When it comes to your health, understanding your family history can be a game changer. Knowing if certain conditions run in your family helps healthcare providers tailor preventive measures and personalized treatment plans just for you. This article will guide you through the importance of maintaining an accurate patient family history record and how it can impact your medical care. So, stick around and discover more about why this information is vital for your well-being!
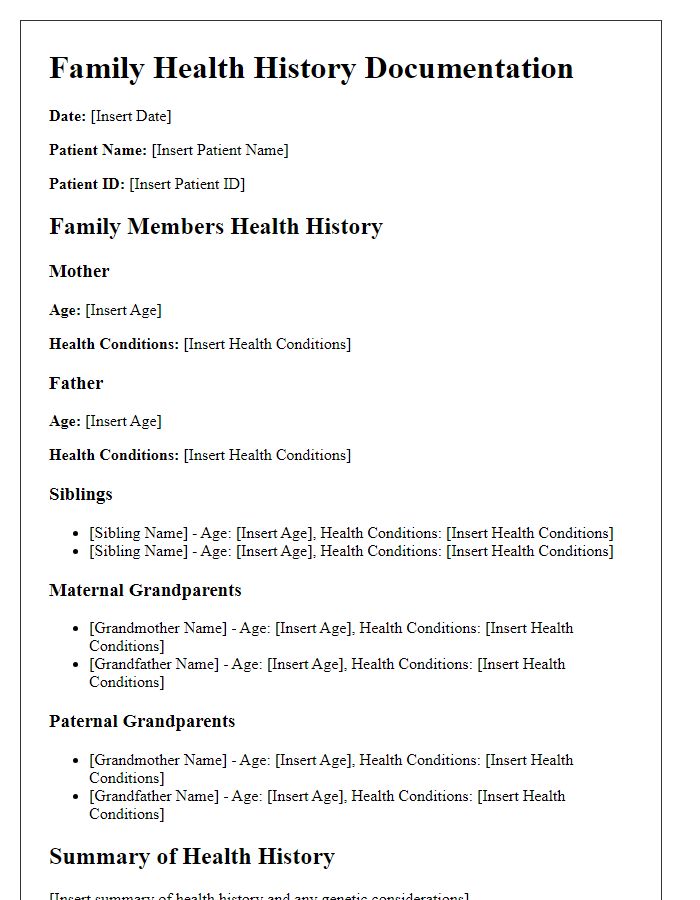
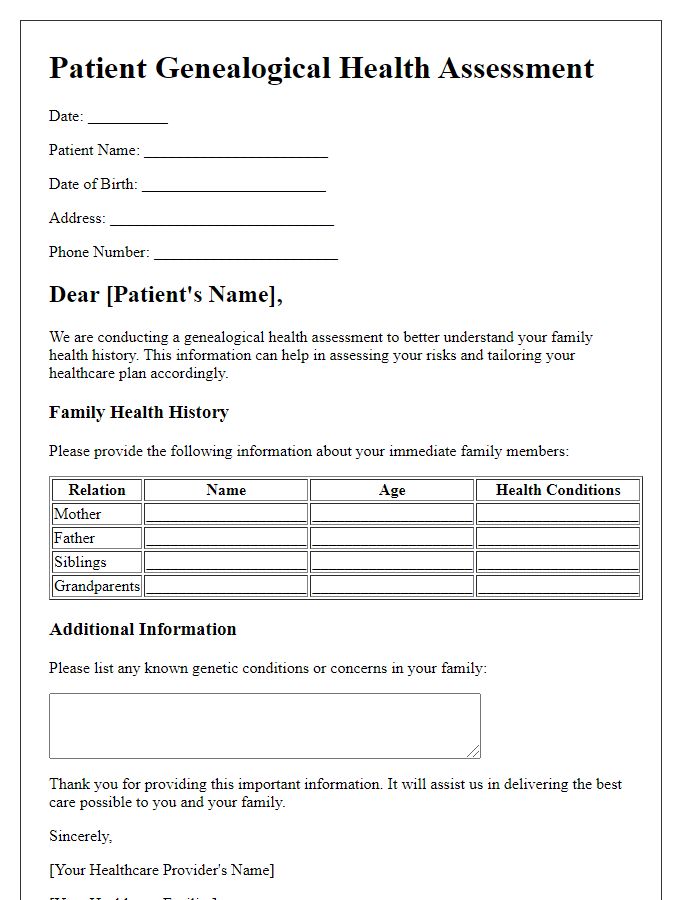
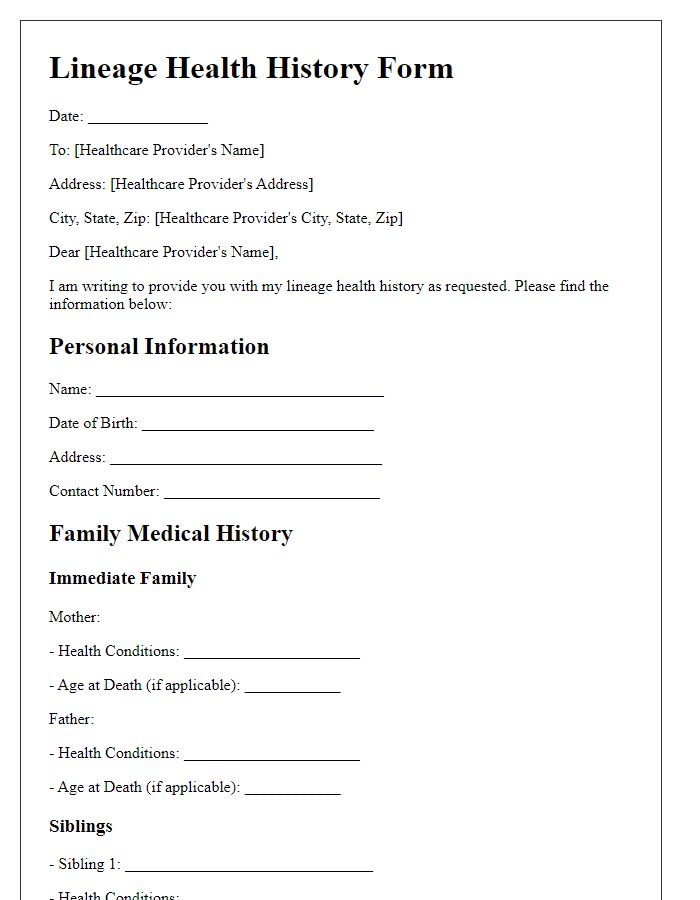
Patient Identification Information
Patient identification information encompasses essential details that provide context and clarity regarding individual medical histories. Key elements include the patient's full name, such as John Smith, gender, male, date of birth, January 15, 1985, and current residence, 123 Elm Street, Springfield, IL. Medical record number, often a unique identifier assigned by healthcare institutions, such as 987654321, ensures accurate tracking of patient information. Additionally, include contact information, including phone number, (555) 123-4567, and emergency contact details, like Jane Smith, relation: sister, phone number: (555) 987-6543. Lastly, capturing demographic data such as ethnicity, American, and insurance information, for example, Blue Cross Blue Shield, is crucial for comprehensive family medical history records.
Family Member Relationships
Family history plays a crucial role in understanding an individual's health risks and conditions. It is essential to document relationships accurately, such as parents (biological or adoptive), siblings (brothers and sisters), and grandparents (maternal and paternal). Details about the health status of these family members provide insight into hereditary diseases, such as diabetes or heart conditions. For instance, a first-degree relative, like a parent or sibling, can significantly increase the likelihood of developing conditions like breast cancer, especially when diagnosed before the age of 50. Additionally, mental health issues, such as bipolar disorder or schizophrenia, often have familial patterns worth noting. The family structure, including aunts, uncles, and cousins, can also reveal relevant health trends, contributing to a more comprehensive understanding of genetic predispositions.
Medical History and Conditions
Comprehensive family medical history plays a crucial role in understanding potential health risks. This record includes vital details about hereditary conditions, such as diabetes mellitus (affecting over 422 million people globally), heart disease (responsible for 17.9 million deaths annually), and certain cancers. The familial lineage should document incidences of conditions like breast cancer (with a noted BRCA1/BRCA2 gene mutation association), hypertension (impacting nearly 1.13 billion adults worldwide), and autoimmune disorders such as rheumatoid arthritis. Disease manifestation ages, treatments received, and outcomes are essential data points for assessing genetic predispositions. Significant lifestyle factors, like smoking (linked to 8 million deaths yearly) and obesity rates (nearly 650 million adults classified as obese), should also be included to enhance predictive health assessments. Accurate and detailed records facilitate personalized preventive care and early interventions for at-risk individuals.
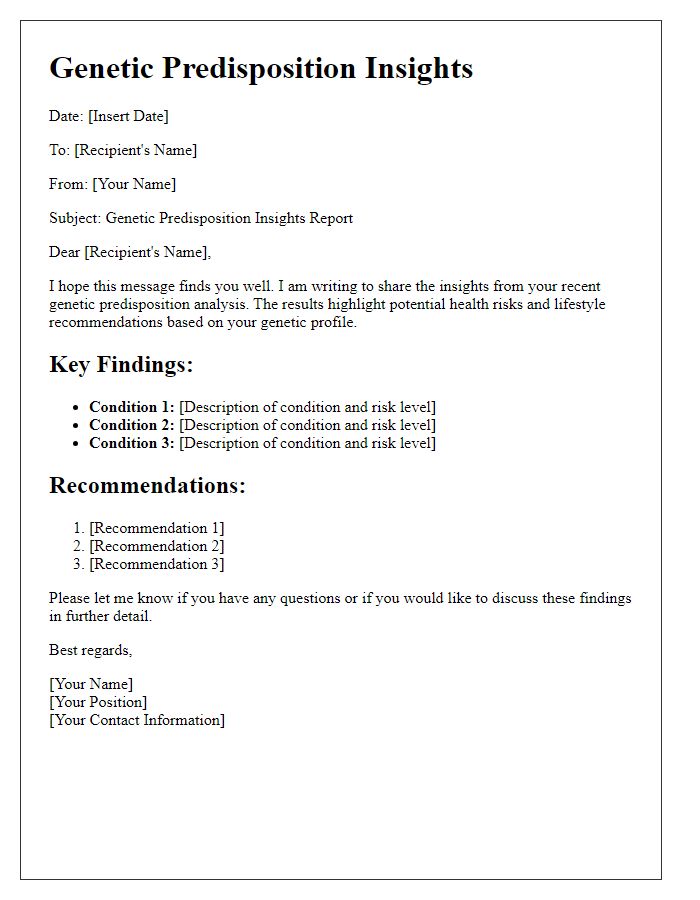
Genetic Disorder Indicators
Genetic disorder indicators, such as family history of conditions like cystic fibrosis or Huntington's disease, often require thorough documentation for accurate assessment and diagnosis. Each affected family member, including parents, siblings, and extended relatives, should be noted with specific details regarding age of onset, severity, and outcomes. For example, cystic fibrosis has a prevalence of approximately 1 in 3,500 births in Caucasian populations. Other hereditary conditions, like sickle cell anemia or hemophilia, also necessitate documentation, revealing specific patterns of inheritance such as autosomal recessive or X-linked, respectively. Home environments, lifestyle choices, and external factors influencing health, such as exposure to toxins or dietary habits, should also be included to provide comprehensive insight into genetic risk factors.
Lifestyle and Environmental Factors
Lifestyle and environmental factors significantly influence health outcomes, especially in relation to a person's family history. Regular physical activity, defined as 150 minutes of moderate-intensity exercise weekly, can lower the risk of chronic diseases such as type 2 diabetes and cardiovascular diseases. Nutrition plays a critical role, with guidelines recommending a diet rich in fruits, vegetables, whole grains, and lean proteins, while limiting processed foods, sugars, and saturated fats. Environmental exposure to pollutants, like fine particulate matter (PM2.5) and hazardous substances, found in areas with industrial activity or heavy traffic, can heighten the risk of respiratory diseases and cancers. Family lifestyle habits, including smoking and alcohol consumption patterns, can also affect genetic predispositions, increasing susceptibility to various conditions. Additionally, the impact of socio-economic status, access to healthcare, and educational opportunities contributes to overall health, shaping life choices that influence both current well-being and future health trajectories.

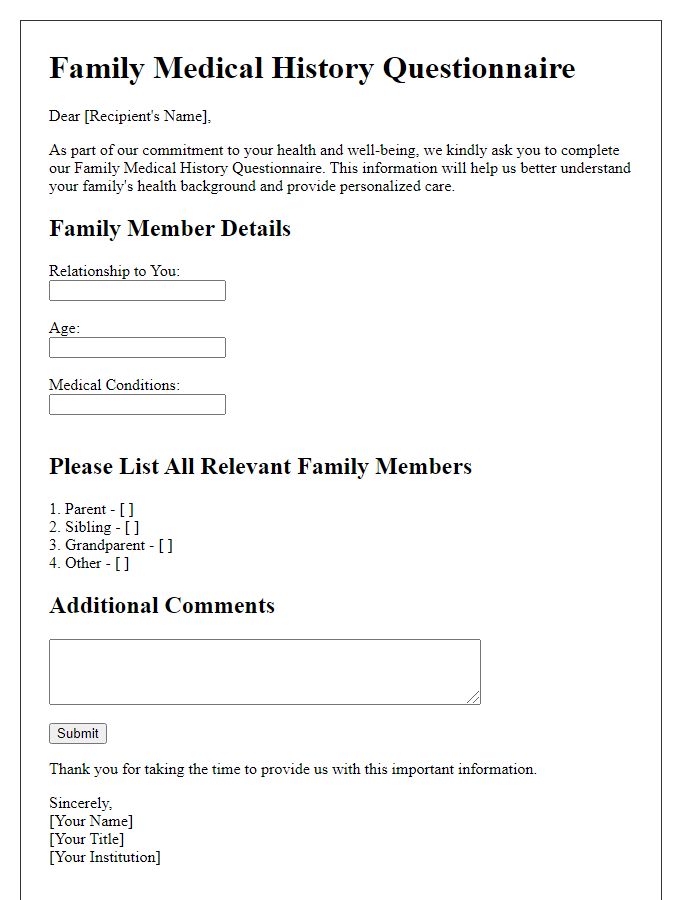
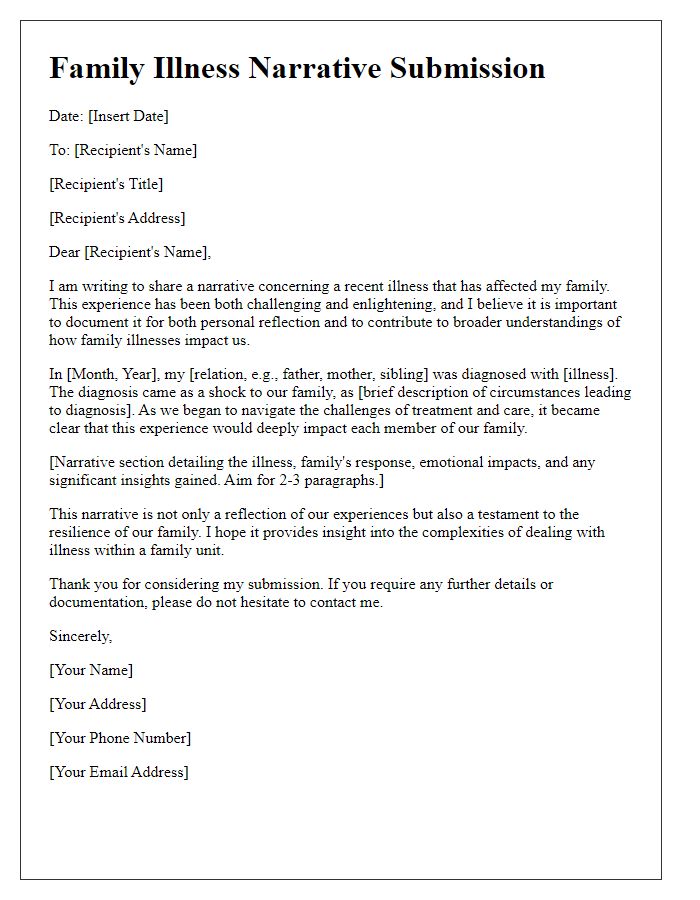

Comments