Navigating the sensitive topic of end-of-life care can be challenging, but it's a conversation that can bring peace and clarity. By openly discussing wishes and preferences, we can ensure that our loved ones receive the care they truly desire. This dialogue not only eases future decision-making but also strengthens the bonds between family members. Curious to learn more about how to approach this important discussion?
Patient's Understanding and Preferences
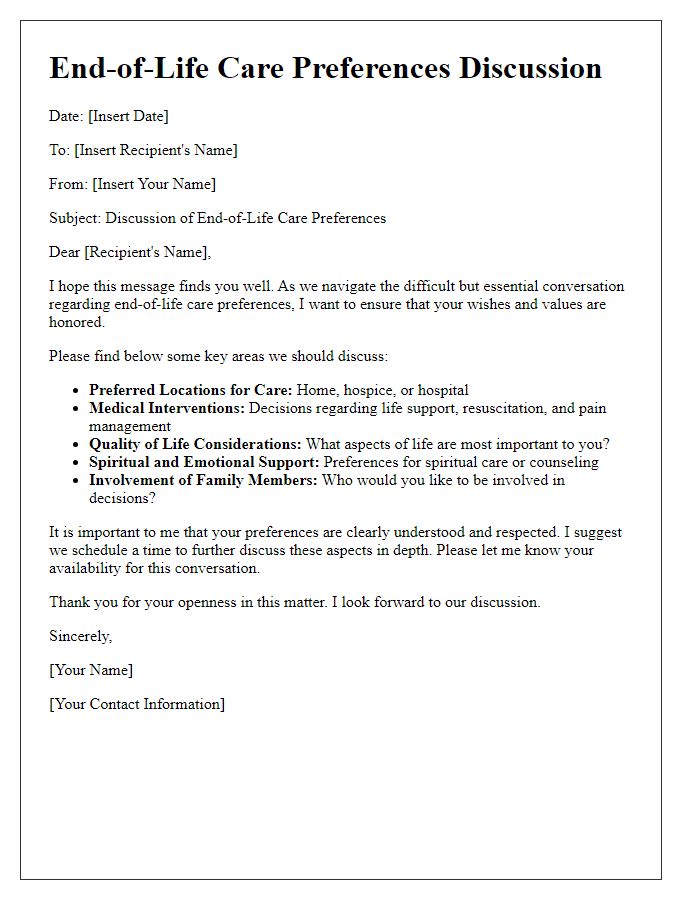
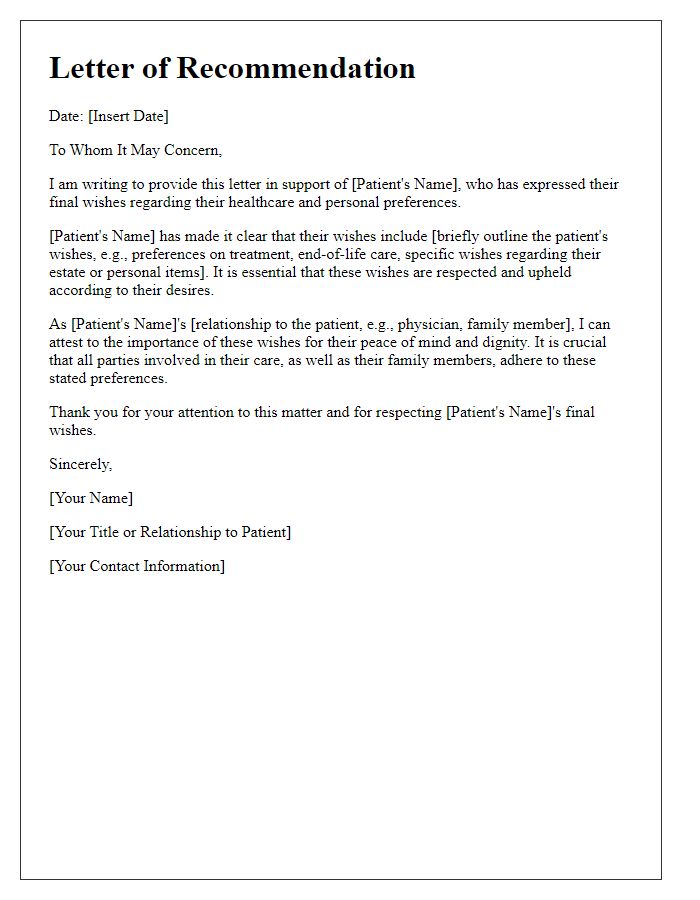
End-of-life care discussions are essential for ensuring that a patient's preferences and understanding of their condition are aligned with medical recommendations. This includes comprehensively evaluating the patient's diagnosis, which may involve terminal illnesses such as advanced cancer or end-stage renal failure, affecting care decisions. Healthcare providers must engage in empathetic communication, allowing the patient to express their desires regarding palliative options, life-sustaining treatments, and hospice care. Attention should be paid to the patient's emotional state, understanding of their prognosis, and cultural beliefs about death and dying, as these factors critically influence their choices. Additionally, it is crucial to document the patient's expressed wishes, ensuring that their preferences guide future medical interventions and uphold their dignity in care.
Communication of Prognosis and Options
End-of-life care discussions are crucial for ensuring that patients and families understand the prognosis and available options. These conversations typically take place in healthcare settings like hospitals or hospice care units. The healthcare team, including physicians, nurses, and social workers, plays a vital role in providing clear information about terminal illnesses, such as advanced cancer stages or end-organ failure. Prognosis may include the life expectancy estimates, which can range widely depending on individual health conditions, from a few weeks to several months. Options for care might encompass palliative care, which prioritizes comfort over curative measures, and advanced directives that outline a patient's preferences for treatment. Highlighting the importance of open dialogue, these discussions aim to empower families to make informed decisions aligned with the patient's values and wishes.
Emotional and Spiritual Support
End-of-life care is crucial for providing comfort and dignity to individuals facing terminal illnesses, with emotional and spiritual support playing key roles. Emotional support involves addressing feelings of fear, sadness, and anxiety often experienced by patients and their families during this challenging time. Techniques such as active listening and empathetic communication create a safe space for sharing feelings. Spiritual support, often facilitated by chaplains or spiritual counselors, involves addressing existential questions and offering comfort through faith or personal beliefs. Integration of holistic approaches, such as art therapy or mindfulness practices, can enhance the emotional well-being of patients. Engaging family members in conversations about values, legacy, and wishes fosters a deeper understanding and connection within the family unit. Resources such as support groups and grief counseling services provide additional layers of assistance, ensuring that both patients and families navigate the complexities of end-of-life care with compassion and respect.
Legal and Financial Considerations
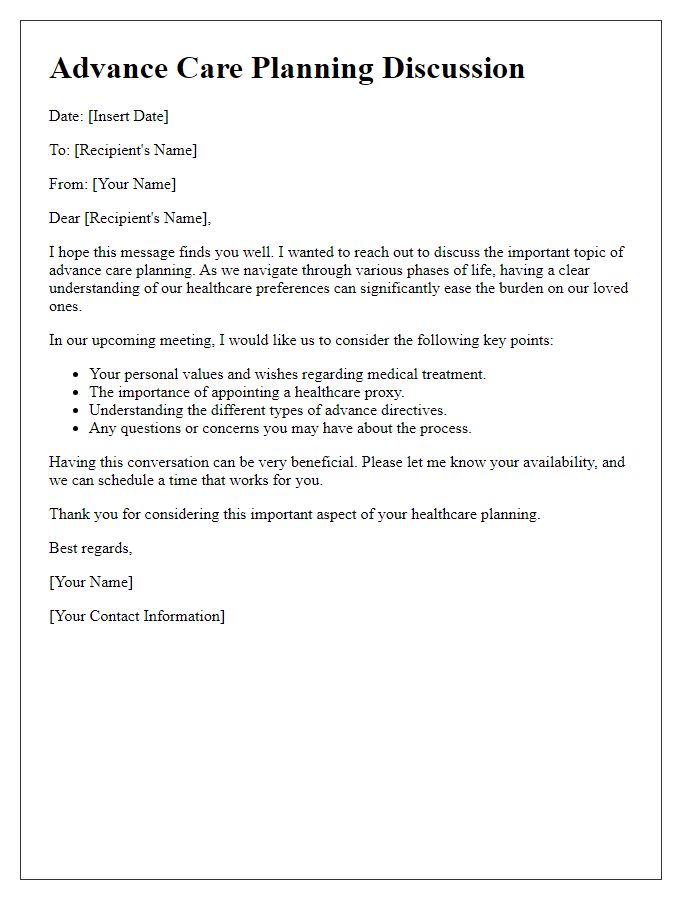
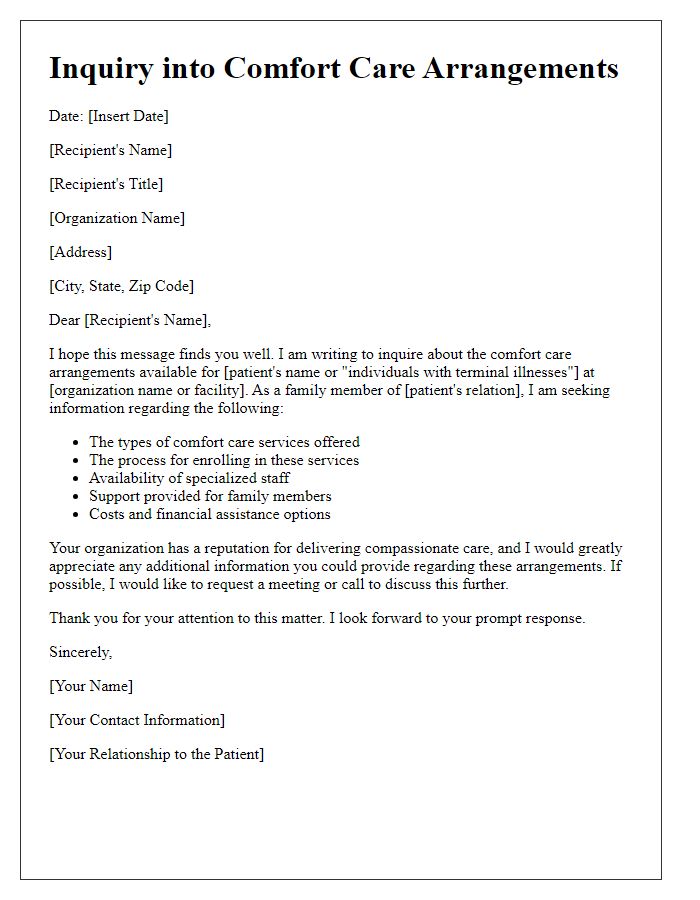
End-of-life care discussions hold significant importance for individuals and families facing critical health decisions. Legal documents, such as advance directives and living wills, outline patient preferences, ensuring autonomy in medical decisions when individuals are incapacitated. Financial considerations include potential costs associated with hospice services, palliative care, and health insurance coverage limitations. Understanding the implications of the Patient Protection and Affordable Care Act (PPACA) on end-of-life care can guide families in navigating healthcare options. Additionally, conversations about power of attorney and guardianship assist in delineating responsibilities for making financial and healthcare choices, offering clarity during emotionally challenging times. Lastly, ensuring that beneficiaries are clearly designated in estate planning documents can prevent disputes and provide peace of mind.
Coordination with Healthcare Team and Family
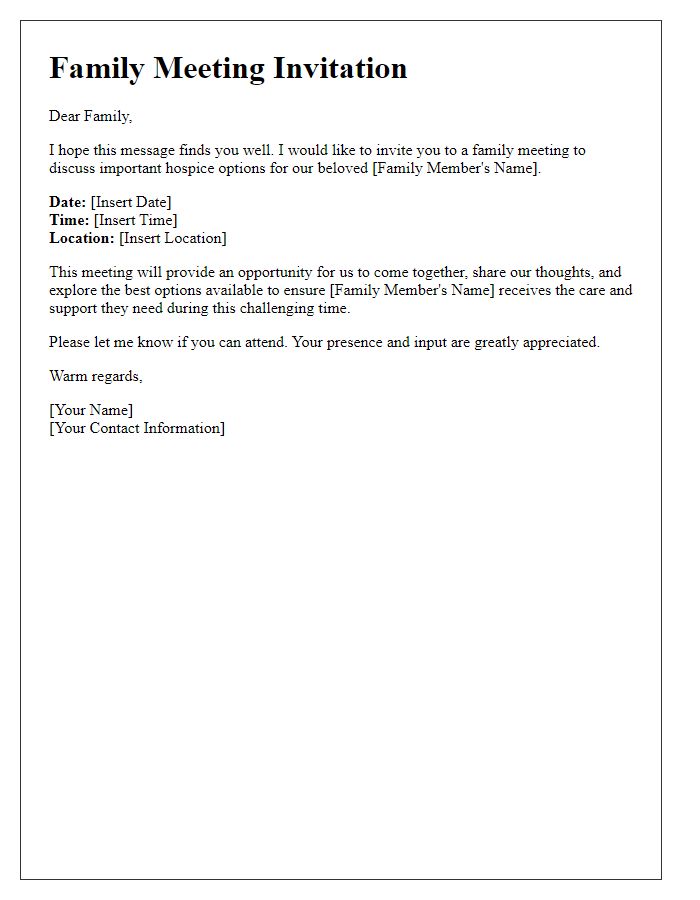
End-of-life care discussions require sensitive coordination between healthcare teams and family members. Clear communication is essential to align everyone's goals and preferences regarding patient comfort and quality of life. Healthcare team members, including physicians, nurses, and social workers, must ensure accurate information dissemination about the patient's condition, prognosis, and available palliative options. Family involvement is critical; emotional support and understanding can be enhanced through regular meetings in settings like hospitals or homes, particularly when caregivers are present. Documenting preferences in advance care planning documents, such as advance directives or POLST (Provider Orders for Life-Sustaining Treatment), helps honor the patient's wishes. This collaborative approach strengthens the bond between families and healthcare providers, fostering a compassionate and respectful environment during difficult times.


Comments