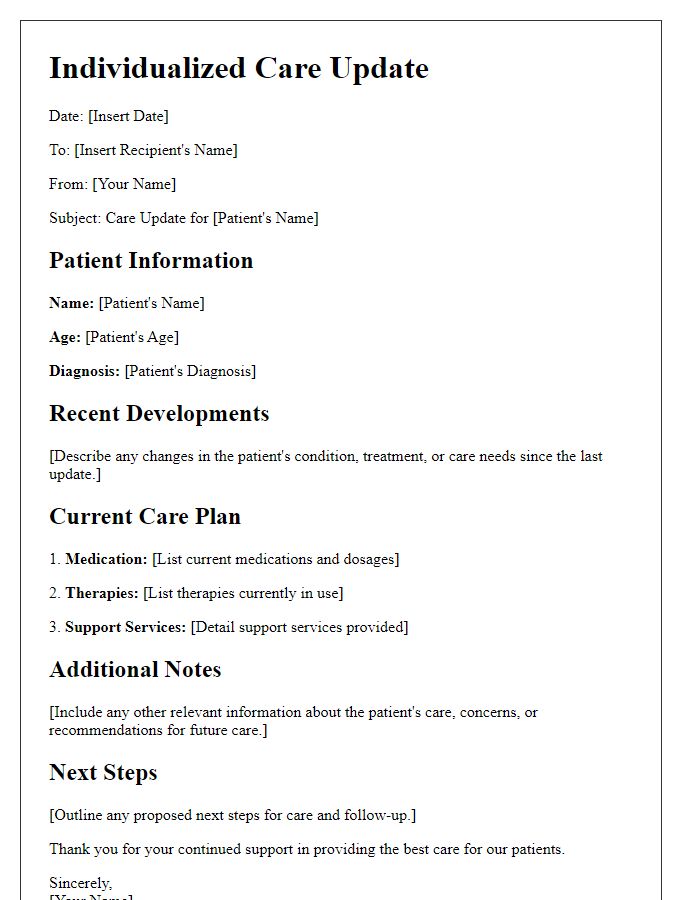
Patient Information: Name, age, medical history.
Update on elderly patient care plan reveals essential information for tailored support. Patient Name: John Smith, Age: 78 years, diagnosed with hypertension and type 2 diabetes mellitus, showcasing a medical history that includes a mild stroke in 2022 and moderate osteoarthritis. Regular check-ups at Sunshine Medical Center have indicated fluctuating blood sugar levels, necessitating adjustments in dietary plans and medication monitoring. A physical therapy program initiated to enhance mobility in his knee joints, scheduled twice a week at Enrichment Rehabilitation Center, is yielding positive results. Family involvement and caregiver support from Harmony Assisted Living remain critical in ensuring adherence to the care plan. Continued assessments will assist in addressing evolving healthcare needs promptly.
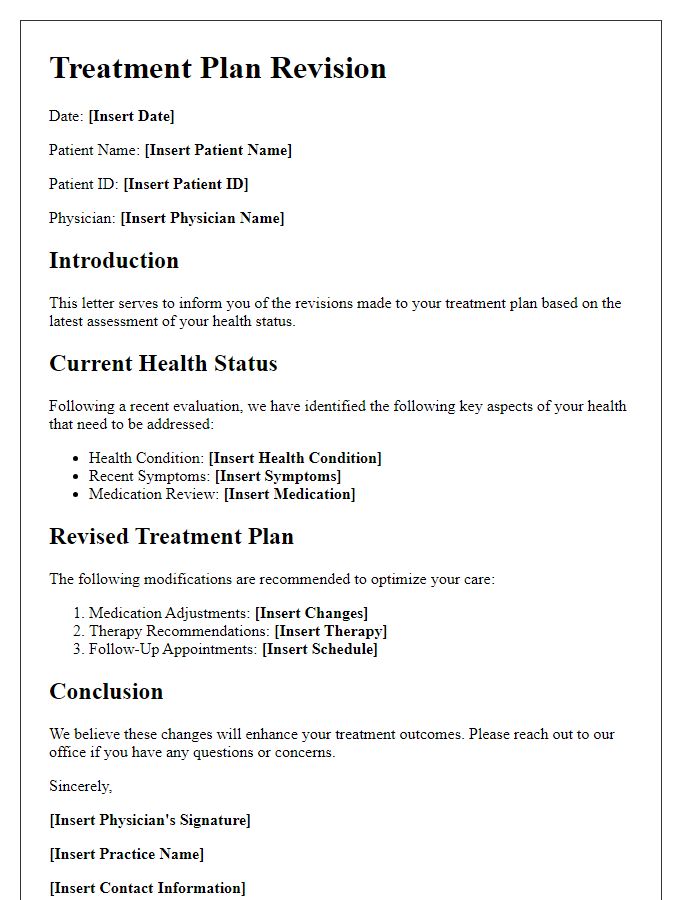
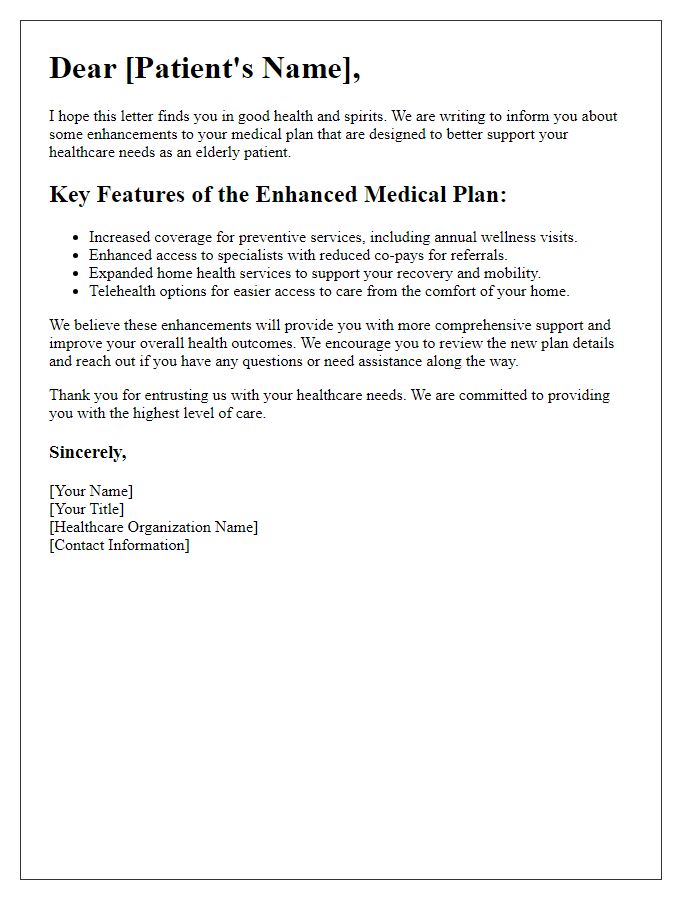
Current Health Status: Recent assessments, diagnostics.
Current health status of elderly patients often requires careful evaluation following recent assessments and diagnostics. Vital signs, such as blood pressure (normal range: 120/80 mmHg), heart rate (60-100 beats per minute), and glucose levels (70-130 mg/dL when fasting) provide critical information about overall health. Recent diagnostic tests, including blood panels and imaging studies, reveal essential markers for conditions like diabetes, hypertension, or potential heart disease. Mental health assessments, including the Geriatric Depression Scale, can indicate mood changes affecting daily living, while cognitive tests ensure memory functions are stable. Mobility evaluations, using tools like the Timed Up and Go test, help determine the risk of falls and the need for potential rehabilitation services. Overall, a comprehensive review of these factors ensures a tailored care plan that promotes optimal health and well-being for elderly patients.
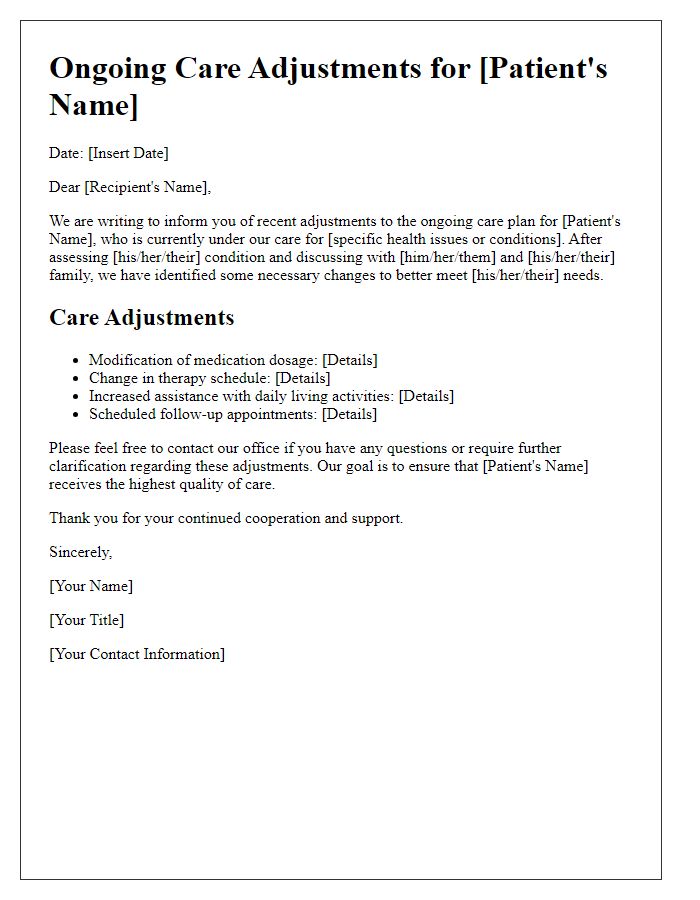
Care Plan Changes: Adjustments in medication, therapy, diet.
Medication adjustments for elderly patients often include a review of prescriptions, such as antihypertensives or anticoagulants, particularly to avoid polypharmacy issues (using multiple medications) that may lead to adverse reactions. Therapy changes may involve incorporating physical therapy sessions to enhance mobility and prevent falls, while occupational therapy can support daily living activities, ensuring safety and independence. Dietary modifications should focus on tailored nutrition plans, addressing specific health conditions like diabetes or heart disease, emphasizing heart-healthy foods and low-sugar options. Regular evaluations are essential for continuous improvement in this comprehensive care strategy to meet the evolving needs of elderly patients.
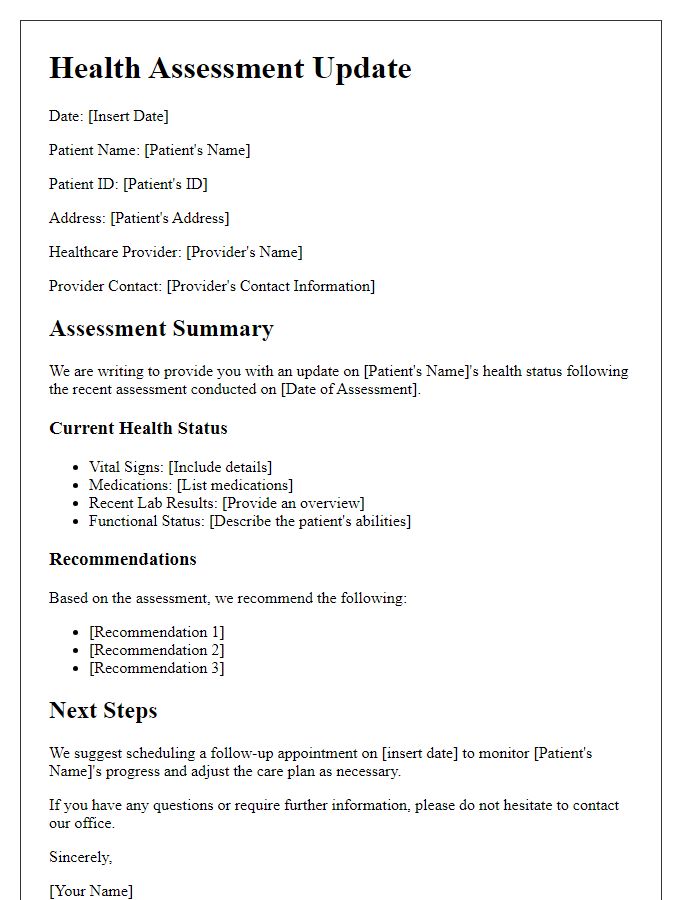
Caregiver Instructions: Responsibilities, contacts, emergency procedures.
Caregiver instructions for elderly patient care plans are critical in ensuring the health and safety of seniors. Responsibilities include daily medication management, which should adhere to prescribed schedules (specific times like 8 AM and 8 PM) to avoid dosage errors. Regular monitoring of vital signs, such as blood pressure (normal range 120/80 mmHg) and blood sugar levels (target reading around 70-130 mg/dL), must be recorded and reported to health care providers. Contacts should include primary care physician details, such as Dr. Jane Smith at City Hospital, along with emergency contacts--family members or friends who can be reached rapidly. Emergency procedures must outline steps to take in case of a fall, stroke symptoms (such as sudden confusion, speaking difficulty), or cardiac events (recognizable by chest pain). Additionally, familiarize with local emergency services, such as dialing 911 in the United States, to ensure prompt action in critical situations.
Follow-up Schedule: Appointments, future evaluations, communication plan.
The follow-up schedule for elderly patient care includes structured appointments aimed at monitoring health developments. Routine evaluations are designated every three months to assess chronic conditions, such as hypertension and diabetes, with a focus on specific parameters like blood pressure readings and glucose levels. Communication plans involve bi-weekly check-ins through telephone consultations or virtual visits to address ongoing health concerns and medication management. Additionally, referrals to specialists, including cardiologists and endocrinologists, may be arranged as necessary based on the patient's progress and health feedback received during evaluations. This comprehensive approach ensures continuity of care and timely interventions for optimal health outcomes.


Comments