Are you curious about how your data can make a difference in clinical research? Sharing your clinical trial data not only contributes to scientific advancement but also enhances the integrity and transparency of medical studies. This simple act allows researchers to accelerate breakthroughs and improve patient care for all. If you're interested in learning more about the process and benefits of data sharing for clinical trials, read on!
Purpose and Scope of Data Sharing
Clinical trial data sharing aims to enhance scientific research by providing access to anonymized participant data, including demographic information, treatment outcomes, and adverse event reports. This practice supports transparency and collaboration within the medical community, allowing researchers to validate findings, conduct meta-analyses, or explore new hypotheses. The data shared includes information from clinical trials conducted at prestigious institutions such as the National Institutes of Health (NIH) and respected pharmaceutical companies globally. By participating in this initiative, stakeholders contribute to the advancement of medical science, ultimately benefitting public health and informing future clinical practices.
Confidentiality and Privacy Measures
Clinical trial data sharing involves strict confidentiality and privacy measures to protect participant information. Data anonymization techniques are employed, ensuring no personally identifiable information (PII) is included in shared datasets. Advanced encryption methods safeguard data during transmission and storage, adhering to regulatory standards, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States. Informed consent forms outline the specific uses of data, detailing potential risks and security measures. Research institutions implement access controls, restricting data access to authorized personnel only, further minimizing the risk of unauthorized disclosures. Continuous monitoring and auditing practices are established to ensure compliance with privacy regulations and maintain participant trust.
Voluntary Participation and Withdrawal Rights
Voluntary participation in clinical trials is crucial for advancing medical research. Participants must be fully informed that they can withdraw their consent at any time without any penalty or loss of benefits. This includes access to standard medical care, which continues irrespective of participation. Informed consent forms must clearly outline the purpose of the study, explaining how data will be used, and ensuring confidentiality of personal health information (PHI). Ethical guidelines promote respect for participants' autonomy, allowing for questions or concerns to be addressed by researchers readily. Research institutions, like the National Institutes of Health (NIH), emphasize the importance of transparency in the consent process to foster trust in scientific inquiry. Participants should feel empowered to make decisions regarding their involvement, knowing their rights regarding personal data and future contact.
Potential Risks and Benefits
Informed consent for clinical trial participation entails recognizing potential risks and benefits associated with data sharing. Participants may encounter risks, such as privacy breaches regarding personal health information, especially concerning sensitive data like genetic predispositions or chronic conditions. However, sharing aggregated data enhances research capabilities leading to advancements in medical knowledge, potentially benefiting future treatments for conditions like diabetes or cancer. Collaboration with reputable institutions, including academic centers like Johns Hopkins or pharmaceutical companies such as Pfizer, aims to maintain data confidentiality while maximizing public health outcomes. Ultimately, informed decision-making empowers participants to weigh individual risks against collective benefits to society.
Data Sharing and Access Procedures
Clinical trial data sharing necessitates robust consent procedures to ensure participant privacy and data integrity. Participants, typically enrolled in research studies at renowned institutions like Johns Hopkins University or the Mayo Clinic, must be informed about the nature of shared data, including anonymization methods employed to protect personal identifiers. The data, which may include sensitive health information, demographic details, and trial results, is often categorized under regulated frameworks such as the Health Insurance Portability and Accountability Act (HIPAA). Clear guidelines regarding who can access this data, such as researchers affiliated with FDA-approved studies, and the purpose of data use, must be delineated. Lastly, participants should be made aware of their rights regarding data withdrawal even after initial consent, emphasizing the ethical commitment of the research community to prioritize individual autonomy throughout the trial timeframe.
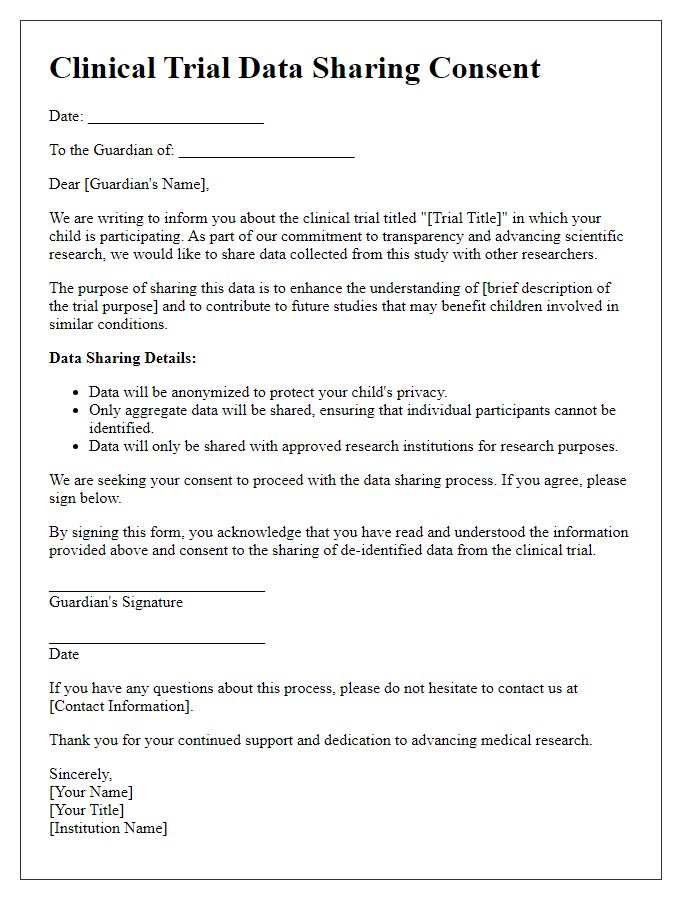
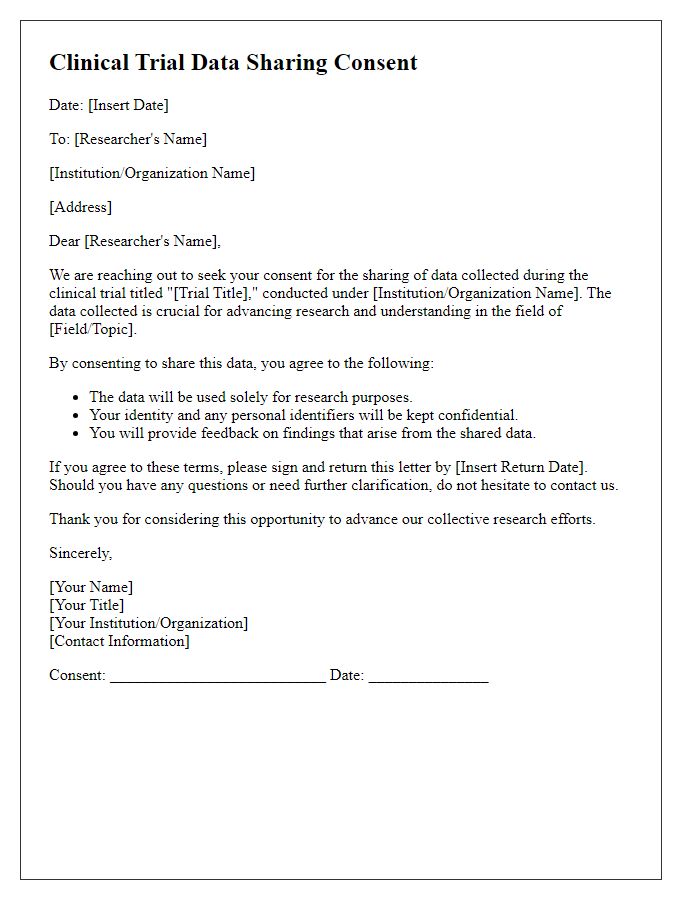
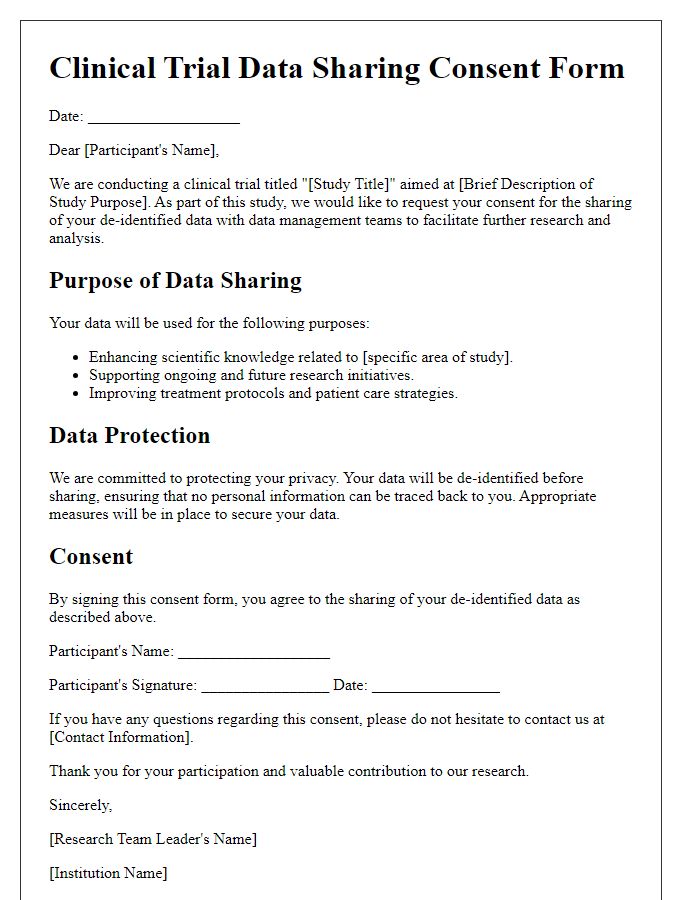
Letter Template For Clinical Trial Data Sharing Consent Samples
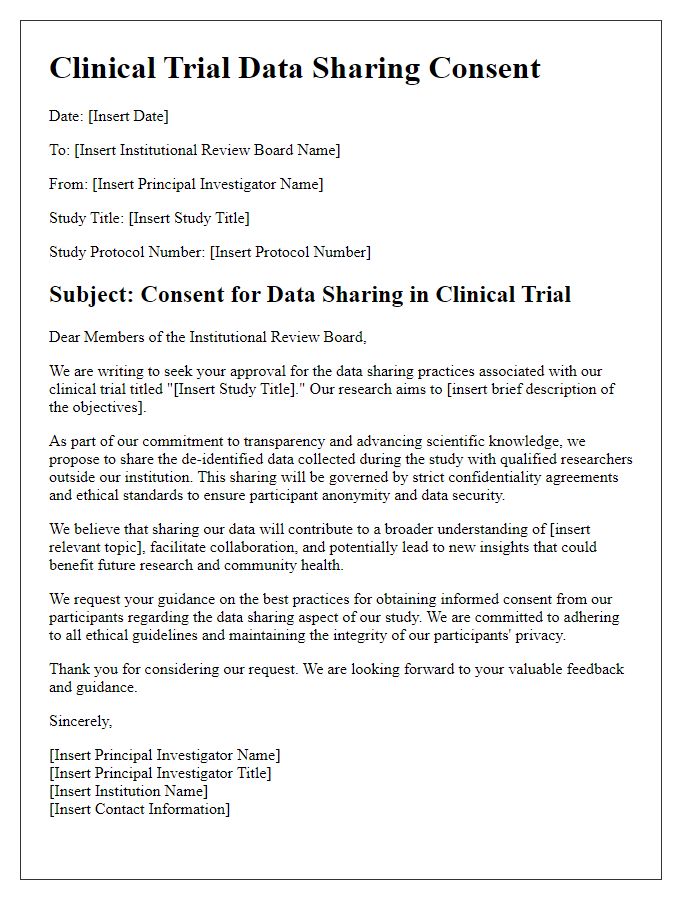
Letter template of clinical trial data sharing consent for institutional review boards
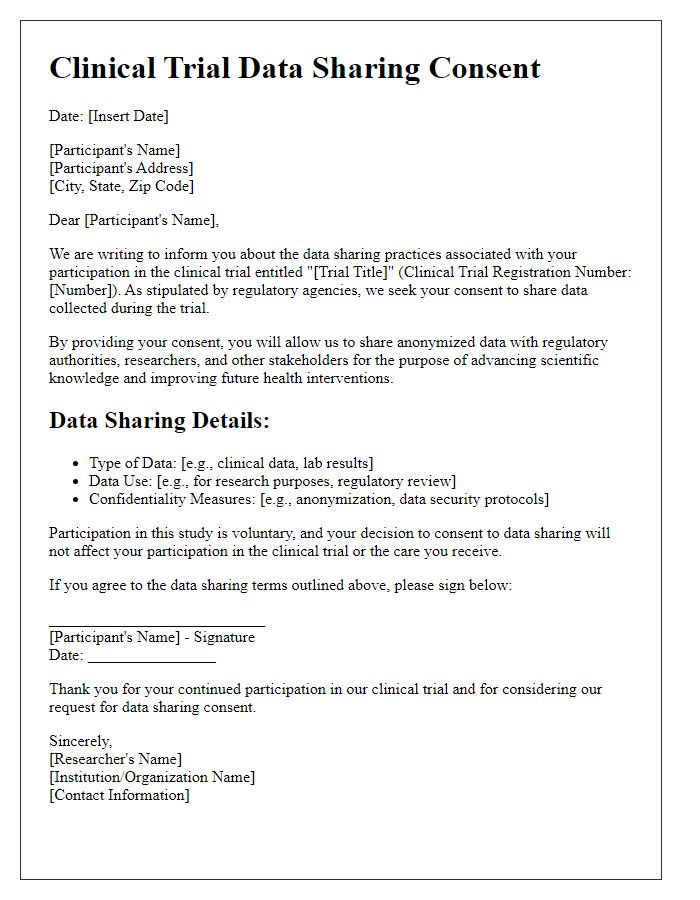
Letter template of clinical trial data sharing consent for regulatory agencies
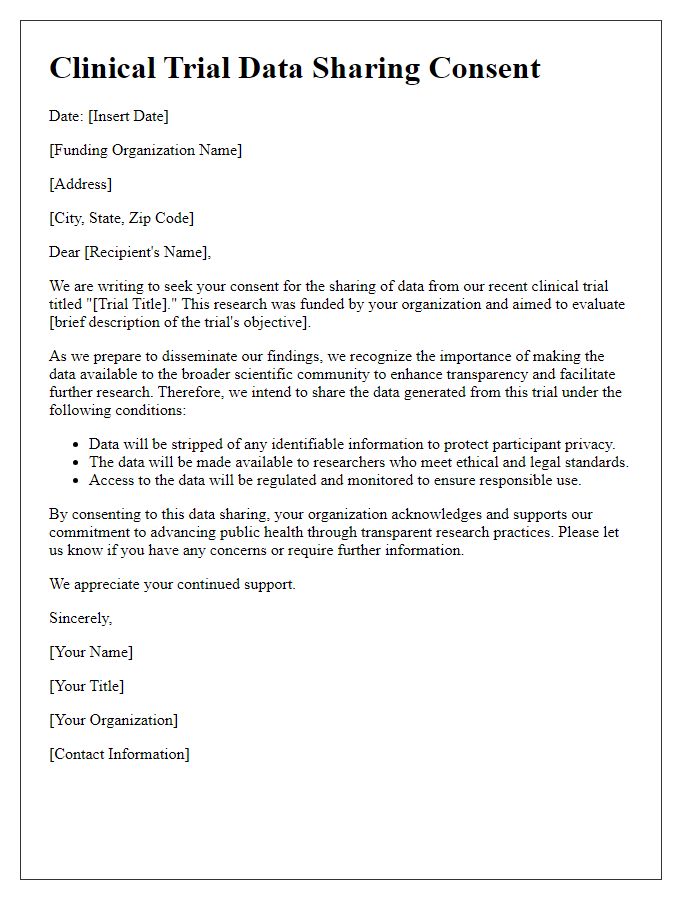
Letter template of clinical trial data sharing consent for funding organizations
Letter template of clinical trial data sharing consent for collaborators
Letter template of clinical trial data sharing consent for external auditors
Letter template of clinical trial data sharing consent for patient advocacy groups


Comments