Are you looking to streamline the process of sending a medical referral request? Writing a clear and concise letter can make all the difference in ensuring your patient receives timely care. In our latest article, we'll explore essential components to include in your referral request, tips for maintaining professionalism, and how to follow up effectively. So, grab a cup of coffee and dive in for insights that will enhance your communication with medical specialists!
Patient Information
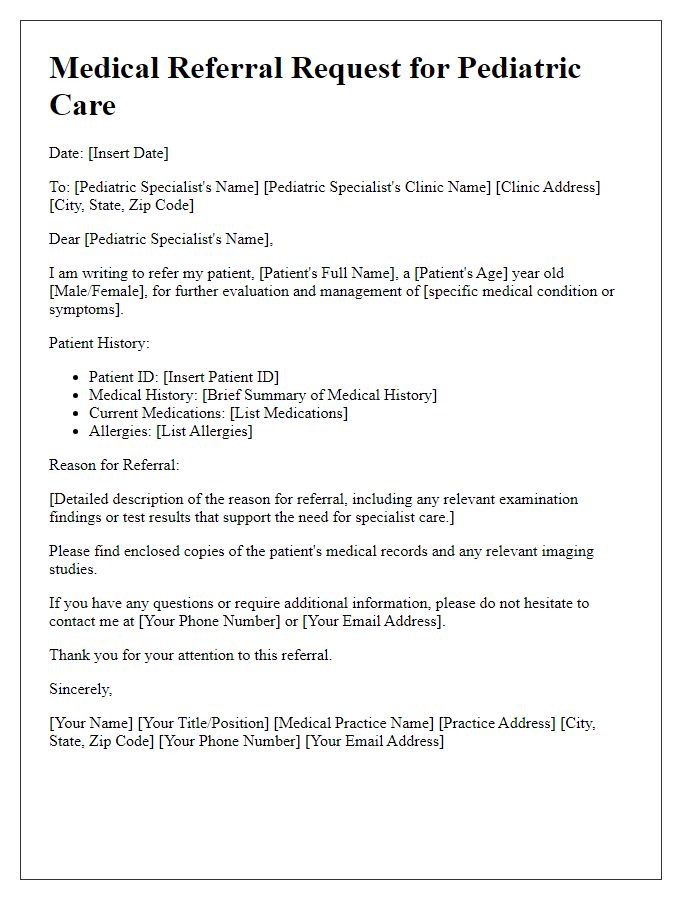
Patient information is critical for accurate medical referrals in healthcare settings. Essential details include the patient's full name, date of birth (DOB), and contact information. Medical history encompasses current diagnoses and previous treatments, including surgeries, allergies, and prescriptions. Insurance information, such as the provider and policy number, ensures coverage for consultations. Referring physician data, including specialty, practice location, and contact details, facilitates smooth communication between healthcare providers. Specific reasons for referral must be articulated, detailing symptoms, duration, and any relevant exam findings. These elements create a comprehensive picture of the patient's health, aiding specialists in effective evaluation and treatment.
Referring Physician Details
A medical referral request requires the inclusion of specific details to ensure clarity and facilitate communication between healthcare providers. The referring physician's name, such as Dr. John Smith, should be stated prominently. Contact information, including the office phone number (555-123-4567), fax number (555-987-6543), and email address (john.smith@medicalgroup.com), is critical for prompt follow-up. The physician's specialty, such as Family Medicine or Internal Medicine, should be indicated for context. Additionally, including the medical institution's name, like Springfield General Hospital, along with its address (123 Health St, Springfield, IL 62701), contributes to establishing the referral's professional backdrop. This format ensures accuracy during the referral process while enabling smooth patient transitions between providers.
Medical History Summary
A medical history summary is a crucial document for understanding a patient's healthcare context. It should include key information such as the patient's demographics (name, age, gender), a comprehensive list of past medical conditions (like diabetes or hypertension), current medications (including dosages and frequencies), and recent surgeries or hospitalizations (with dates and reasons). Additionally, family medical history should be noted, highlighting hereditary conditions that may impact the patient's health. Allergy information, particularly to medications (like penicillin or aspirin), is essential for preventing adverse reactions. Lifestyle factors (such as smoking, alcohol consumption, and exercise habits) contribute valuable insights for ongoing care. Lastly, a summary of recent diagnostic tests (like blood work or imaging studies) enhances the understanding of the patient's current health status, aiding in effective referrals to specialized services if needed.
Reason for Referral
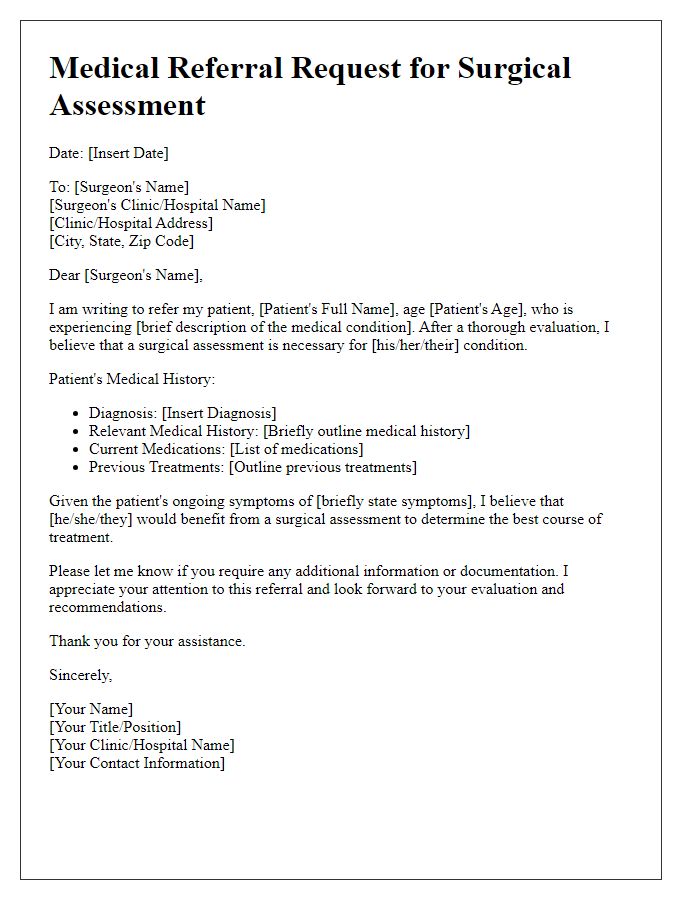
A medical referral request is often necessitated by complex patient needs requiring specialized intervention from healthcare professionals. Conditions such as chronic pain syndromes, cardiovascular diseases, or mental health disorders can warrant a referral for expert evaluation. Such requests typically outline specific reasons for seeking additional expertise, which may include diagnostic clarification, advanced treatment options, or surgical interventions. Clear documentation of the patient's medical history, current treatment protocols, and any previous diagnostic imaging or laboratory results can enhance the referral process. Referrals should be directed to specialists in relevant fields, such as orthopedic surgeons, cardiologists, or psychiatrists, to ensure optimal patient care and outcomes.
Specific Diagnostic or Treatment Requests
In a medical referral request, specifying diagnostic or treatment needs is essential for the proper management of patient care. A request for a specialized neurological evaluation, for instance, may arise from symptoms such as persistent migraines (lasting more than 15 days a month) or unexplained seizures. A referral to a gastroenterologist could be needed for a patient experiencing chronic abdominal pain (lasting over six months) accompanied by significant weight loss (over 10% of body weight), which may indicate underlying conditions like celiac disease or Crohn's disease. Timely access to diagnostic tests such as MRIs, CT scans, or endoscopies is crucial for accurate diagnosis and effective treatment pathways. Clear communication of patient history, along with specific diagnostic or therapeutic interventions required, ensures seamless transitions across healthcare settings.
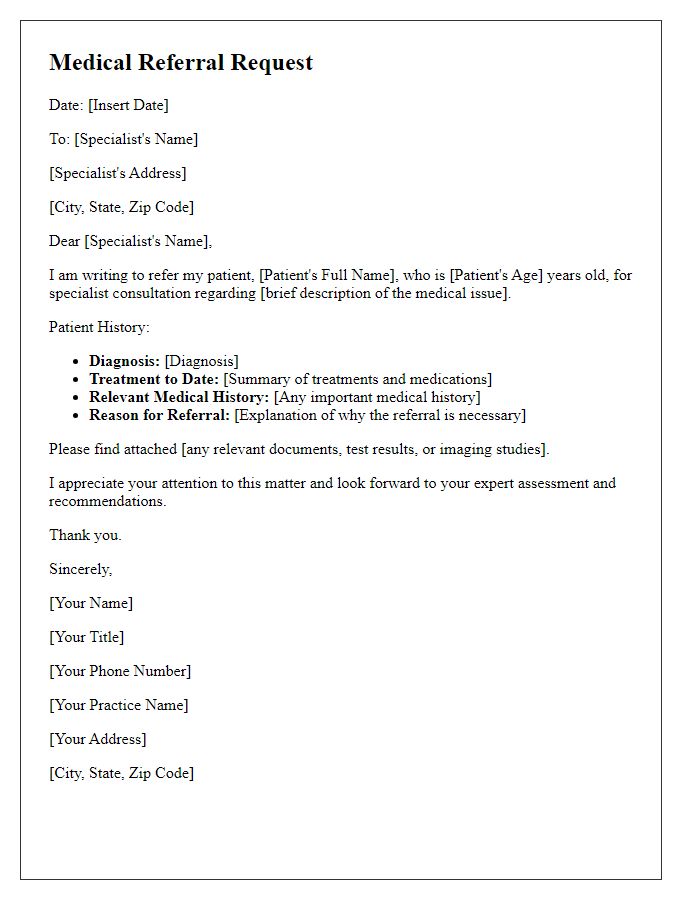
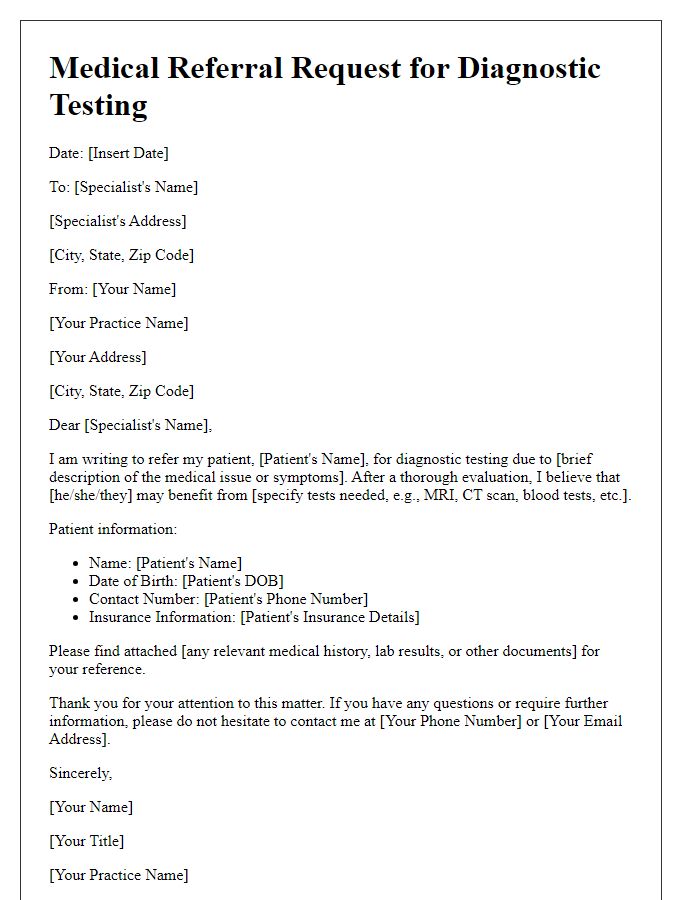
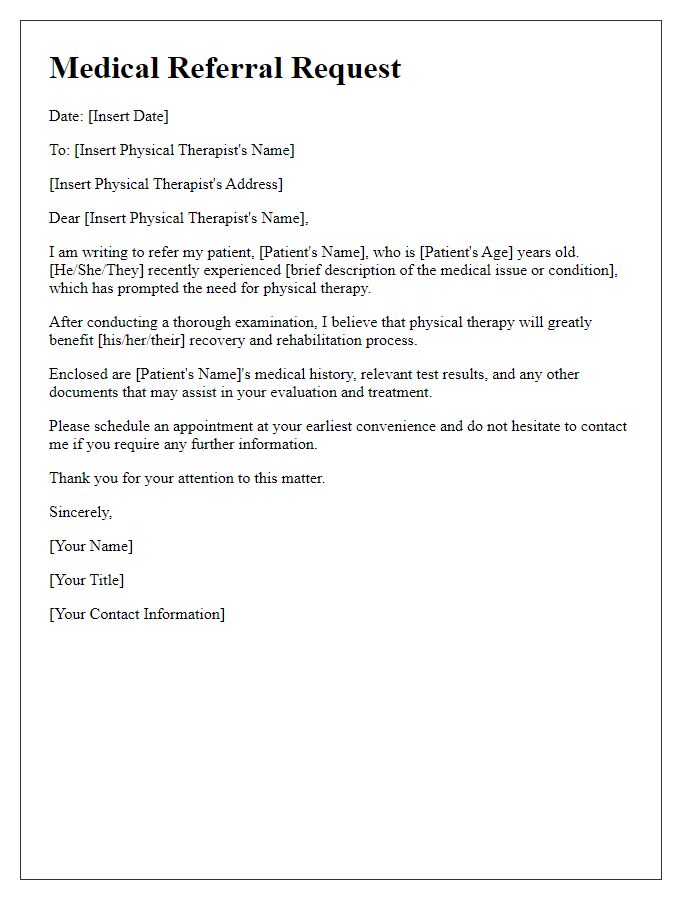
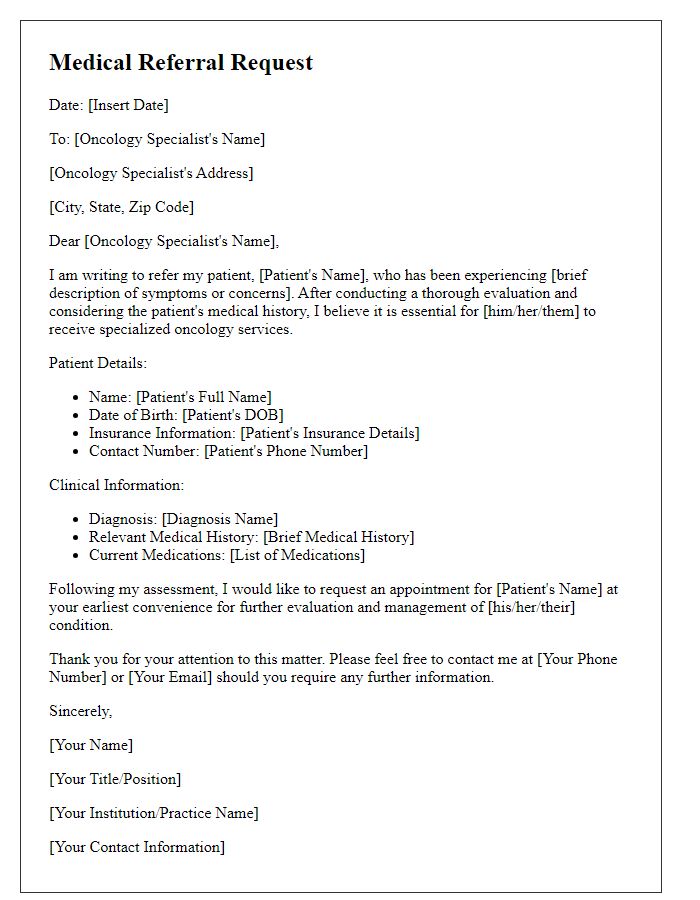
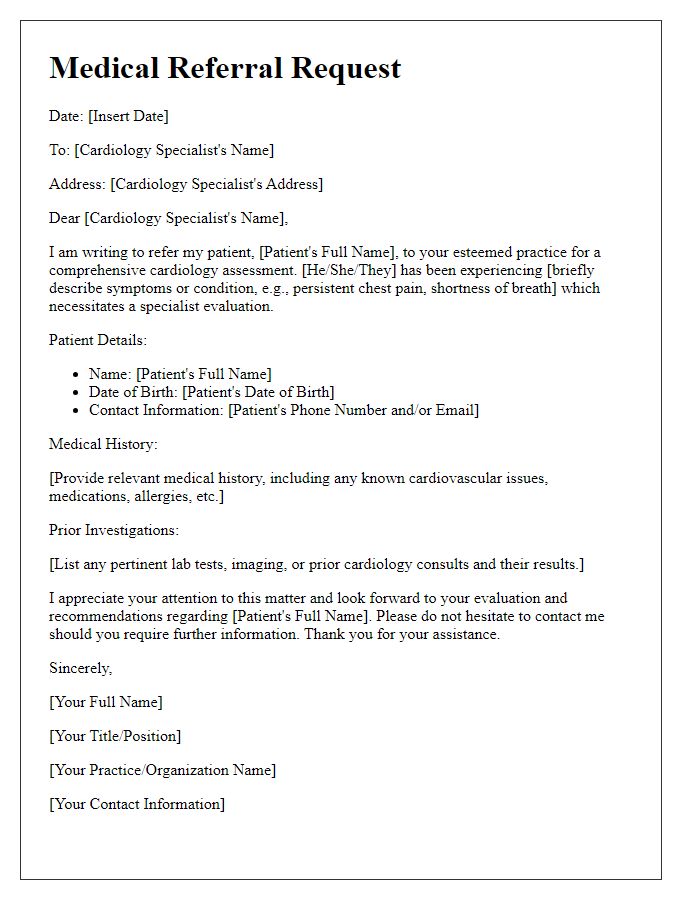
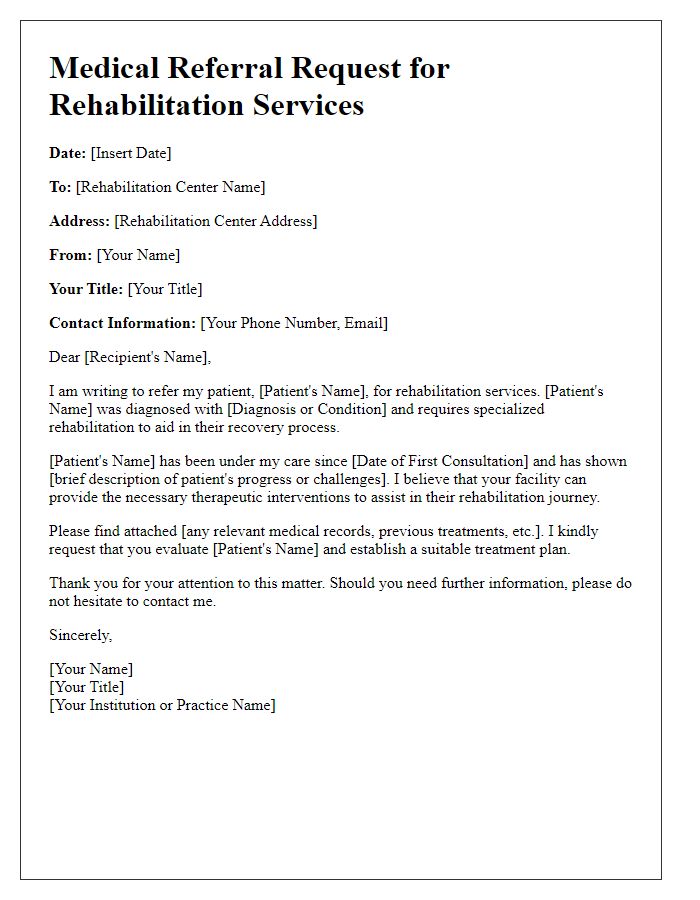
Letter Template For Medical Referral Request Samples
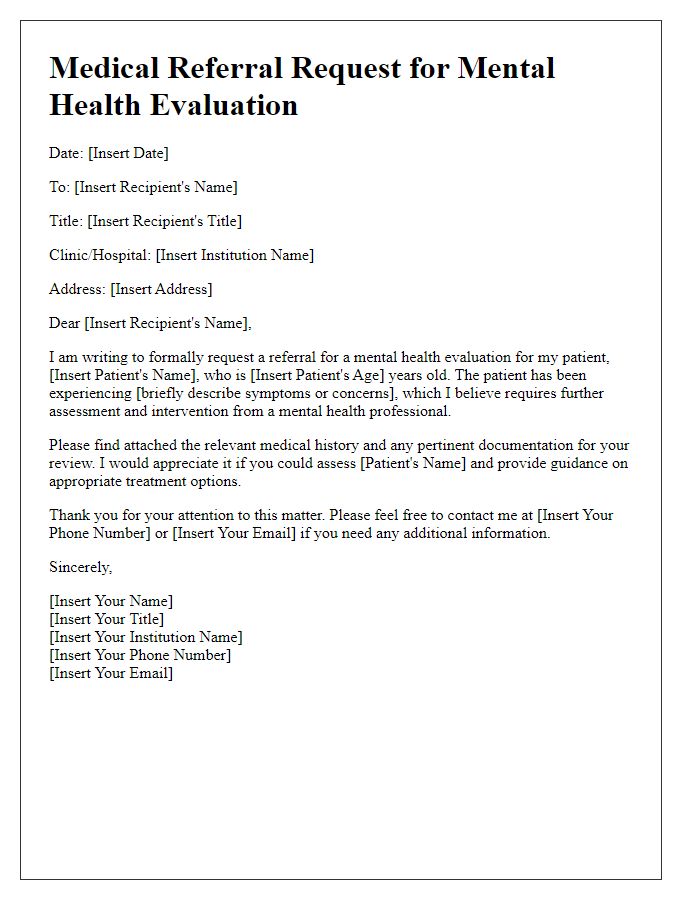
Letter template of medical referral request for mental health evaluation
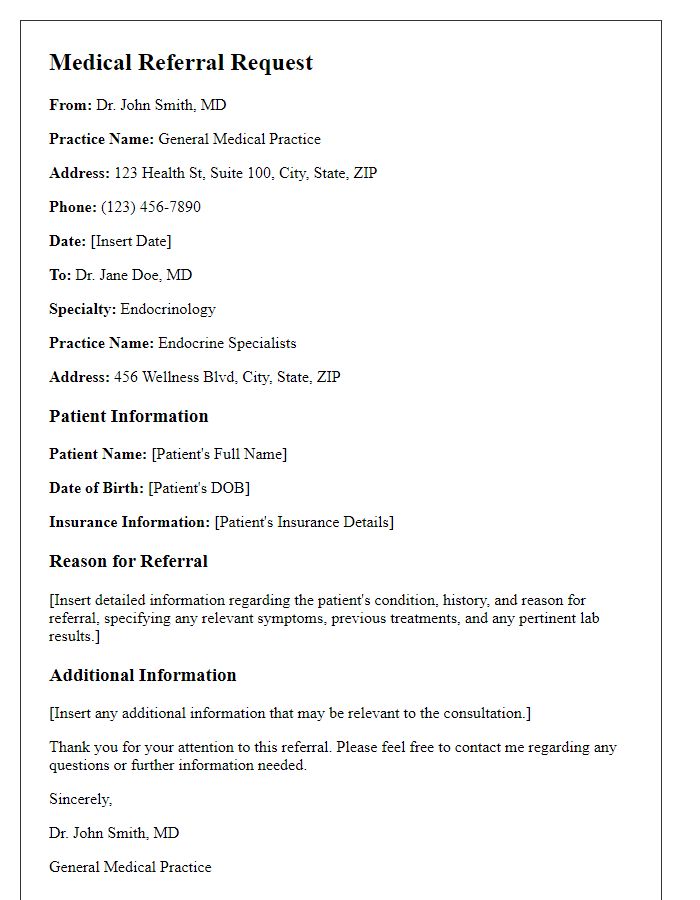
Letter template of medical referral request for endocrinology consultation


Comments