Are you frustrated with an incorrect medical diagnosis billing? You're not aloneâmany people find themselves in the same confusing situation when navigating healthcare costs. Understanding how to challenge these errors is crucial for protecting your finances and ensuring you get the care you deserve. In this article, we'll guide you through crafting a compelling letter template to contest those charges, so keep reading to learn more!
Patient Information: Name, contact details, insurance information.
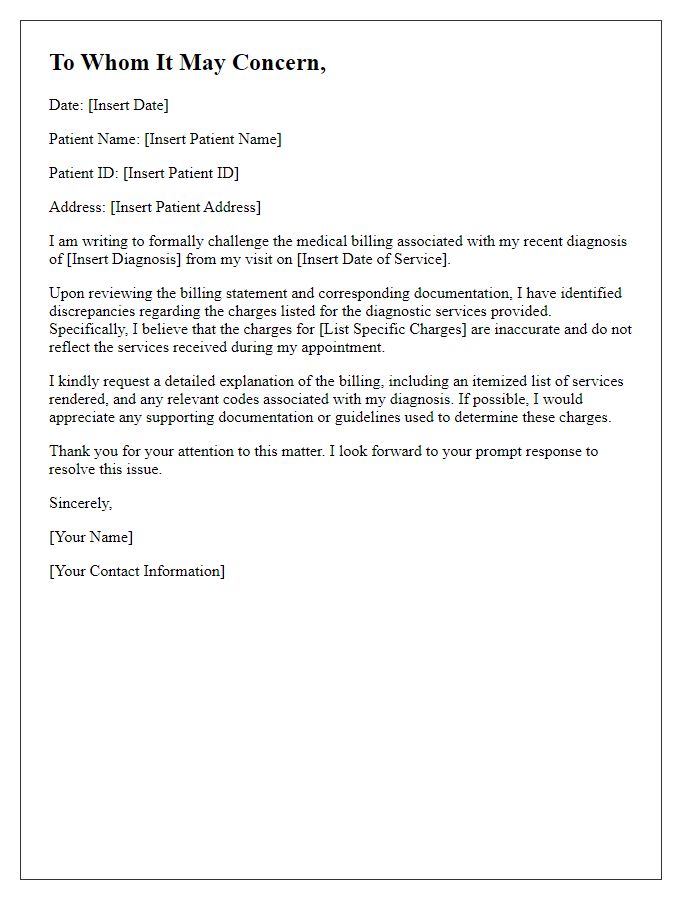
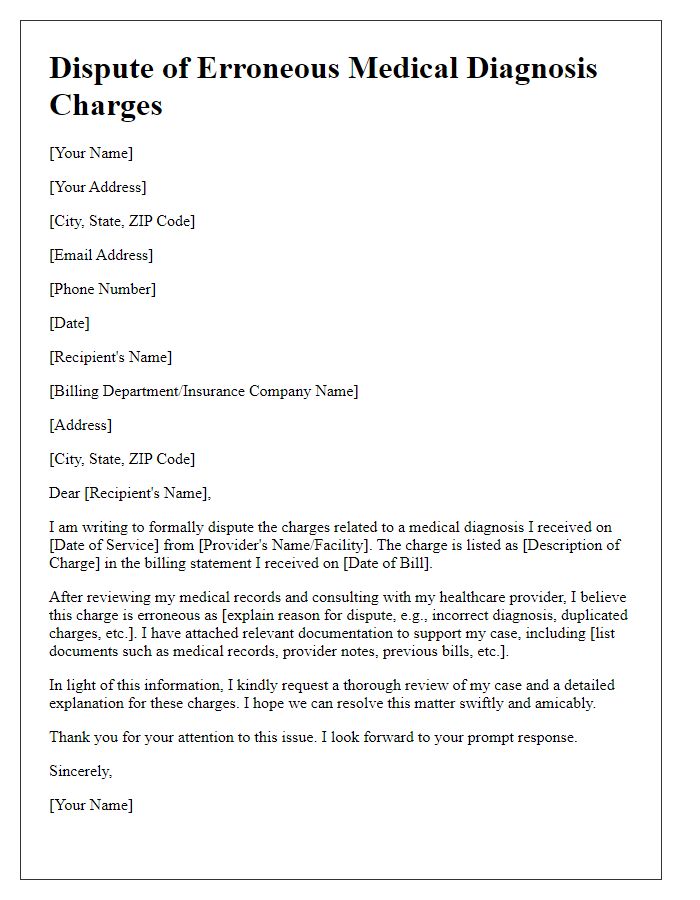
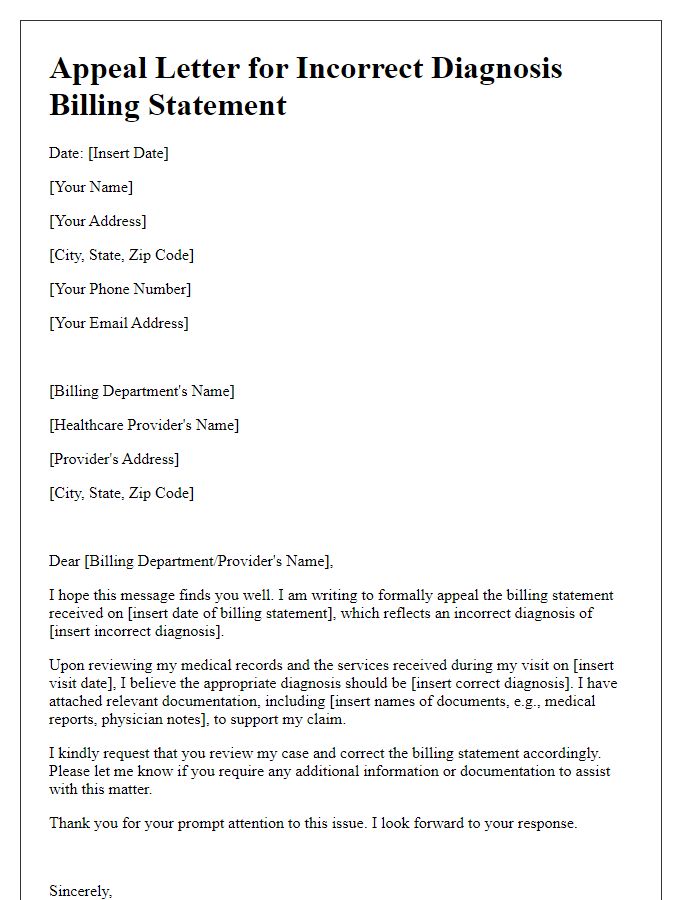
Patient information plays a vital role in contesting incorrect medical diagnosis billing associated with healthcare services. The patient's name (John Doe), contact details (123-456-7890, johndoe@email.com), and insurance information (XYZ Health Insurance, Policy #987654321) are crucial identifiers for verifying claims. Incorrect diagnosis coding, such as using ICD-10 codes (International Classification of Diseases, 10th Revision), can lead to billing discrepancies in healthcare facilities like St. Mary's Hospital. These discrepancies often result in inflated charges and insurance claim denials, affecting patients financially. Documenting specific treatment dates, medical history, and correspondence records enhances accuracy in contesting unjust charges, ensuring appropriate resolution and financial accountability.
Billing Details: Invoice number, date of service, charges in question.
Billing discrepancies can arise from incorrect medical diagnosis billing, leading to confusion and financial strain for patients. The invoice number (for example, #123456) dated September 15, 2023, outlines specific charges associated with a supposed treatment related to a medical condition (such as a bronchial infection). These charges in question (totaling $500) appear to have stemmed from an inaccurate code that misrepresented the actual diagnosis provided during the appointment. Clarity on each charge is crucial, as this directly impacts insurance coverage and out-of-pocket expenses. Correcting this billing error not only alleviates undue stress but also ensures accurate financial records and accountability within healthcare services.
Disputed Diagnosis: Clearly state the incorrect diagnosis.
Disputed Diagnosis involves asserting inaccuracies in medical billing relating to a specific diagnosis. For instance, a patient diagnosed with a common cold (ICD-10 code J00) may receive a bill indicating a more severe respiratory condition such as pneumonia (ICD-10 code J18). This misdiagnosis not only inflates potential out-of-pocket costs but also affects the patient's health records and insurance claims. Accurate billing is critical to ensure appropriate treatment is documented, ultimately impacting future care decisions. Emphasizing the importance of correct diagnostic codes (which can cost thousands) is essential in contesting the billing discrepancies effectively.
Supporting Evidence: Medical records, doctor's note, test results.
Contesting an incorrect medical diagnosis billing requires a detailed approach supported by specific evidence. Medical records, which provide a comprehensive overview of patient history, treatment plans, and previous consultations, are crucial for substantiating claims. A doctor's note, detailing the practitioner's findings and recommendations, serves as a vital piece of documentation to validate the accuracy of the diagnosis. Test results, including lab analyses or imaging reports such as X-rays or MRIs, can offer concrete evidence of the patient's condition and demonstrate discrepancies in the billing statement. Collectively, these documents play an essential role in addressing billing inaccuracies and enforcing accountability from medical providers.
Request for Resolution: Desired outcome, contact for further discussion.
Inaccurate medical diagnosis billing can create significant financial strain for patients, leading to disputes with healthcare providers. Incorrect coding (such as using the wrong ICD-10 codes) can result in overcharges or denials from insurance companies, exacerbating the patient's situation. Documentation errors in medical records, such as misrepresented diagnosis or treatment details, can also contribute to billing inaccuracies. Patients often seek resolution through clear and concise communication with billing departments, requesting itemized statements and explanations for charges. Desired outcomes may include corrected billing or reimbursement for overcharged amounts, while offering availability for further discussion aids in resolving misunderstandings swiftly and effectively.
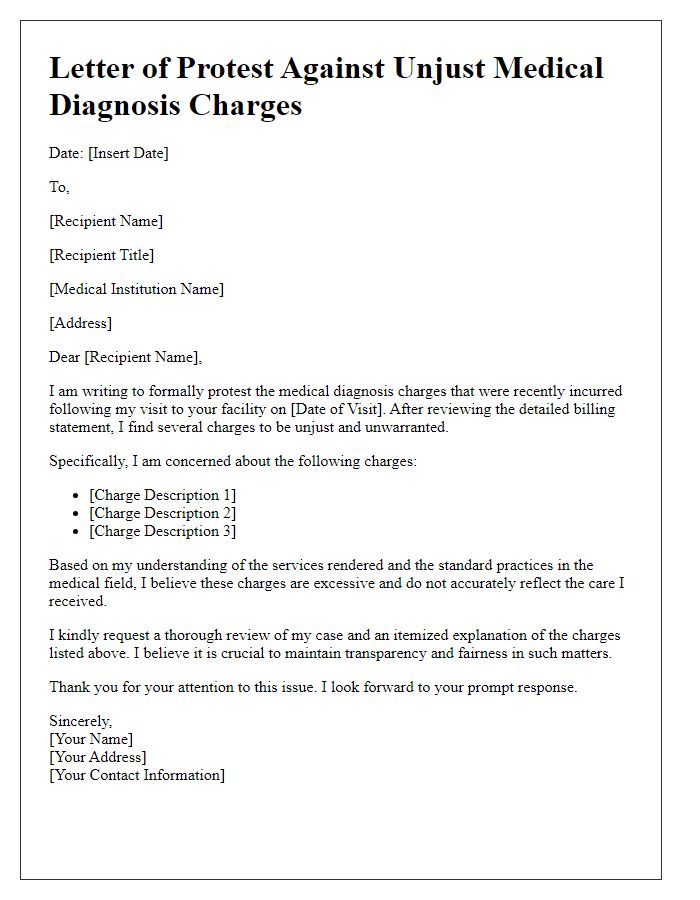
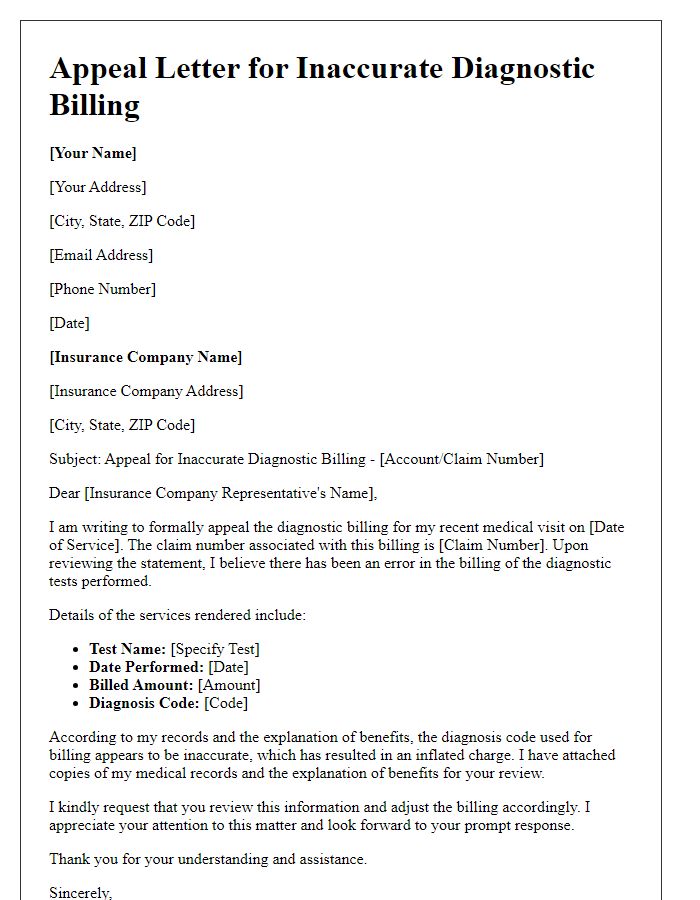
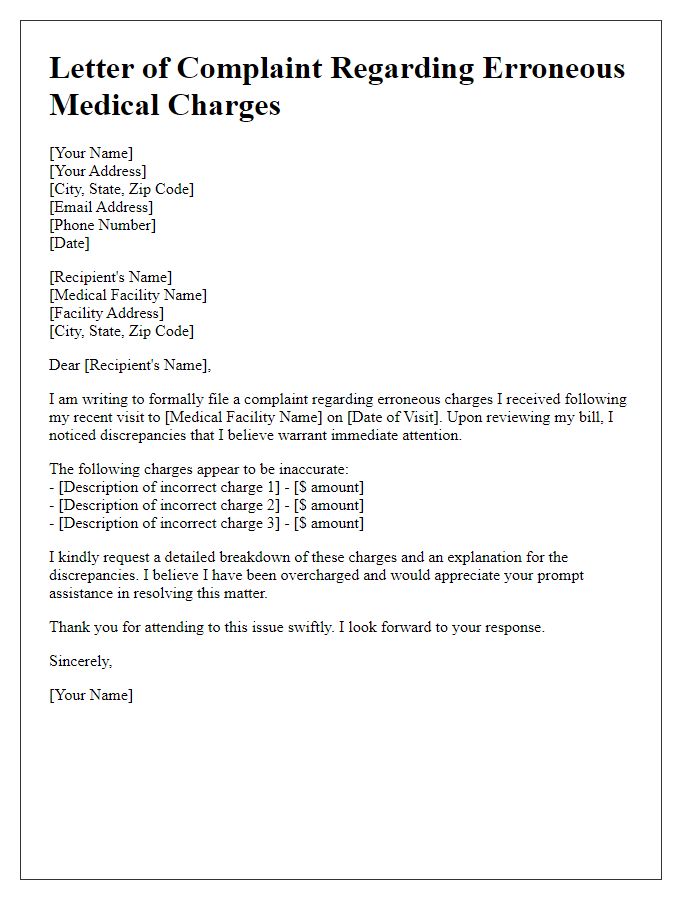
Letter Template For Contesting Incorrect Medical Diagnosis Billing Samples
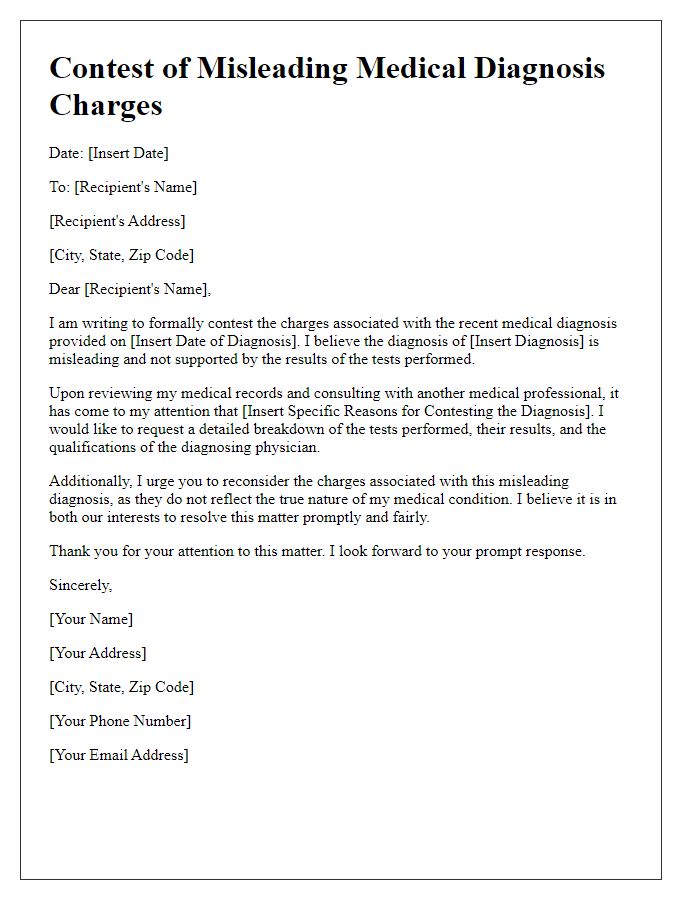
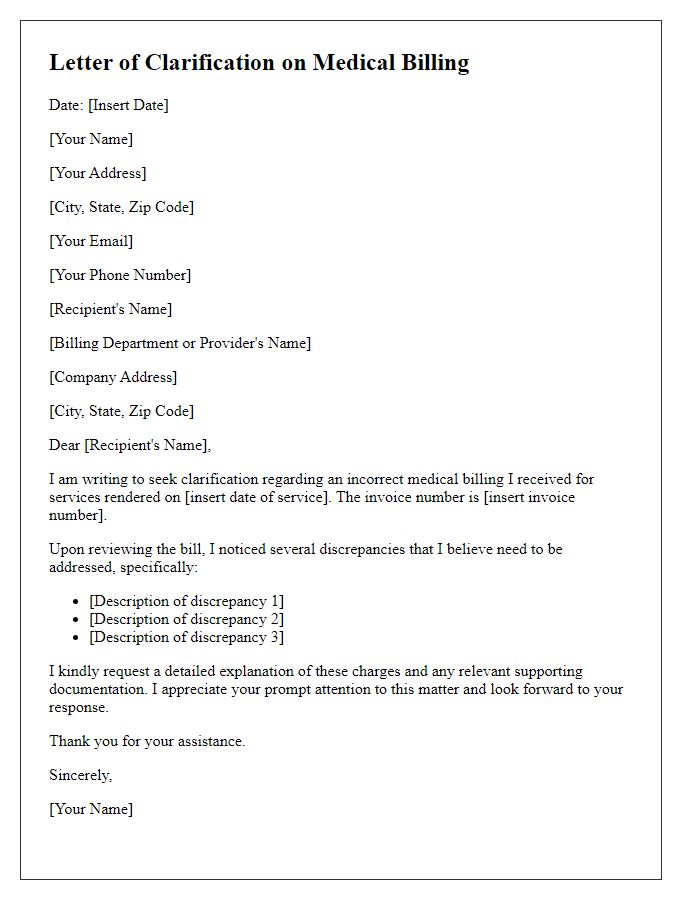
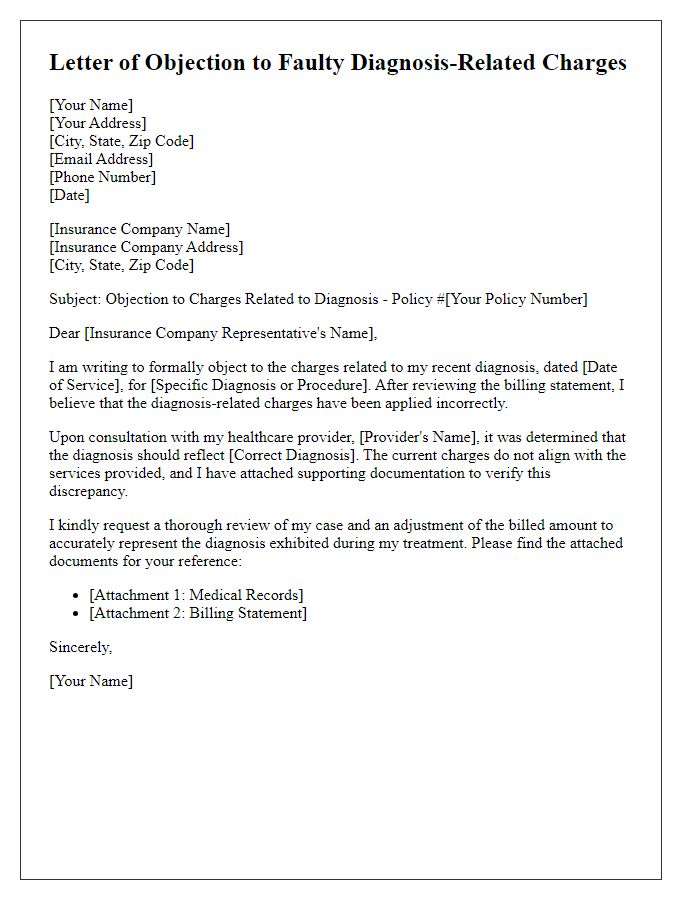
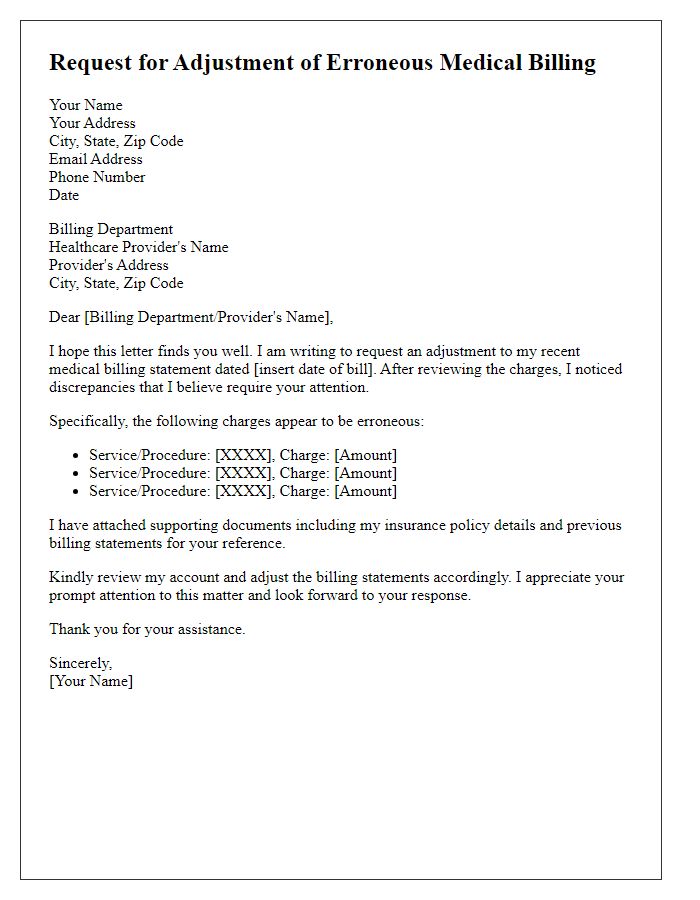
Letter template of challenging inaccurate medical billing for diagnosis.



Comments