Following up after a neurological exam can feel both necessary and overwhelming. It's essential to understand the results and the next steps in your care, as this information can shape your health journey. In this article, we'll break down the key components of a follow-up letter, ensuring that you grasp the nuances of your neurological assessment with ease. Join us as we delve deeper into how to effectively communicate with your healthcare provider and what you can expect moving forward!
Patient Identification Information
Patient identification information plays a crucial role in the documentation and continuity of care for individuals undergoing neurological exams. This includes the patient's name, which should be comprehensive and clearly presented as last name followed by first name, ensuring accurate identification. Patient's date of birth (DOB), typically formatted as MM/DD/YYYY, aids in differentiating between individuals with similar or identical names. Additionally, the medical record number (MRN) assigned by the healthcare institution provides a unique identifier for easy retrieval of medical history. Contact information should encompass the patient's phone number and current address, allowing for smooth communication regarding follow-up appointments or additional testing. Insurance details may also be necessary, including the provider's name and policy number, facilitating billing and authorization for neurological services. Charting these elements ensures a systematic approach to patient management within neurological care settings.
Exam Summary and Findings
The neurological exam follow-up report outlines critical observations regarding cognitive function, reflexes, and motor skills. Key findings include the assessment of cranial nerves, which revealed normal function in vision and hearing, alongside intact gag and facial movements. Reflex testing indicated hyperreflexia in the upper extremities, while lower extremity reflexes remained within normal limits. Gait analysis demonstrated no significant abnormalities, although coordination tasks, such as finger-to-nose tests, showed slight dysmetria. Sensory evaluation highlighted diminished sensation in the left arm, potentially indicating underlying neuropathy. Overall, the detailed examination provides vital insights into the patient's neurological health and potential areas needing further investigation or intervention.
Diagnosis and Interpretation
A neurological exam follow-up, focusing on the diagnosis and interpretation, often emphasizes key aspects such as brain function, sensory abilities, and reflex responses. Common diagnoses include Alzheimer's disease, a progressive neurodegenerative condition affecting memory and cognitive abilities, and Multiple Sclerosis (MS), an autoimmune disorder impacting communication between the brain and body. Evaluation typically involves brain imaging techniques like MRI (Magnetic Resonance Imaging) to identify lesions or abnormalities in the CNS (Central Nervous System). Additionally, patient symptoms such as headaches, coordination issues, or visual disturbances provide crucial context for interpretation. In summary, this follow-up aims to clarify the diagnosis, assess the impact on daily functioning, and guide further management strategies for optimal patient care.
Recommended Treatment Plan
A neurological follow-up appointment provides essential insights regarding conditions such as migraines, Parkinson's disease, or multiple sclerosis. During the assessment, a physician may evaluate vital signs like blood pressure, heart rate, and neurological indicators, including reflexes and sensory perception. For patients experiencing chronic migraines, a treatment plan might include medications such as triptans or beta-blockers, which have been shown to alleviate symptoms. Lifestyle modifications, including regular exercise and hydration, play critical roles in managing conditions. For progressive disorders like Parkinson's disease, therapies may include dopamine agonists or deep brain stimulation, aimed at improving motor function and quality of life. Regular monitoring of symptoms and adjusting treatment accordingly is crucial for patient outcomes. Collaboration with physiotherapists or occupational therapists may enhance rehabilitation efforts, focusing on improving mobility and daily living skills.
Follow-up Appointments and Instructions
Follow-up appointments for neurological exams are critical for assessing patient progress and treatment effectiveness. Typically scheduled within a few weeks following initial evaluations, these appointments allow healthcare providers to review neurological function changes, medication effects, and any emerging symptoms. Instructions often include maintaining a symptom diary, noting any fluctuations in headaches, seizures, or neurological deficits, and adhering to prescribed treatment plans, which may involve medications like antiepileptics or lifestyle adjustments. Patients may also be advised to undergo additional diagnostic tests, such as MRI scans or EEGs, at specific intervals to monitor brain activity and assess for conditions like multiple sclerosis or epilepsy. Regular follow-up is essential for optimizing patient care and ensuring early intervention if complications arise.
Letter Template For Neurological Exam Follow-Up Samples
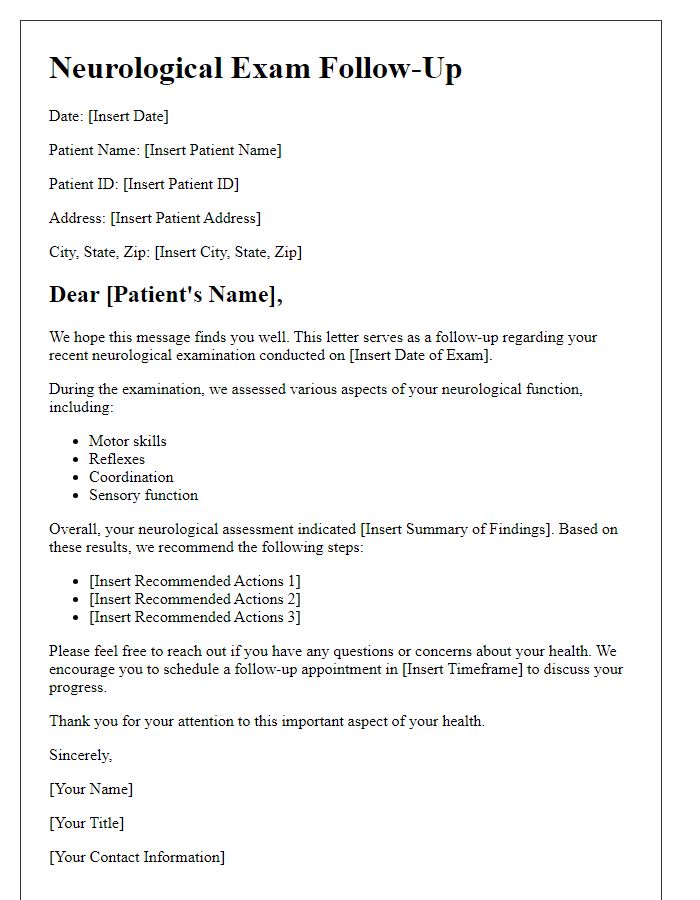
Letter template of neurological exam follow-up for general health assessment.
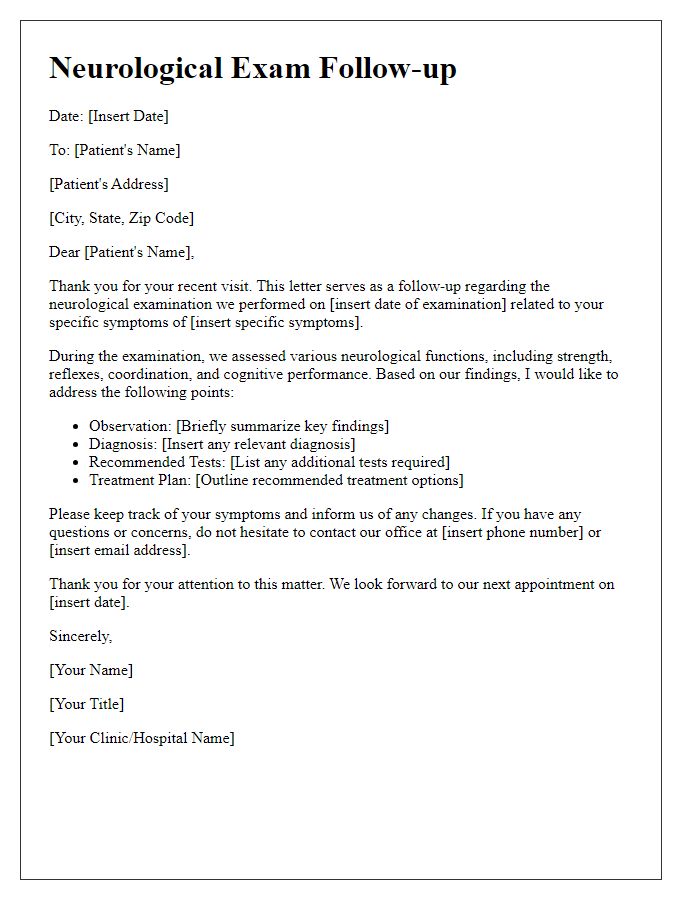
Letter template of neurological exam follow-up for specific symptom evaluation.
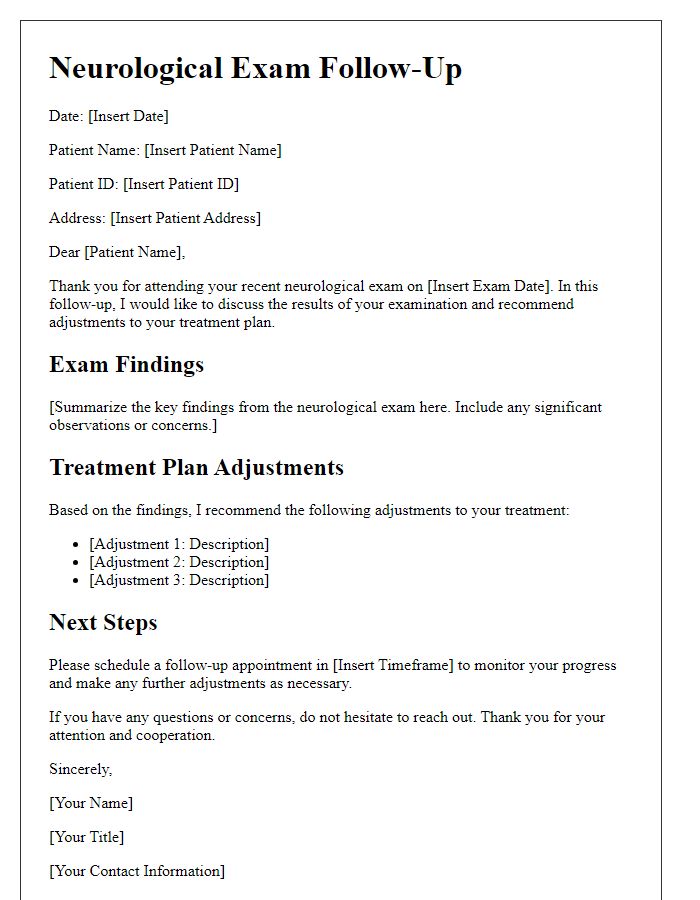
Letter template of neurological exam follow-up for treatment adjustment.
Letter template of neurological exam follow-up for referral to a specialist.
Letter template of neurological exam follow-up for lifestyle and management recommendations.
Letter template of neurological exam follow-up for patient progress monitoring.
Letter template of neurological exam follow-up for chronic condition management.


Comments