Hey there! Are you ready to navigate the world of healthcare enrollment? It can be a bit overwhelming, but we're here to simplify the process for you. From understanding your options to ensuring you meet essential deadlines, this guide will help you make informed decisions about your health coverage. So, let's dive in and explore all the important details you need to know!
Clear subject line
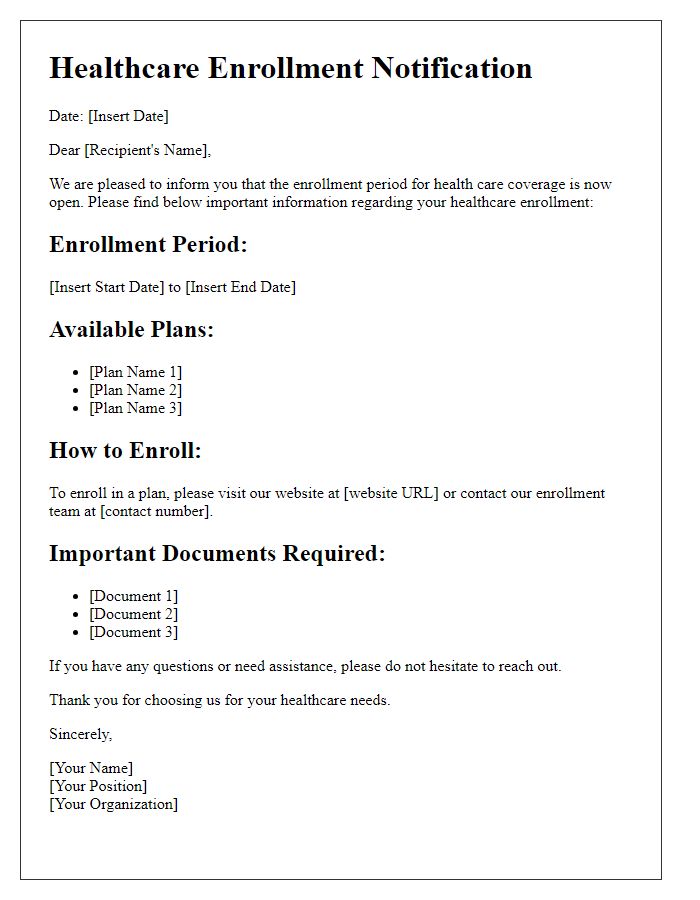
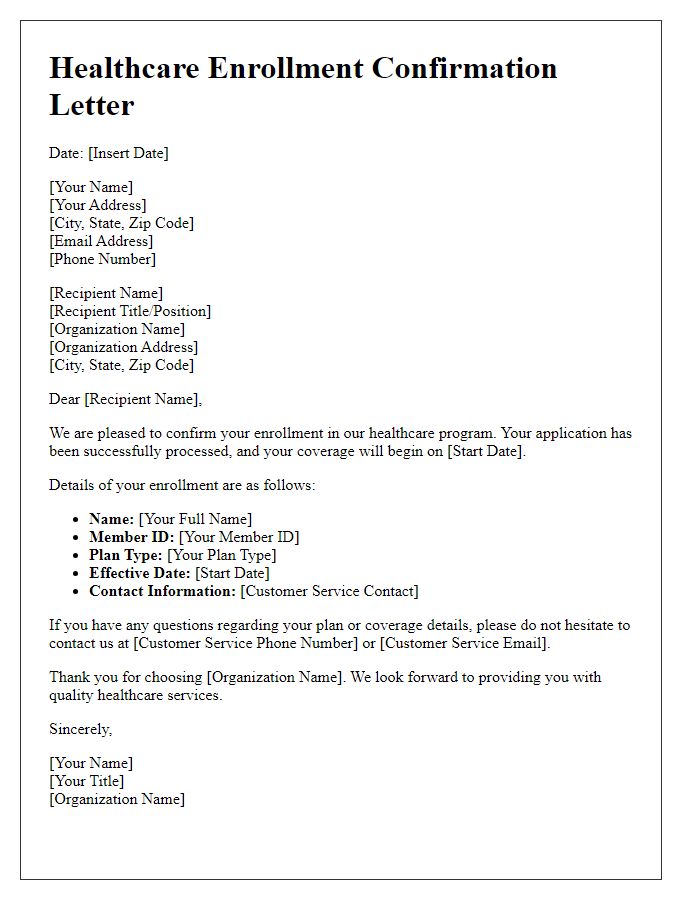
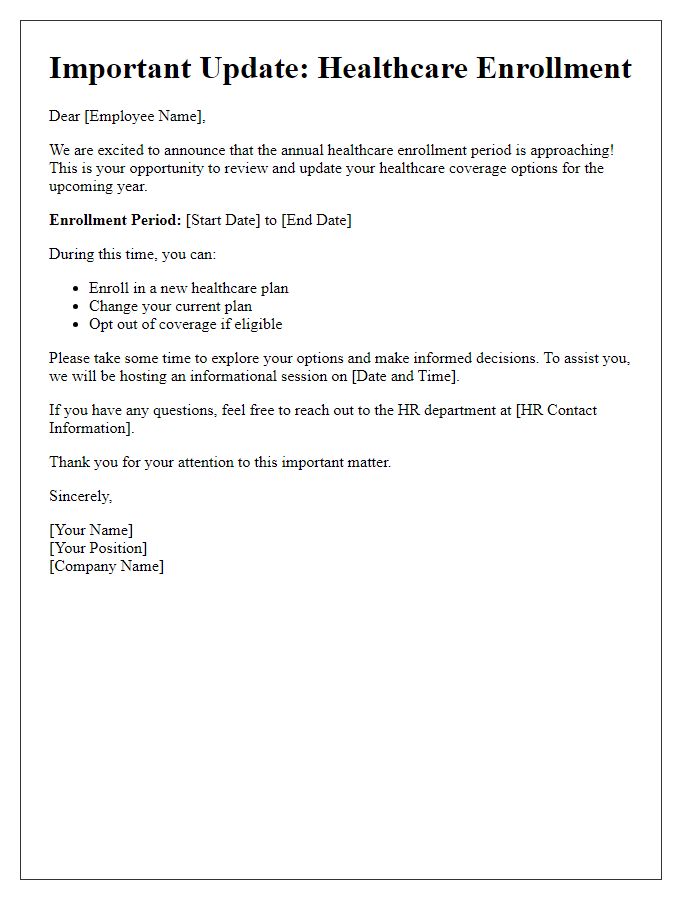
Healthcare enrollment notices provide essential information about upcoming opportunities to enroll in health insurance plans. Notifications are typically sent during the annual enrollment period (often between November 1 to December 15 in the United States). These notices detail important deadlines, eligibility criteria, and plan options. Individuals may need to review specific plan benefits, premiums, and coverage networks, as well as ensure compliance with the Affordable Care Act (ACA) requirements. Enrollments can take place through online marketplaces or state exchanges, emphasizing the importance of timely engagement in the enrollment process to avoid gaps in coverage.
Personalized greeting
A healthcare enrollment notice is an important communication that provides individuals with information about their health insurance options. The notice typically includes details about enrollment periods, coverage options, and instructions for obtaining and completing necessary paperwork. For example, the notice might explain that open enrollment for the Affordable Care Act (ACA) typically occurs from November 1st to December 15th each year, urging individuals to review plans available in their state, such as the various tiers of coverage (Bronze, Silver, Gold, Platinum) offered through healthcare marketplaces. It may also highlight eligibility criteria for Medicaid or Children's Health Insurance Program (CHIP) and emphasize the importance of timely enrollment to avoid gaps in coverage. The notice's personalized greeting can enhance engagement and encourage individuals to take immediate action, ensuring they secure adequate healthcare without delays.
Enrollment details and deadlines
Enrollment for healthcare plans requires attention to key dates and specific options. Open enrollment periods typically begin on November 1 and end on December 15 each year, providing individuals and families the chance to select or change their healthcare plans. Applicants must review different coverage options available through state exchanges or private insurers, including preferred provider organizations (PPOs) and health maintenance organizations (HMOs). It's crucial to gather necessary documentation such as income verification and proof of residency before starting the enrollment process. Failure to enroll within this designated window could result in a lack of health coverage until the next enrollment period, potentially affecting access to essential medical services.
Benefits and coverage information
Healthcare enrollment notices inform beneficiaries about essential benefits and coverage options available under their health plans. These documents outline specific details, including types of services covered (such as preventive care, emergency services, and prescription drugs), network providers (hospitals, clinics, and specialists), and cost-sharing information (premium rates, deductibles, and co-pays). Important deadlines for enrollment periods are also highlighted to ensure timely registration. Furthermore, each notice may include contact information for customer service representatives or online portals where individuals can manage their plans, update personal information, and review policy documentation, ensuring accessibility to crucial health resources.
Contact information for questions
Healthcare enrollment notifications are crucial for individuals to understand their coverage options. Contact information sections within these notices typically include phone numbers, email addresses, or online resources for inquiries. Important details might consist of dedicated customer service hours, often between 8 AM to 6 PM, local time, and availability of multilingual support. Highlighting specific department contacts, such as claims assistance or eligibility verification teams, enhances clarity. Registered members may also find links to official websites for comprehensive FAQs, enrollment forms, and policy documents, ensuring they can access essential guidance throughout the enrollment process.


Comments