Navigating the tough decision to terminate a healthcare professional can be challenging, but it's essential for maintaining the quality of care in any medical facility. Clear communication and adherence to protocols are paramount in ensuring this process is handled with dignity and respect. By outlining the reasons for termination and providing the necessary support for transition, we can foster a more positive environment even in difficult times. If you're looking for a comprehensive letter template to guide you through this process, keep reading for expert insights and practical tips!
Professional Conduct Issues
Professional conduct issues can significantly impact the credibility and effectiveness of healthcare professionals. Such issues may involve breaches of ethical standards, inappropriate behavior towards colleagues or patients, and violations of established protocols. For example, continuous tardiness (arriving late more than five times within a month), failure to maintain patient confidentiality (disclosing sensitive patient information to unauthorized individuals), and inappropriate interactions (e.g., using disparaging language towards staff) often lead to serious consequences. Healthcare organizations, such as hospitals or clinics, typically address these matters promptly to uphold patient safety and maintain a professional working environment. Failure to adhere to the required standards can ultimately result in termination, which underscores the importance of professionalism and ethical conduct in the healthcare field.
Legal and Regulatory Compliance
Termination of a healthcare professional, particularly within institutions like hospitals or clinics, often involves complex legal and regulatory considerations. Documentation should reference compliance with the Health Insurance Portability and Accountability Act (HIPAA), which governs patient confidentiality and data protection standards in healthcare settings. Specific guidelines may come from state licensing boards, ensuring that termination follows established protocols set out by the National Practitioner Data Bank (NPDB). Additionally, incorporating local labor laws that mandate proper notice periods and severance guidelines contributes to ethical practices. The process typically culminates in a formal notification outlining reasons for termination, ensuring transparency while safeguarding the institution against potential legal repercussions.
Patient Safety Concerns
Patient safety concerns in healthcare settings can arise from numerous factors such as inadequate training, lack of adherence to protocols, or insufficient staffing. For instance, in hospitals like Massachusetts General Hospital in Boston, high patient volumes can strain resources, potentially leading to oversight in medication administration, increasing the risk of adverse events. Instances of negligence, such as incorrect dosages of critical medications (for instance, insulin or anticoagulants) have been documented, highlighting the importance of rigorous adherence to safety protocols. Additionally, communication failures among medical staff can exacerbate risks; a 2019 study found that miscommunication contributed to 30% of patient safety incidents. Proper evaluation and swift action on safety concerns are crucial, as they directly impact patient outcomes and trust in healthcare systems.
Documentation Standards
Termination of healthcare professionals due to documentation standards breaches can have significant implications for patient care and compliance. Poor documentation practices, including missing critical patient information or failing to follow established protocols, can result in compromised patient safety and potential legal liabilities. Specific cases might involve incidents where vital statistics are not recorded accurately within Electronic Health Records (EHR), leading to treatment errors. Compliance with documentation standards, as outlined by regulatory agencies like the Centers for Medicare & Medicaid Services (CMS), ensures the continuity of care and protects healthcare organizations from audit risks. Inconsistent documentation, particularly concerning medication administration or treatment plans, may prompt serious review actions or disciplinary measures against healthcare workers who fail to uphold these essential responsibilities.
Performance and Competency Evaluation
Healthcare professionals often face performance and competency evaluations to ensure quality care within institutions like hospitals or clinics. A comprehensive evaluation may include metrics such as patient satisfaction scores, adherence to medical guidelines, and clinical outcomes. For instance, a healthcare professional with a low patient satisfaction rating (below 75% in feedback surveys) might undergo further scrutiny. Specific incidents, like missed diagnoses or medication errors, also significantly impact evaluations. Ongoing training programs and mentorship initiatives aim to address competency issues and improve overall performance. In certain situations, a healthcare worker may receive a termination notice due to continued underperformance, emphasizing the need for adherence to established healthcare standards.
Letter Template For Healthcare Professional Termination Samples
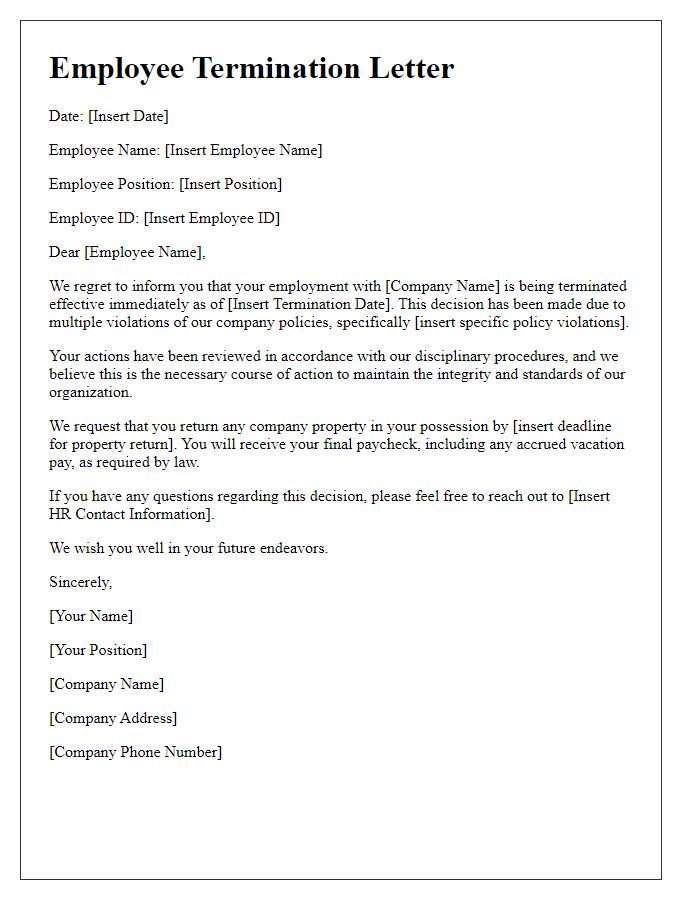
Letter template of employee termination for healthcare professionals due to policy violations
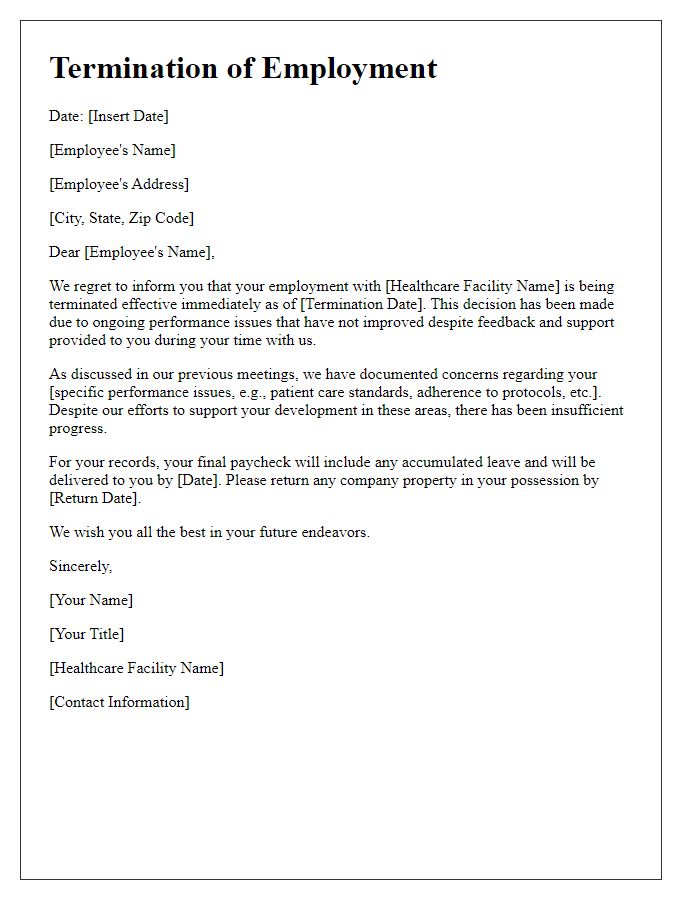
Letter template of termination for healthcare staff due to performance issues
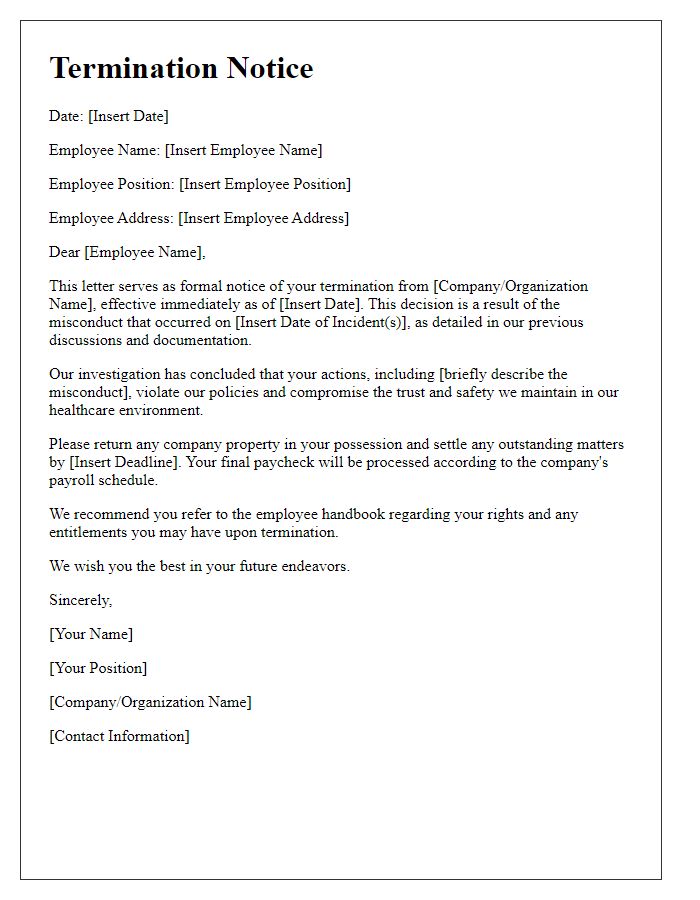
Letter template of termination notice for healthcare employees involved in misconduct
Letter template of resignation acceptance for healthcare professionals after termination discussion
Letter template of termination for healthcare workers due to budget cuts
Letter template of notification for healthcare professional termination with severance details
Letter template of immediate termination for healthcare employees after legal violations
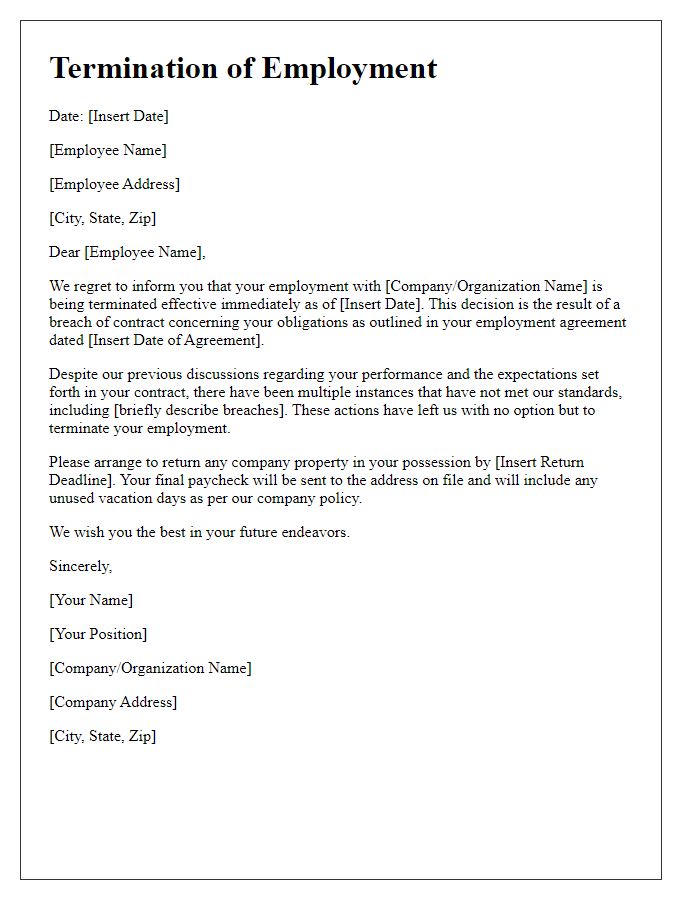
Letter template of formal termination for healthcare professionals due to breach of contract
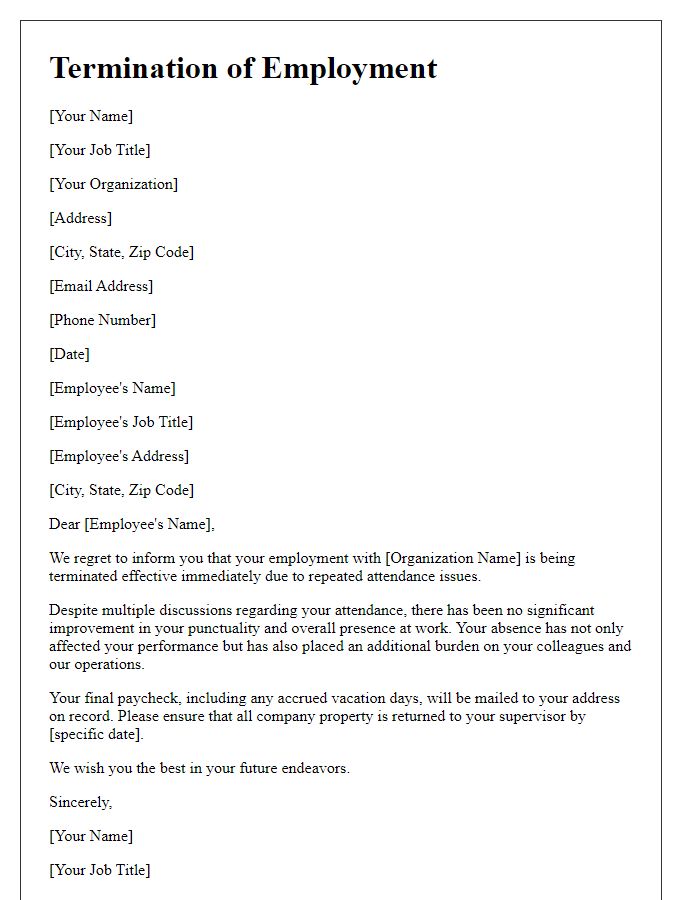
Letter template of termination for healthcare personnel over repeated attendance issues


Comments