Navigating the world of healthcare can often feel overwhelming, especially when it comes to obtaining necessary treatments. One crucial aspect of this journey is understanding prior authorization requests, which can determine whether a specific procedure or medication is covered by insurance. By familiarizing yourself with the ins and outs of these requests, you can empower yourself to advocate for your healthcare needs. Ready to dive deeper into the process and learn how to effectively craft your own prior authorization request?
Patient Information and Diagnosis
Patient information is critical for a prior authorization request, including the patient's full name, date of birth (DOB), insurance policy number, and diagnosis details. Diagnosis details should specify the medical condition (such as Hypertension, coded as I10 in ICD-10), the onset date, and any pertinent medical history, including previous treatments or medications tried (like Lisinopril or Amlodipine) and their outcomes. Accurate and concise documentation ensures that the insurance company can quickly assess the necessity of the requested treatment or medication, facilitating timely patient care. Comprehensive details can mitigate delays, ensuring compliance with healthcare regulations and standards set by entities such as the Centers for Medicare & Medicaid Services (CMS).
Detailed Treatment Plan and Medical Necessity
A prior authorization request detailing the treatment plan and medical necessity for a patient diagnosed with chronic migraines, for instance, may include specific procedures such as Botox injections (onabotulinumtoxinA) administered every 12 weeks, along with prescription medications like topiramate and amitriptyline. A physician's office located in New York City (Manhattan) may emphasize the patient's history of migraines occurring 15 or more days per month despite using over-the-counter pain relief. The plan must also reflect recent diagnostic imaging results from a MRI scan to rule out secondary causes, ensuring compliance with clinical guidelines that support the use of preventive treatments for high-frequency migraine sufferers. Details about prior treatment failures, such as inadequate responses to triptans and NSAIDs, bolster the argument for medical necessity, highlighting the need for a comprehensive approach to managing the debilitating symptoms affecting the patient's quality of life.
Relevant Clinical Evidence and Guidelines
Prior authorization requests for medical treatments often hinge on relevant clinical evidence and guidelines that support the necessity of the proposed intervention. Clinical trials, such as those published in the New England Journal of Medicine, often provide critical data on efficacy rates, side effects, and comparative effectiveness of treatments. The National Comprehensive Cancer Network (NCCN) guidelines, for example, offer evidence-based recommendations for managing specific cancers, ensuring that treatments align with best practices. Additionally, studies from institutions like the American Medical Association highlight the importance of individualized patient care, emphasizing data on patient outcomes based on demographic factors. Understanding the nuances of these sources strengthens the justification for approval, ensuring compliance with regulatory standards and focusing on patient-centered care.
Specific Medication/Procedure Requested
Prior authorization requests for specific medications, such as Ocrelizumab for multiple sclerosis, require detailed documentation. Healthcare providers must include patient identification numbers, documented medical history, and a description of the condition (e.g., relapsing forms of multiple sclerosis) that necessitates treatment. The request should clearly outline the medication's indication per the latest clinical guidelines and previous treatment attempts, along with their outcomes. Such details provide the insurance company with a comprehensive understanding of the need for the medication and may reference relevant medical literature or studies that support the use of Ocrelizumab in managing symptoms and improving patient outcomes. Prompt submission of this information can expedite the approval process.
Healthcare Provider Contact Information
Healthcare providers play a crucial role in ensuring patients receive necessary medical services by submitting prior authorization requests. These requests often include crucial details such as the healthcare provider's name, which may be Dr. Emily Smith, a specialist in cardiology, and the contact number, for instance, (555) 123-4567. The provider's facility may be Heart Health Clinic located in Boston, Massachusetts. Additionally, the National Provider Identifier (NPI) number, such as 1234567890, is key for identification in health insurance systems. Accurate and complete contact information expedites the authorization process, ensuring timely access to necessary treatments.
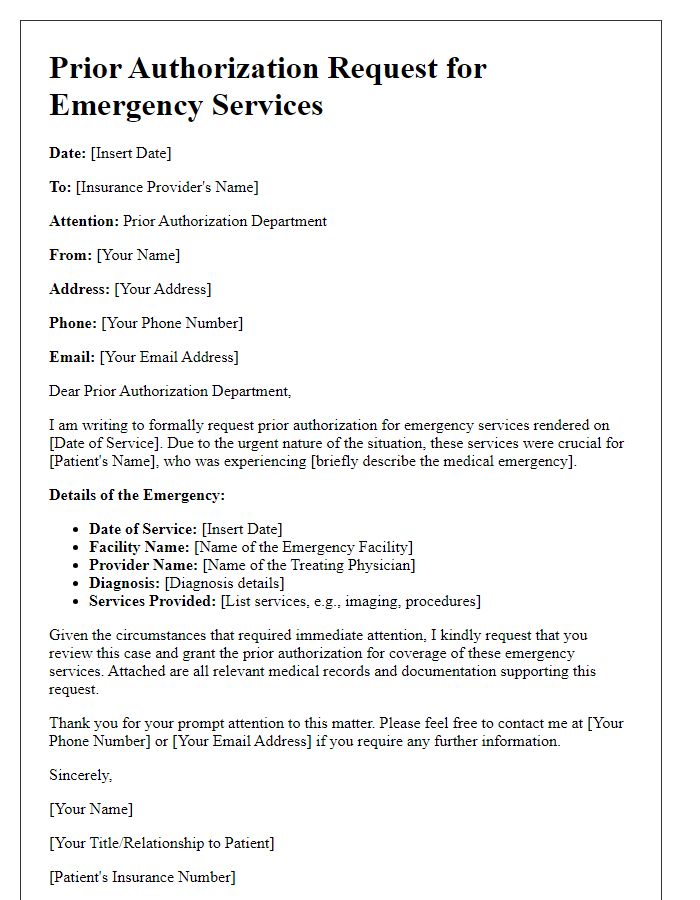
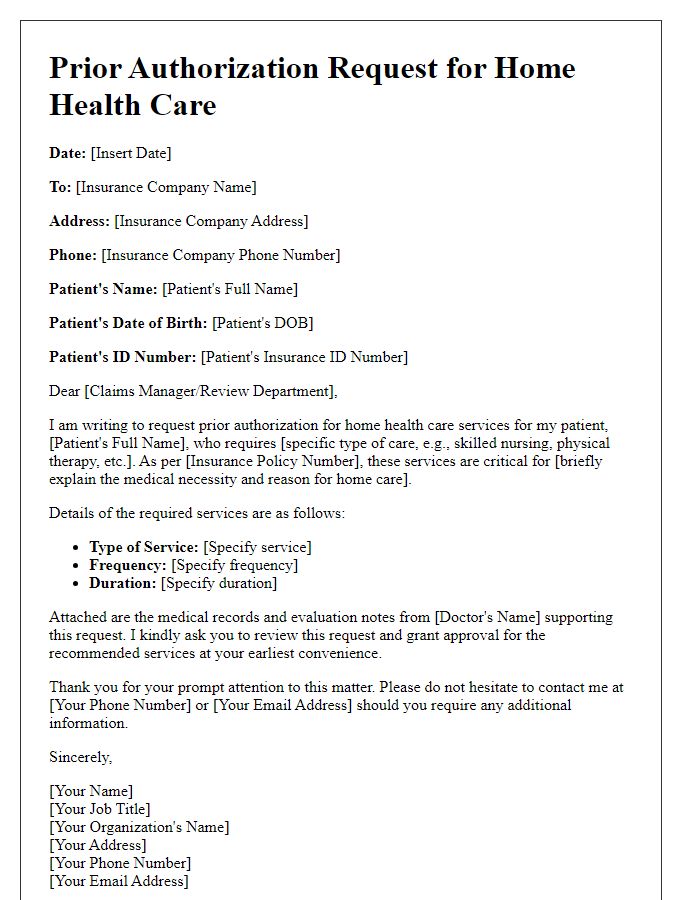
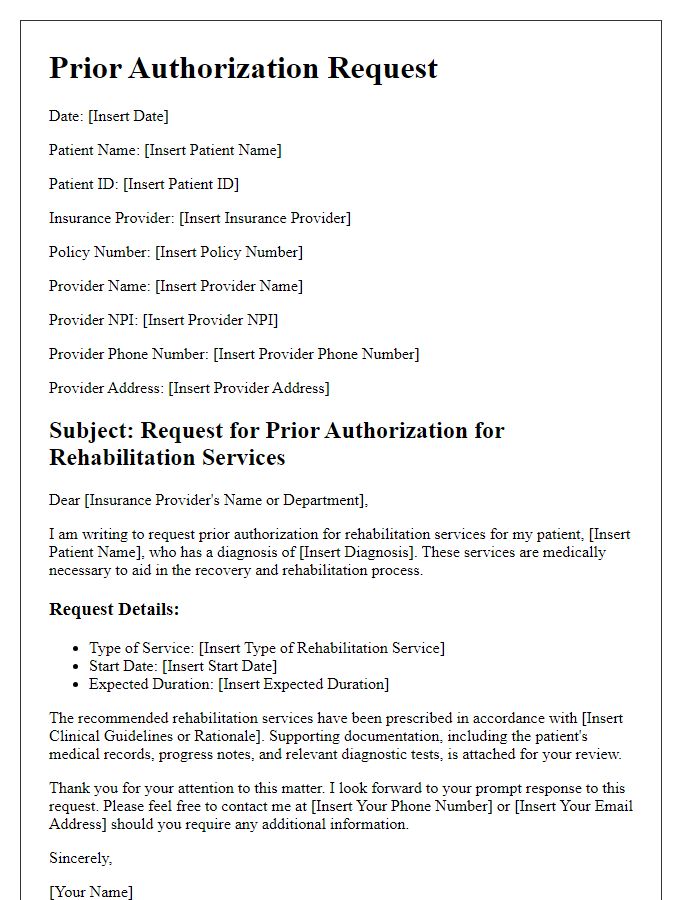
Letter Template For Prior Authorization Request Samples
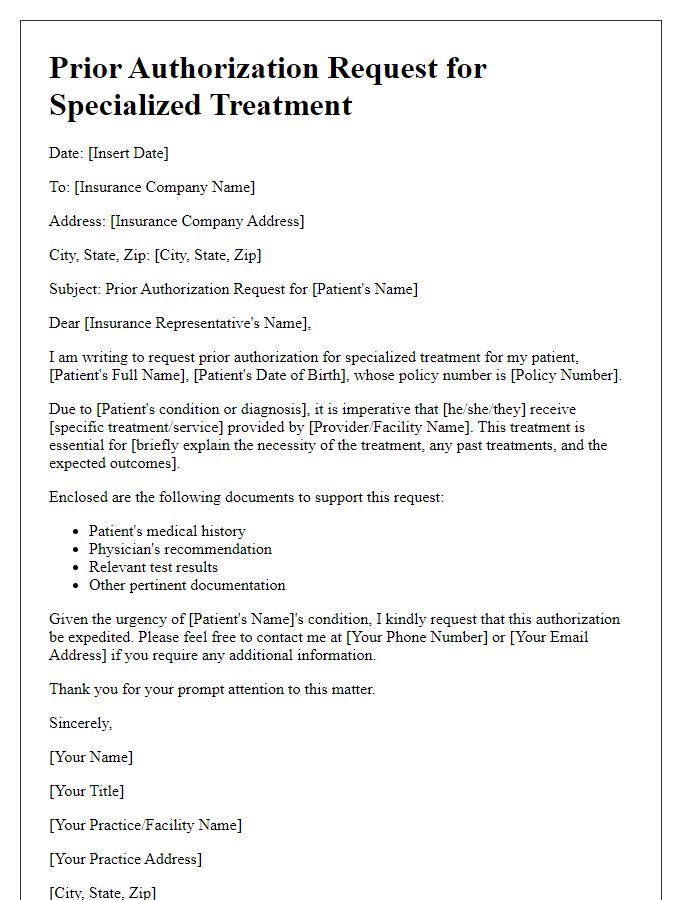
Letter template of prior authorization request for specialized treatment
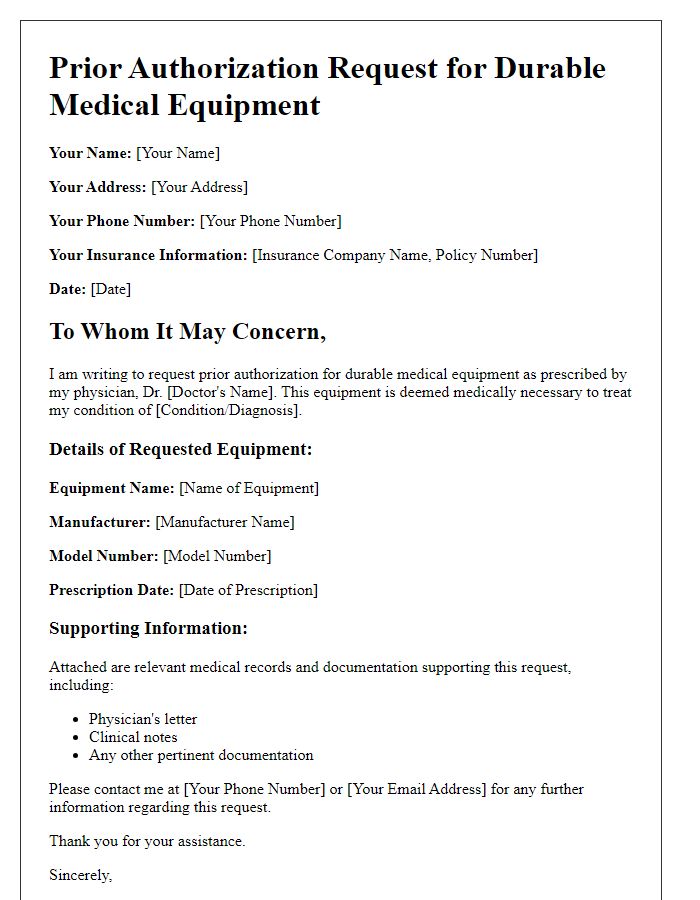
Letter template of prior authorization request for durable medical equipment
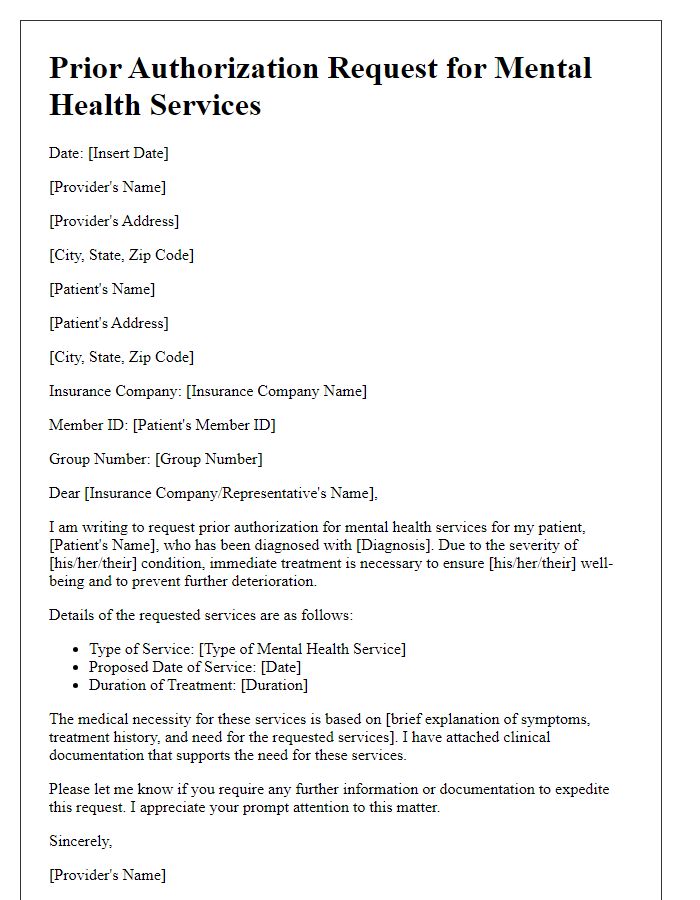
Letter template of prior authorization request for mental health services
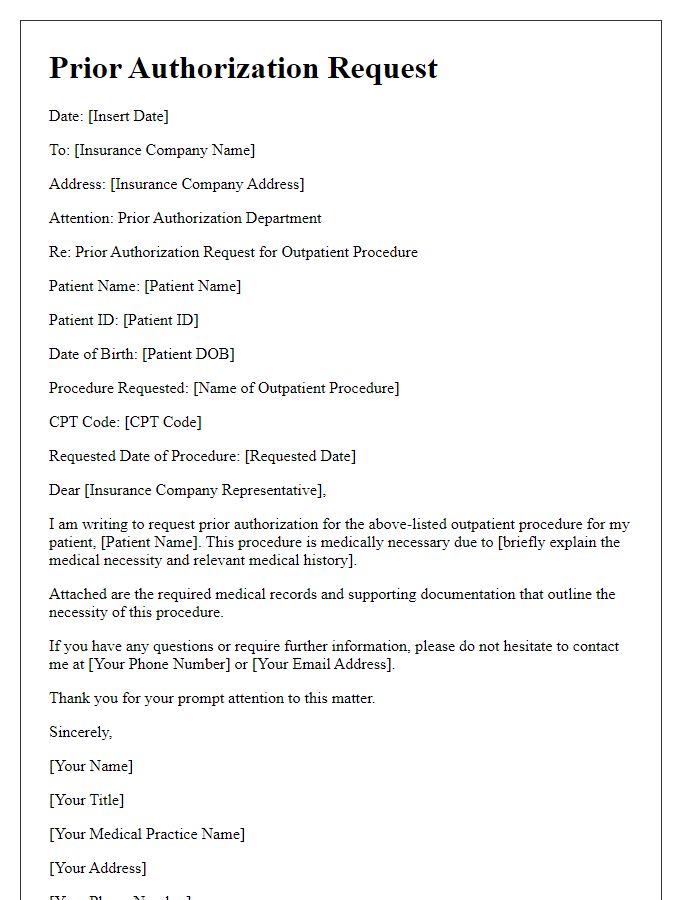
Letter template of prior authorization request for outpatient procedures


Comments