Are you considering a corneal transplant or just curious about the evaluation process? Understanding what to expect can make a significant difference in your journey towards better vision. This article will walk you through the essential steps of a corneal transplant evaluation, providing clarity and insight into this life-changing procedure. Let's dive in and explore the process together!
Patient's Full Name and Contact Information
Corneal transplantation aims to restore vision by replacing damaged corneal tissue with a healthy donor cornea. Pre-operative evaluations are crucial, assessing patient factors such as the underlying condition leading to corneal opacity, like keratoconus or trauma. Comprehensive eye examinations, including refraction measurements, corneal topography, and pachymetry, provide essential insights into corneal thickness and shape. Patient's full name and contact information must be accurately documented to facilitate surgical coordination and ensure effective communication throughout the process. Evaluation also involves discussing medical history to identify any contraindications. A detailed consent process informs patients about potential risks, benefits, and the expected recovery timeline post-transplantation.
Physician's Contact Details
The corneal transplant evaluation process involves multiple critical assessments and consultations, typically conducted within specialized ophthalmology clinics. Key components include obtaining a comprehensive medical history, conducting visual acuity tests, and performing corneal topography, which maps the curvature of the cornea. Additional diagnostic imaging such as optical coherence tomography (OCT) provides detailed cross-sectional images of the cornea, essential for evaluating conditions such as keratoconus or corneal dystrophies. A thorough examination by a cornea specialist, ideally an ophthalmologist with fellowship training in corneal diseases, ensures accurate diagnosis. The physician's contact details, including clinic address and direct phone line, facilitate efficient communication between patients and healthcare providers throughout the evaluation process. This coordinated effort is crucial for determining patient eligibility for procedures like penetrating keratoplasty (full-thickness corneal transplant) or lamellar keratoplasty (partial-thickness corneal transplant).
Purpose of the Evaluation
Corneal transplant evaluations are essential procedures conducted to assess the health and suitability of a patient's cornea, the transparent front part of the eye. These evaluations determine the need for a corneal transplant, which involves replacing a diseased or damaged cornea with healthy tissue from a donor, usually within a specialized ophthalmic clinic. During the evaluation at facilities like the Cleveland Clinic, various tests, including corneal topography and slit-lamp examination, provide insights into the condition of the cornea. Appropriate candidates typically exhibit significant visual impairment or severe corneal scarring due to conditions such as keratoconus or corneal dystrophies. In addition, eye doctors will also check for underlying systemic diseases, such as diabetes or autoimmune disorders, that could affect recovery post-surgery. This comprehensive assessment outlines the potential risks and benefits of surgery to determine optimal patient outcomes.
Pre-Appointment Instructions
Before a corneal transplant evaluation at a specialized ophthalmology clinic, patients must follow important pre-appointment instructions for a successful assessment. First, schedule an appointment at least two weeks in advance to ensure availability of the necessary medical staff. Gather previous medical records and ophthalmic examination data to provide the healthcare team with a comprehensive overview of the patient's eye health history. Avoid wearing contact lenses for a minimum period of 72 hours prior to the visit, as this can affect corneal measurements and overall assessment accuracy. Prepare a list of questions regarding the corneal transplant procedure, including donor matching, recovery timeline, and potential risks associated with the surgery. Lastly, arrange for transportation after the appointment, as dilating eye drops may be administered, temporarily impairing vision.
Scheduling Details and Timeframe
Corneal transplant evaluations occur in specialized ophthalmology clinics where patients undergo comprehensive assessments. These evaluations typically involve scheduling an appointment within a timeframe of two to four weeks, depending on the clinic's availability. During the evaluation, important diagnostic tests, such as corneal topography and pachymetry, assess the health of the cornea (the transparent front part of the eye). Patients may also require imaging techniques, like optical coherence tomography (OCT), to carefully examine detailed eye anatomy. Following the evaluation, patients receive a detailed report highlighting their eligibility for transplant procedures, surgical options and potential waiting times, which can vary significantly based on factors such as donor availability in the local eye banks and the urgency of the patient's condition.
Letter Template For Corneal Transplant Evaluation Setup Samples
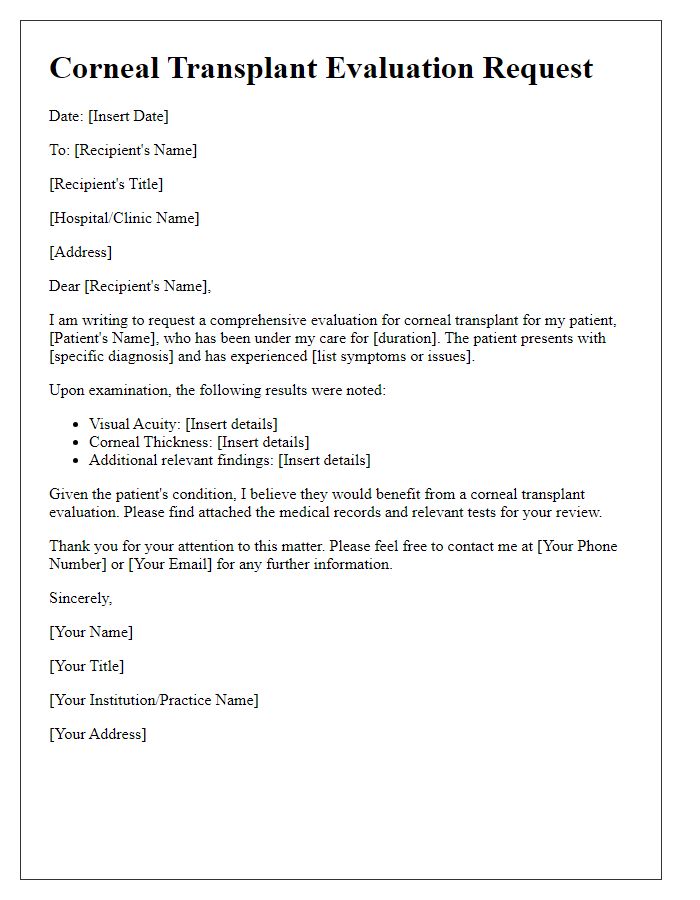
Letter template of corneal transplant evaluation request for ophthalmologist
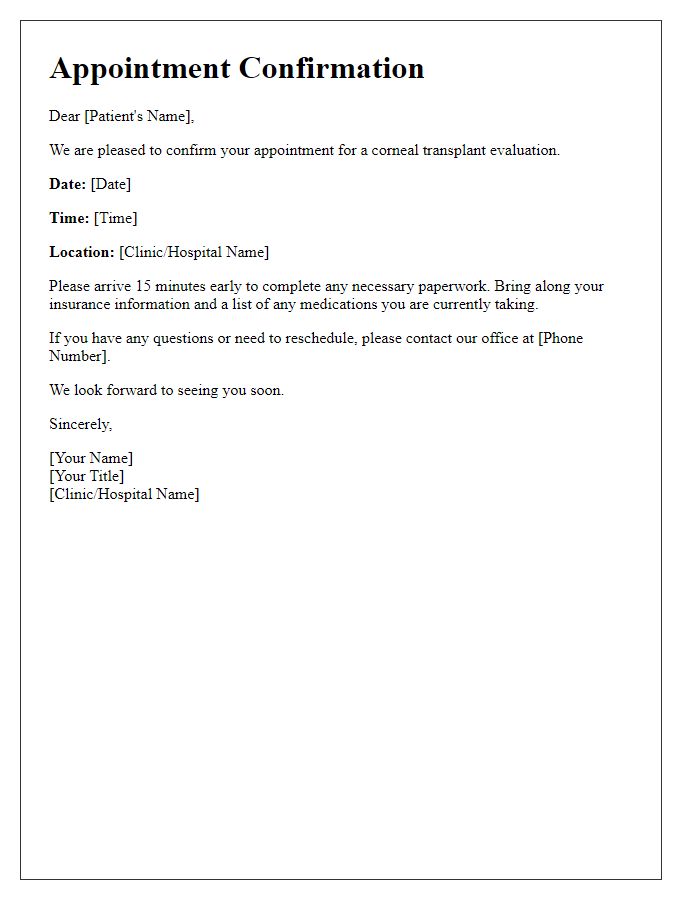
Letter template of corneal transplant evaluation appointment confirmation
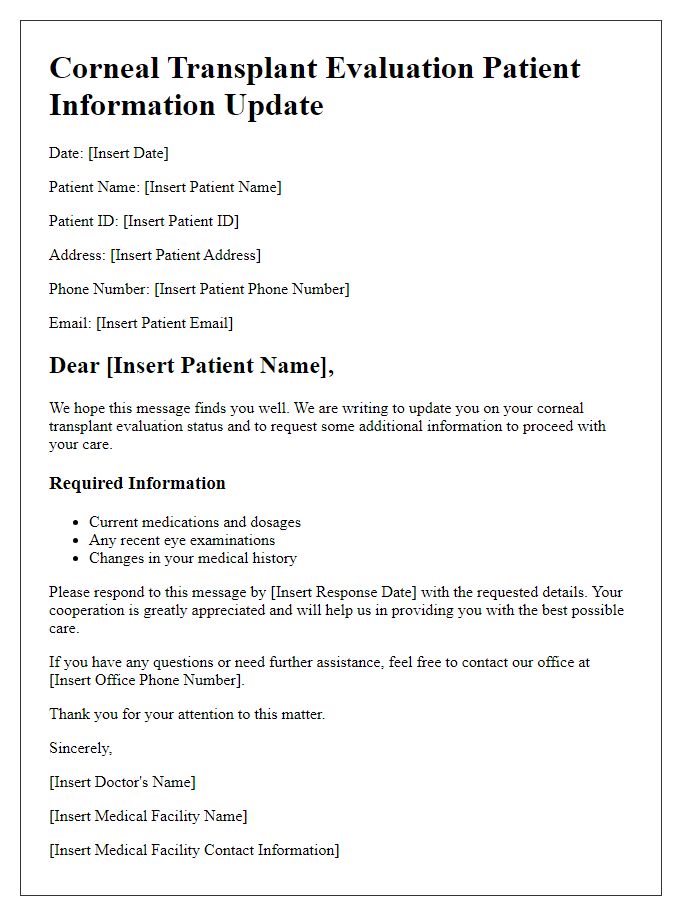
Letter template of corneal transplant evaluation patient information update
Letter template of corneal transplant evaluation for insurance authorization
Letter template of corneal transplant evaluation procedural instructions


Comments