Welcome to our guide on conducting a pharmaceutical service quality audit! In today's ever-evolving healthcare landscape, ensuring the highest standards of service quality is crucial not just for compliance but also for patient safety and satisfaction. Whether you're a seasoned professional or new to the field, understanding the intricacies of these audits will empower you to make informed decisions. Ready to dive deeper and enhance your pharmaceutical services? Let's explore more!
Purpose of the audit
The primary goal of a pharmaceutical service quality audit is to ensure compliance with industry regulations and standards, such as Good Manufacturing Practices (GMP) and Good Distribution Practices (GDP), which can affect patient safety and the efficacy of medications. This audit evaluates operational procedures, product storage conditions, and employee training programs within pharmaceutical facilities, which can significantly determine overall service quality. It examines critical areas such as inventory management, quality control processes, and documentation practices to identify areas for improvement. Additionally, the audit aims to enhance operational efficiency, minimize risks of non-compliance, and ultimately protect public health.
Audit scope and objectives
The pharmaceutical service quality audit encompasses a comprehensive evaluation of operational practices within the pharmaceutical sector, focusing on compliance with regulatory standards set by entities such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). The primary objectives of the audit include assessing the adherence to Good Manufacturing Practice (GMP) regulations, examining quality control processes, and identifying potential areas for improvement. Specific areas of focus include inventory management, warehouse conditions, documentation accuracy, and employee training protocols. Additionally, the audit aims to ensure that patient safety is prioritized while evaluating the efficacy of current service delivery methods. Through this rigorous assessment, the objective is to foster continuous improvement in pharmaceutical services that ultimately enhance patient care and uphold industry standards.
Information required from the service
Pharmaceutical service quality audits often require extensive information to ensure compliance and to assess overall operational effectiveness. Essential details include the audit date, location of the service, and the responsible personnel overseeing compliance measures. A detailed list of services provided, including medication dispensing, patient counseling, and inventory management practices, should be included. Documented standard operating procedures (SOPs) that govern these services are critical for evaluation. Details about medication storage conditions (temperature, humidity controls), security measures for controlled substances, and tracking mechanisms for adverse drug reactions must be provided. Information regarding staff training programs, certifications, and ongoing education interventions can offer insight into staff competency. Financial records related to pharmaceutical purchases, equipment maintenance logs, and records of previous audits assist in analyzing service performance over time. Results from patient satisfaction surveys and feedback mechanisms can provide valuable qualitative data on service quality. Finally, compliance with regulatory guidelines from governing bodies such as the Food and Drug Administration (FDA) or local health authorities is paramount to assess adherence to industry standards.
Schedule and timeline
A comprehensive pharmaceutical service quality audit entails a meticulous evaluation of operational protocols within a clinical setting, such as a hospital or pharmaceutical distribution center. The audit schedule typically spans several weeks, ensuring thorough inspections and assessments. Initial planning may occur in week one, including stakeholder meetings and resource allocation. Week two focuses on document review where relevant records and standard operating procedures (SOPs) are scrutinized for compliance with regulatory standards, such as the FDA's Good Manufacturing Practices (GMP). In week three, field observations and employee interviews occur, assessing practical application of quality measures. Finally, week four encompasses data analysis, where findings are compiled into a detailed report highlighting areas of excellence and opportunities for improvement, followed by the development of action plans for any identified deficiencies.
Contact information for questions
Pharmaceutical service quality audits are vital for ensuring compliance with regulations, such as the FDA's Good Manufacturing Practices (GMP). A structured contact information section, clearly detailing phone numbers, emails, and office hours, is essential for addressing inquiries related to the audit process. For example, a direct line to the Quality Assurance Manager could facilitate quick resolution of issues, while a dedicated email address enables streamlined communication. Specifying office hours, such as 9 AM to 5 PM EST on weekdays, can help stakeholders plan accordingly. Furthermore, including roles of contact personnel, such as compliance officers or regulatory affairs specialists, can enhance clarity and efficiency during the audit.
Letter Template For Pharmaceutical Service Quality Audit Samples
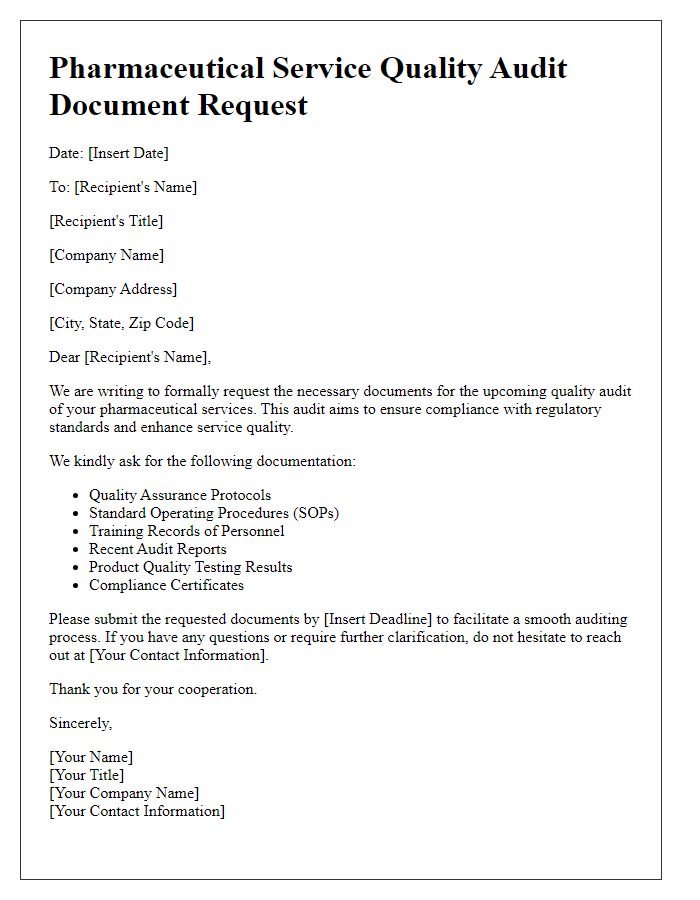
Letter template of pharmaceutical service quality audit request for documents
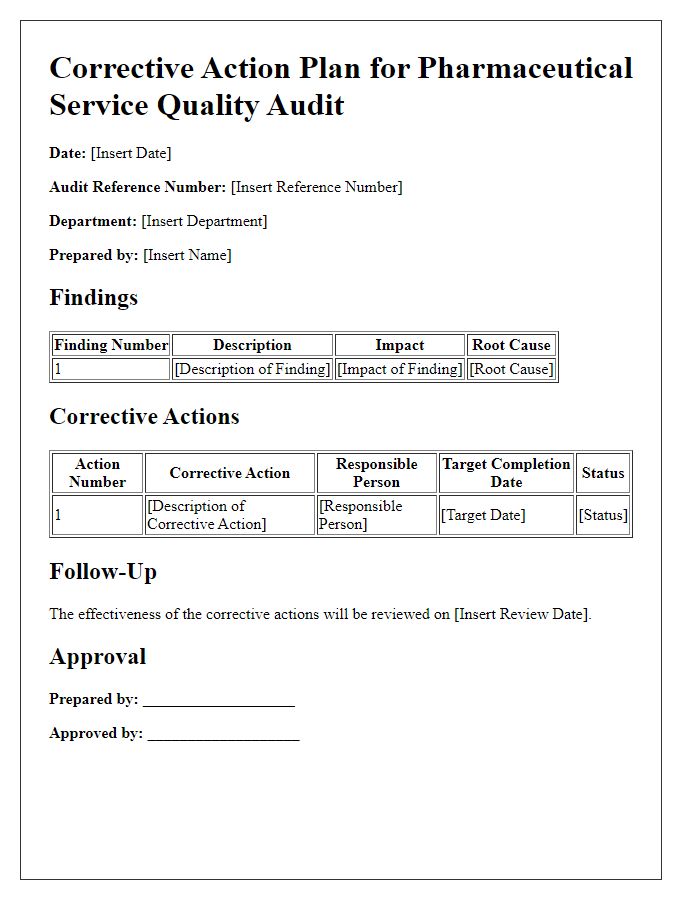
Letter template of pharmaceutical service quality audit corrective action plan


Comments