Navigating medical bills can be a daunting task, especially when unexpected charges pop up that you believe are inaccurate. It's essential to understand your rights and the steps you can take to dispute these charges effectively. By crafting a clear and concise letter, you can articulate your concerns and potentially resolve the issue without further hassle. Ready to learn how to tackle your medical billing disputes? Read on for a detailed guide!
Clear Identification of Patient and Bill Information
Disputes regarding medical bill charges often begin with clear identification of the patient and the associated billing information. For effective communication, details such as the patient's full name (John Michael Smith), date of birth (January 15, 1985), and insurance policy number (ABC12345XYZ) are crucial. It is essential to include the date of service (March 30, 2023) and the specific procedure codes (CPT 99213 for an office visit) that have been billed. Additionally, referencing the billing statement number (Invoice #987654) and the total amount charged ($1,250.00) helps establish context for the dispute. Accurate documentation fosters a smoother resolution process.
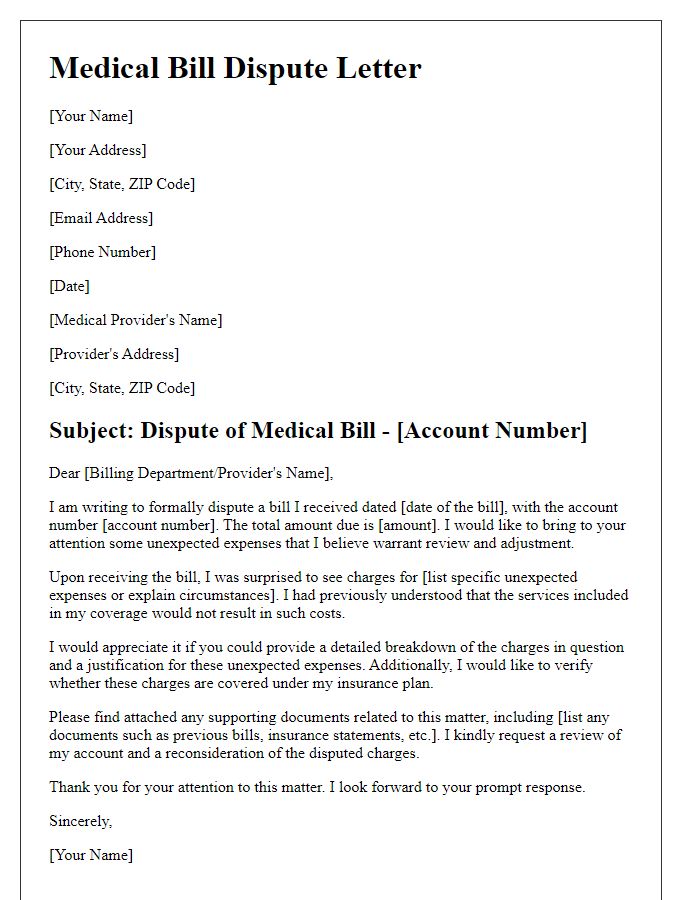
Detailed Explanation of Disputed Charges
Disputing medical bill charges often involves a thorough examination of specific fees associated with healthcare services provided. For example, an emergency room visit, coded under CPT code 99285, might include charges for consultations, diagnostic tests, and treatment supplies. If the billed amount exceeds the average cost of similar services in the region, such as those detailed by the Healthcare Cost and Utilization Project (HCUP), it may warrant a dispute. Additionally, discrepancies between the billed services and the insurance company's Explanation of Benefits (EOB) can arise; for instance, a patient may be charged for a procedure not performed, like a CT scan, which can typically range from $300 to $3,000 depending on facility fees. It's crucial to gather all relevant documents, such as the itemized bill from the healthcare provider, insurance policy details, and any prior communication regarding expected charges. This comprehensive approach ensures clarity and strengthens the case for disputing unjust charges.
Supporting Evidence or Documentation
Disputing medical bill charges often requires supporting evidence or documentation to substantiate the claim. Necessary documents include a detailed bill itemizing all charges, explanation of benefits (EOB) statements from insurance providers such as Blue Cross Blue Shield or Aetna, and medical records indicating the services received during visits at facilities like Johns Hopkins Hospital or Mayo Clinic. Additional proof might involve correspondence regarding pre-authorization or referral confirmations, which can clarify any discrepancies in billing. It is crucial to gather all related documents, ensuring each item reflects accurate services rendered, making a strong case against incorrect charges.
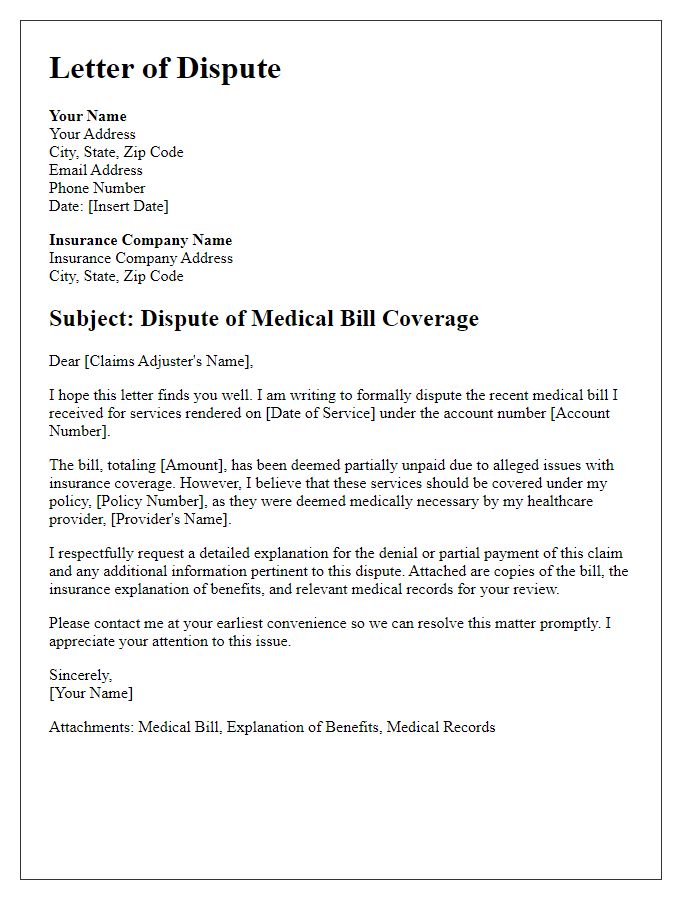
Request for Review and Adjustment
Medical billing disputes can arise due to errors or misunderstandings concerning charges on bills from healthcare providers. Common issues include discrepancies in charges for services rendered, incorrect billing codes, or failure to apply insurance coverage appropriately. A detailed review of the bill (including itemized charges) alongside supporting documents such as explanation of benefits (EOB) statements from insurance companies is crucial. Contacting the billing department of the healthcare facility (such as hospitals or clinics) or reaching out to patient advocacy organizations can aid in addressing these disputes. Prompt action within 30 to 60 days of receiving the bill is often recommended to ensure timely resolution and prevent further collection efforts. Documentation of all communications and agreements should be maintained for reference during the dispute process.
Contact Information and Follow-up Request
Disputing medical bill charges requires detailed attention to contact methods and follow-up strategies. Accurate contact information should include the medical provider's name, billing department phone number, and mailing address (for documentation purposes, typically found on the bill). Clearly state the specific charges in question, including service dates and procedure codes (such as CPT or ICD-10 codes) to support your claim. A follow-up request should detail timelines, indicating when to expect a response (generally within 30 days). Furthermore, emphasize the importance of resolving discrepancies before escalating the issue to government health agencies, such as the Centers for Medicare & Medicaid Services (CMS). Accurate documentation, such as previous statements and payment records, will further strengthen the dispute.
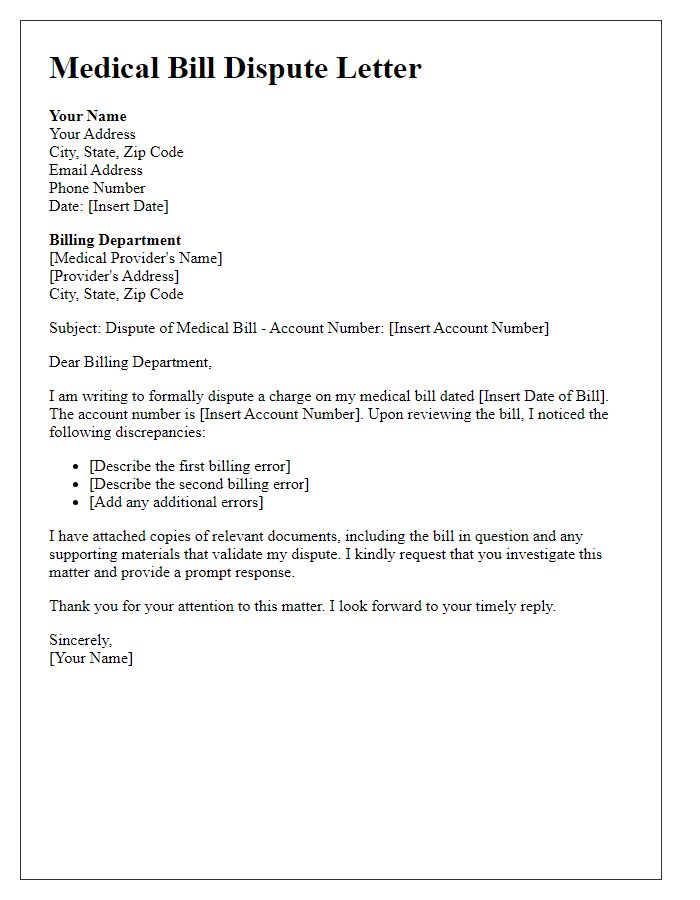
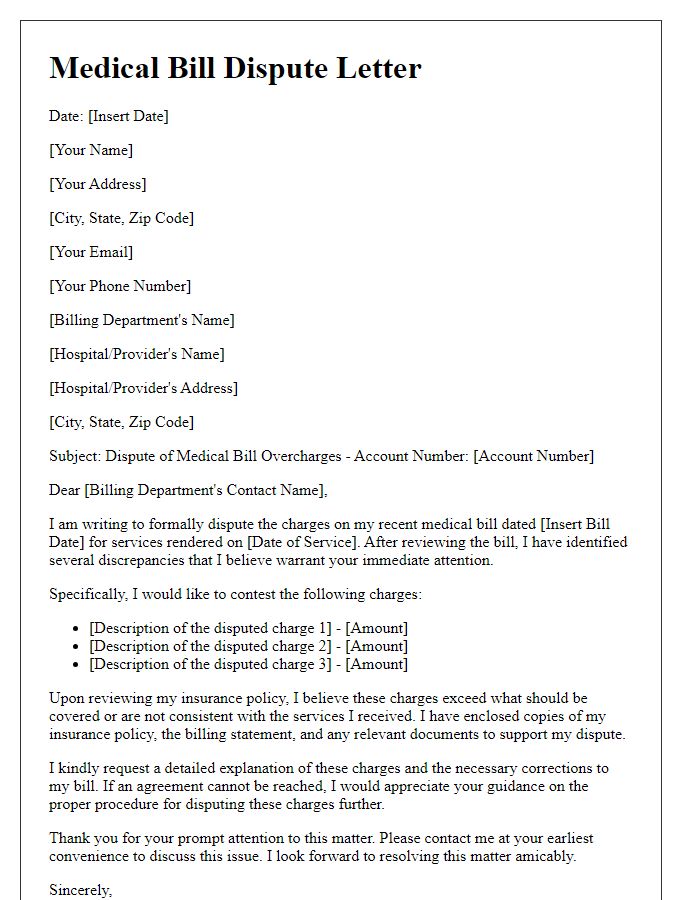
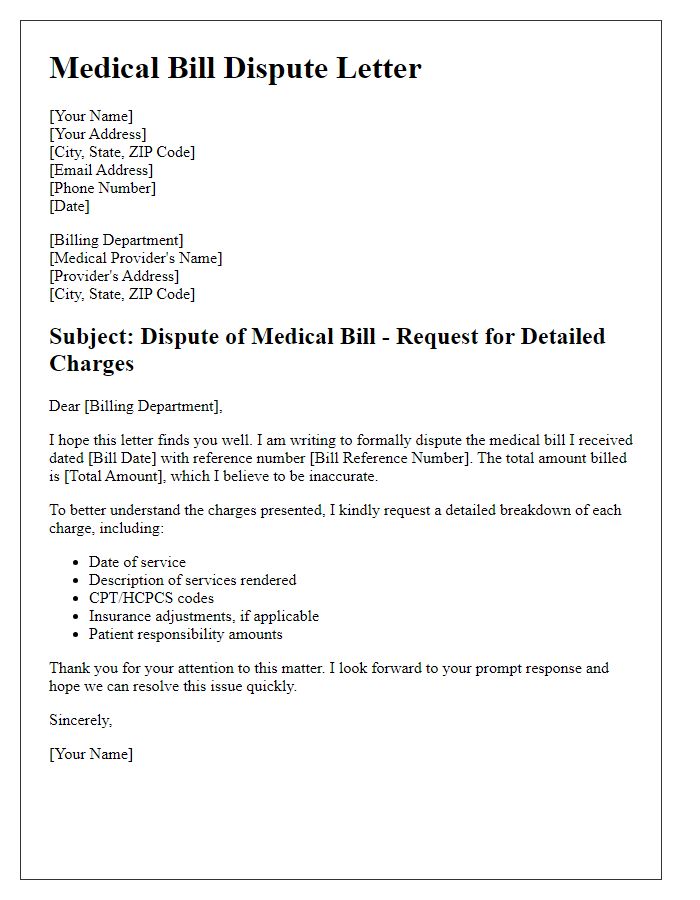
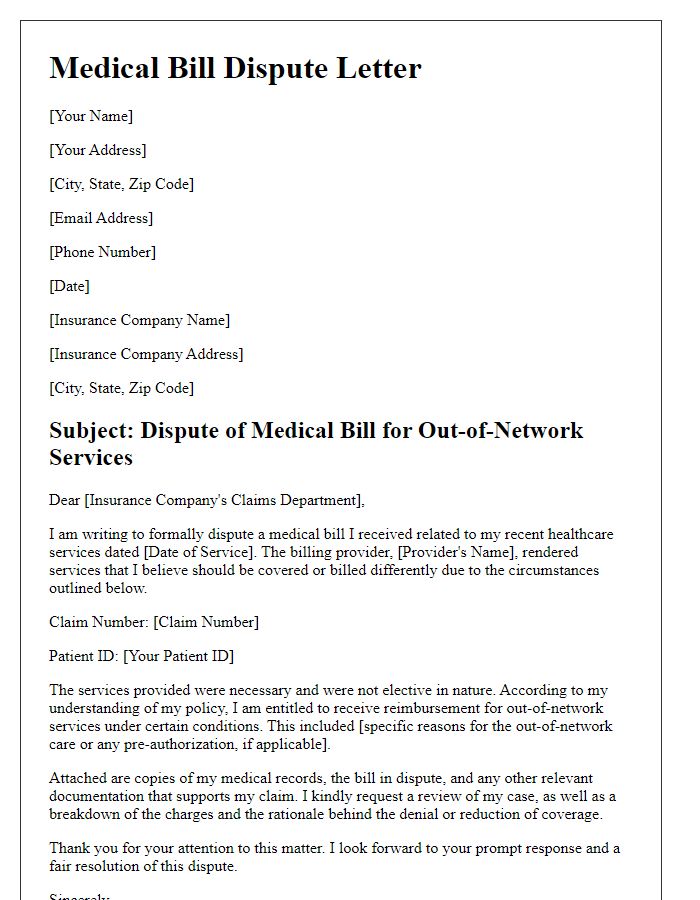
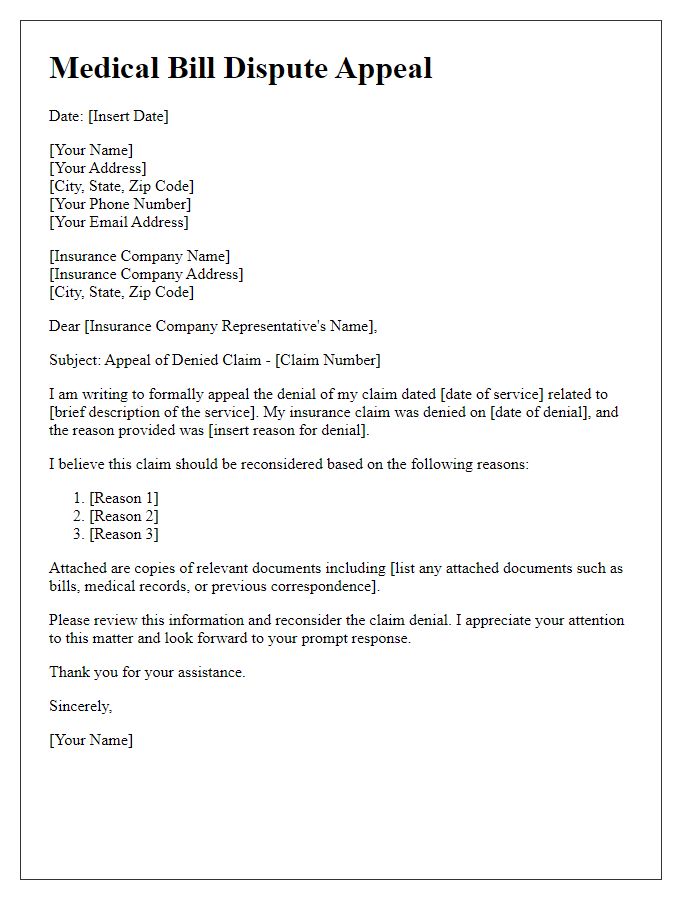
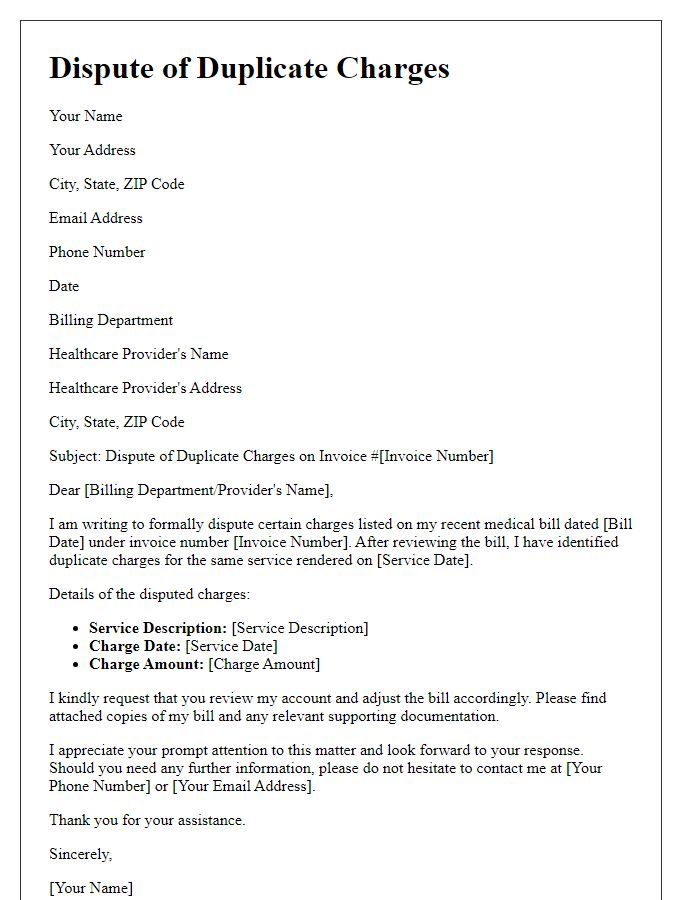
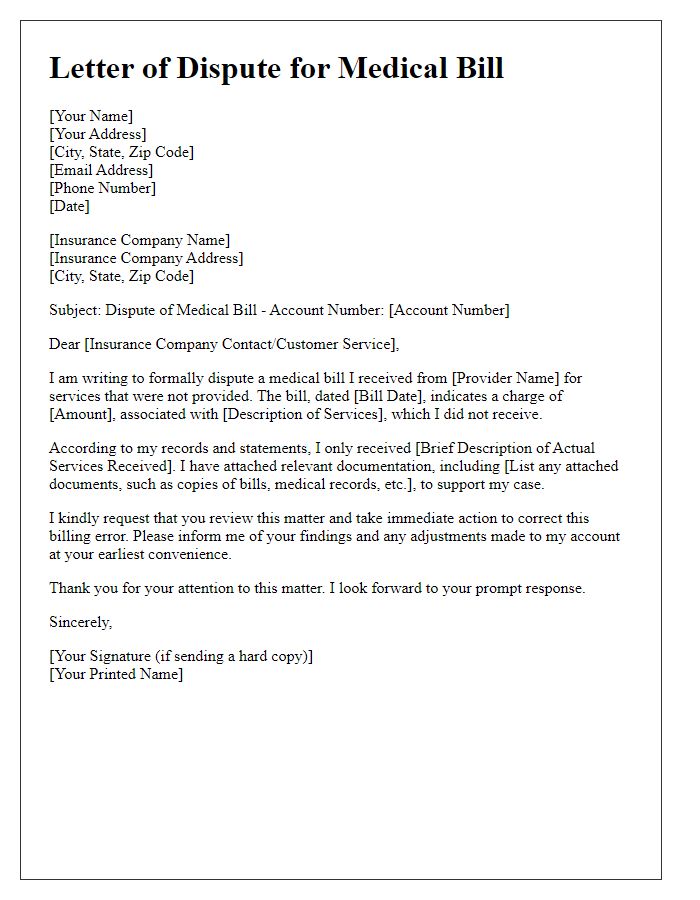
Letter Template For Disputing Medical Bill Charges Samples
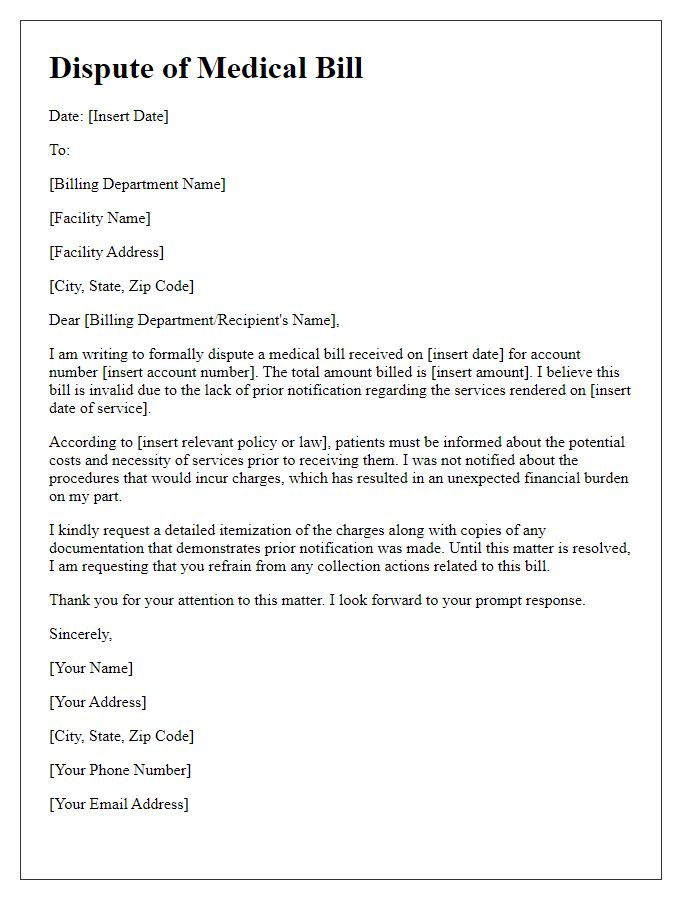
Letter template of medical bill dispute due to lack of prior notification



Comments