Are you exploring the journey of fertility treatment and feeling a bit overwhelmed? You're not alone; countless individuals and couples find themselves navigating this complex landscape of emotions and medical choices. In this article, we'll break down essential components, tips, and insights into creating a personalized fertility treatment plan that suits your unique needs. So, let's dive in and empower you with the knowledge to take your next steps with confidence!
Personal Information Collection
Creating a detailed fertility treatment plan requires careful collection of personal information to ensure tailored care. Initial data includes full name, date of birth, and contact information, crucial for maintaining communication during the treatment journey. Medical history forms should encompass past reproductive health, previous pregnancies (including live births or miscarriages), and any prior fertility treatments experienced. Lifestyle factors must be documented, such as smoking habits, alcohol consumption, exercise routines, and dietary preferences, as these can significantly influence reproductive health. Additionally, partner information should be included, outlining their health history and lifestyle habits. Lastly, any relevant family medical history concerning genetic disorders or reproductive issues should also be gathered to assess potential risks and develop a comprehensive treatment strategy.
Treatment Schedule Outline
The fertility treatment plan for assisted reproductive technologies, such as In Vitro Fertilization (IVF), involves a comprehensive schedule. The initial consultation at the fertility clinic typically occurs within the first week of the menstrual cycle, usually Day 1, when hormone levels are assessed through blood tests. During the second week, between Days 6 to 10, ovarian stimulation begins with hormonal injections, such as Follicle Stimulating Hormone (FSH), to encourage the development of multiple follicles. Monitoring appointments, including blood work and ultrasounds, occur every few days during this phase to evaluate follicular growth and estrogen levels. Once optimal follicle size is reached, typically around Day 12 to 14, a trigger shot of Human Chorionic Gonadotropin (hCG) is administered to facilitate ovulation. Subsequently, egg retrieval is scheduled approximately 36 hours after the trigger shot, performed at the fertility clinic under anesthesia. Following egg retrieval, laboratory processes involve fertilization, with embryo transfer planned based on embryo development, usually between Days 3 to 5 after retrieval. A follow-up blood test for pregnancy is conducted approximately 10 to 14 days post-transfer to confirm successful implantation and pregnancy status. This structured timeline ensures close monitoring and management for potential adjustments needed throughout the process.
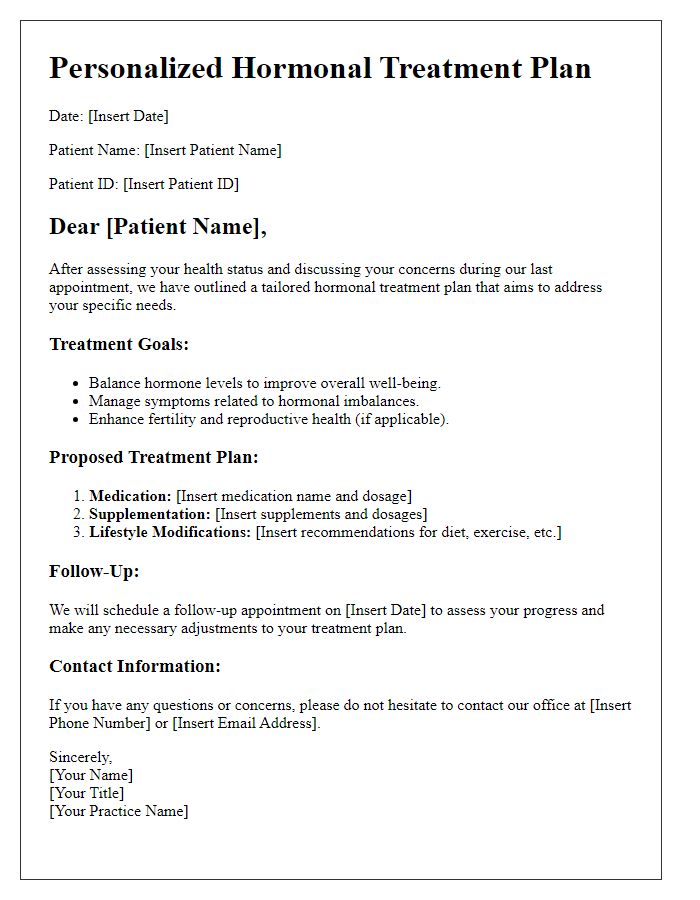
Medication and Dosage Details
A comprehensive fertility treatment plan typically includes crucial medication details for patients seeking assisted reproductive technologies such as In Vitro Fertilization (IVF). Medications like Gonadotropins (e.g., Follistim, Gonal-F) are essential for stimulating ovarian follicle development, administered via subcutaneous injections, often starting around Day 2 or 3 of the menstrual cycle. Dosages can vary, typically ranging from 150 to 450 International Units per day, depending on individual hormone levels evaluated during baseline ultrasounds and blood tests. Additionally, a medication like Lupron may be included to prevent premature ovulation, usually administered at 0.5 to 1 milligram per day. After ovulation induction, patients may require a trigger shot, such as Ovidrel, which contains choriogonadotropin alpha and is administered as a single subcutaneous injection 36 hours before egg retrieval. Progesterone supplements, such as Endometrin or PIO (Progesterone in Oil), are also crucial for uterine lining support post-ovulation, typically starting on the day of embryo transfer. Regular monitoring through ultrasounds and blood tests ensures proper medication efficacy and adjustments to dosages if necessary.
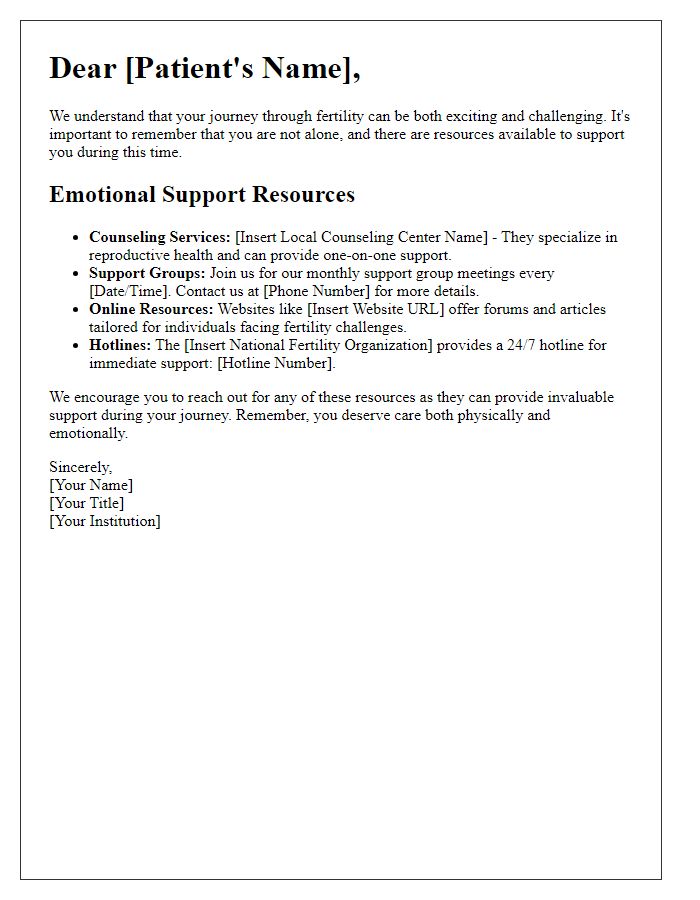
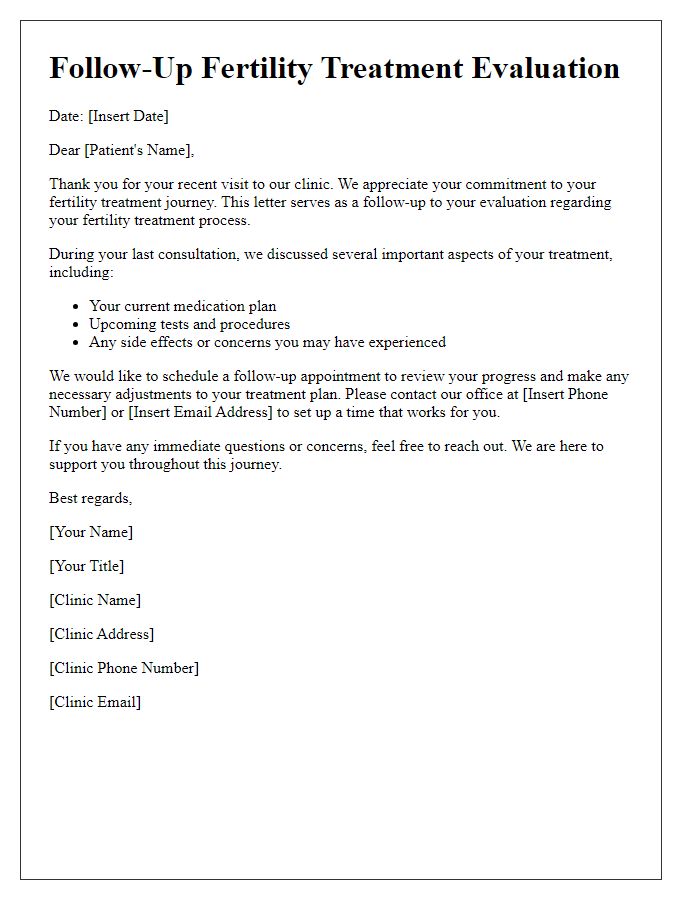
Monitoring and Follow-Up Appointments
Monitoring and follow-up appointments play a critical role in the success of fertility treatment plans, which often involve procedures such as in vitro fertilization (IVF) or intrauterine insemination (IUI). Regular monitoring involves blood tests to measure hormone levels, such as estradiol and progesterone, as well as ultrasounds to assess ovarian response and follicle development. These appointments typically occur at key intervals, often every few days during the stimulation phase, and can take place at specialized fertility clinics, ensuring close supervision by skilled reproductive endocrinologists. Patients should expect follow-up consultations to review treatment progress and adjust medication dosages, with the aim of optimizing outcomes. In addition to physical assessments, emotional support may also be provided during these sessions, addressing the psychological aspects of the treatment journey.
Contact Information for Medical Queries
For patients seeking assistance with fertility treatment, contacting the reproductive health clinic is essential. The clinic's phone number is typically listed as (555) 123-4567, operating from 8 AM to 5 PM, Monday through Friday. For medical inquiries, the clinic may provide an email address, such as info@fertilityclinic.com, ensuring that patients can reach out for guidance or clarification regarding their treatment plans. Patients should also consider visiting the clinic's website, which often contains comprehensive resources and FAQs about fertility options and procedures, contributing to well-informed decision-making. Furthermore, physical address details, like 123 Healthway Drive, Fertility City, can assist in scheduling in-person consultations for more personalized discussions.
Letter Template For Patient Fertility Treatment Plan Samples
Letter template of fertility assessment and treatment roadmap for patients.
Letter template of individualized fertility counseling summary for patients.


Comments