Are you navigating the often-complex world of medical billing? It can be confusing, especially when it comes to understanding your statements and insurance coverages. In this article, we'll break down some common billing issues and provide tips on how to get the clarifications you need. Join us as we explore more about demystifying medical billing and ensuring you're fully informed!
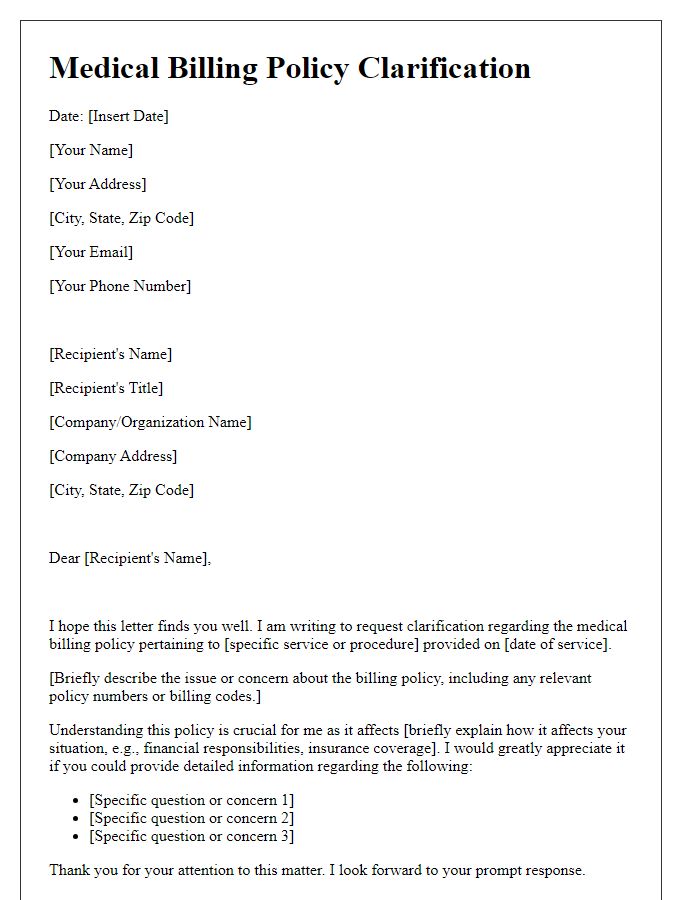
Patient Information
Medical billing clarification relies on precise details regarding patient information, including full name, date of birth, and insurance policy number. Accurate identification ensures correct processing of claims involving procedures, such as X-rays from August 2023 at Riverside General Hospital, and office visits coded for specific diagnoses like diabetes mellitus. Moreover, the inclusion of billing codes, known as CPT (Current Procedural Terminology), and associated dates of service provides clarity to avoid discrepancies. Addressing issues promptly enhances communication between healthcare providers, insurance companies, and patients, fostering financial transparency. Proper documentation and follow-up can greatly expedite claim resolution.
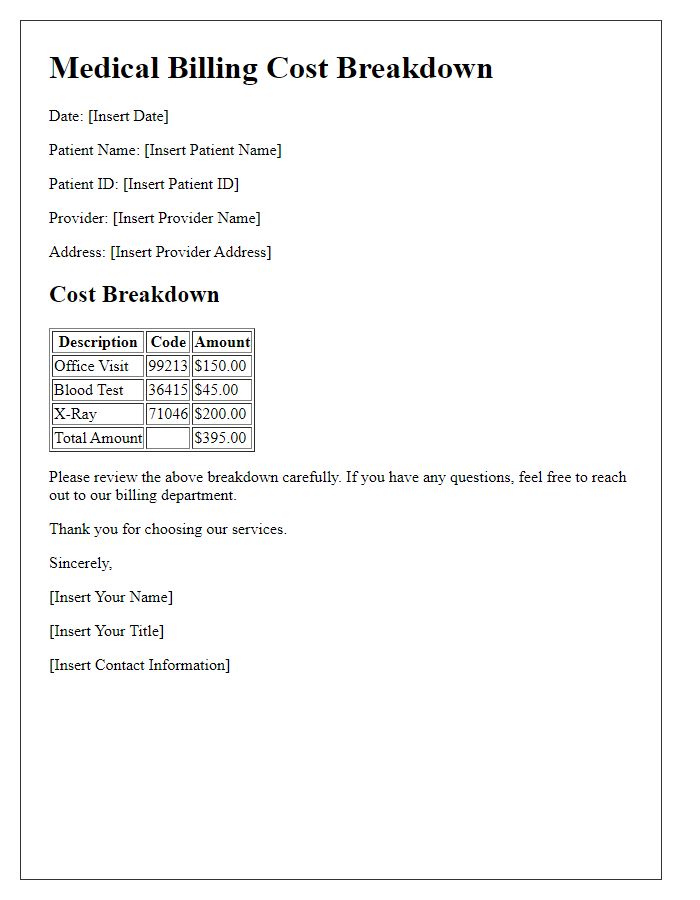
Billing Statement Reference
A billing statement reference serves as a crucial document in the medical billing process, providing detailed breakdowns of services rendered, payment statuses, and outstanding balances. The statement typically includes patient information such as demographics (name, address, insurance details), as well as provider specifics, including the healthcare facility's name and tax identification number. It lists dates of service, description of procedures (like consultations or surgeries), billed amounts, insurance adjustments, and patient responsibilities. Discrepancies or clarifications may arise due to coverage limits or coding errors, often prompting patients to reach out to billing departments for resolution. Ensuring clarity in these documents enhances transparency in medical transactions, ultimately improving patient-provider communication.
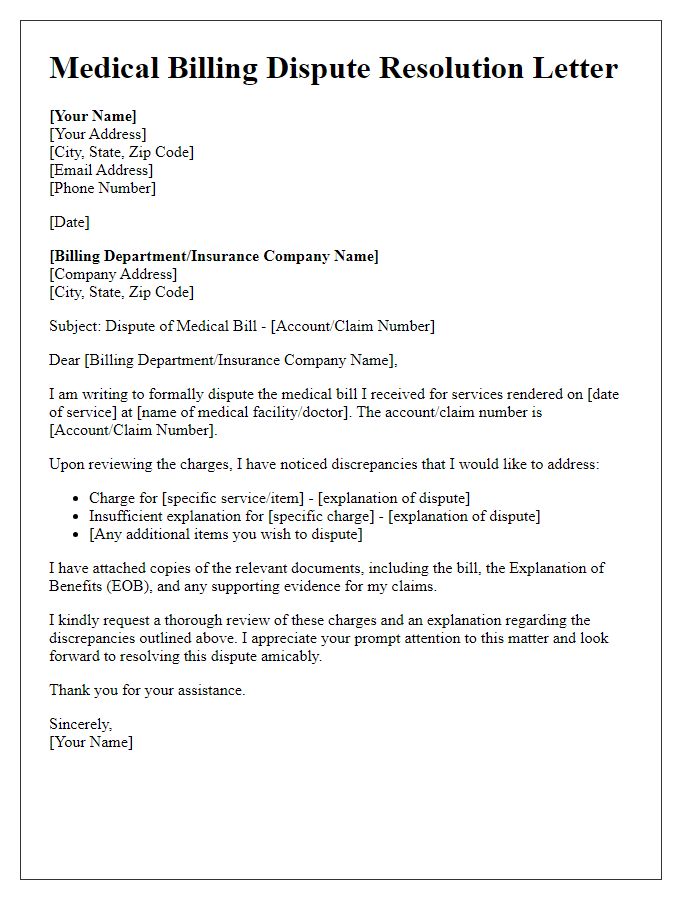
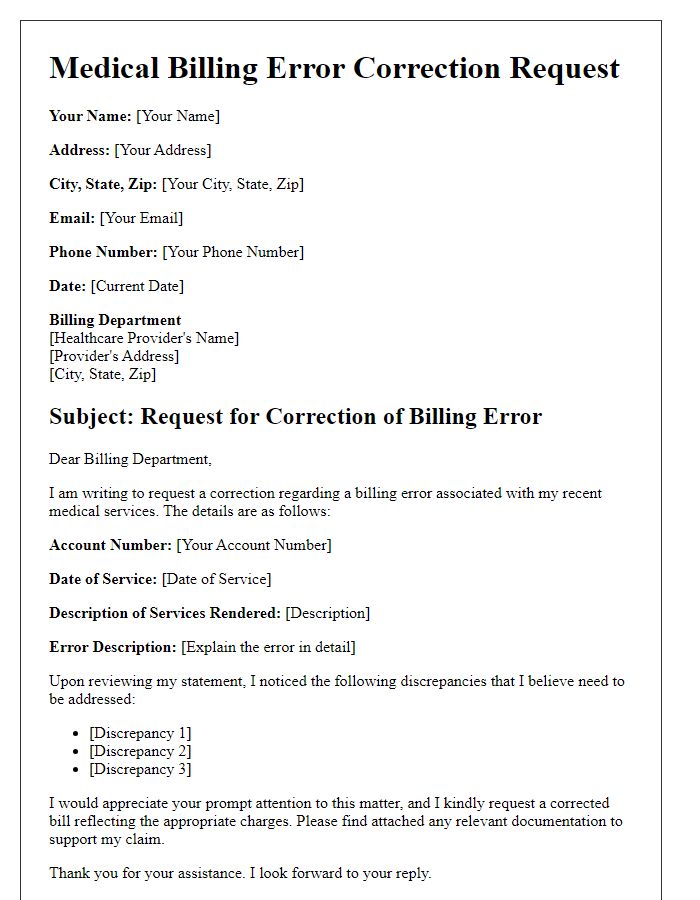
Detailed Description of Discrepancy
In medical billing, discrepancies often arise due to variations in charges for services rendered at healthcare facilities, such as hospitals or clinics, often involving coding issues with ICD-10 (International Classification of Diseases, 10th Revision) and CPT (Current Procedural Terminology) codes. For instance, a patient receiving physical therapy might see a difference in billed amounts, where the initial session costs $150, while subsequent sessions vary between $100 and $120, potentially due to insurance coverage policies or provider agreements. Additionally, itemized statements may show discrepancies in medication charges; a prescribed drug like Omeprazole, with a retail cost of $10, might show a billed amount of $15 due to markup by the provider. Billing errors can arise from outdated insurance information or clerical mistakes, leading to confusion over the responsibility for payment and requiring careful examination of Explanation of Benefits (EOB) documents to resolve claimed discrepancies effectively.
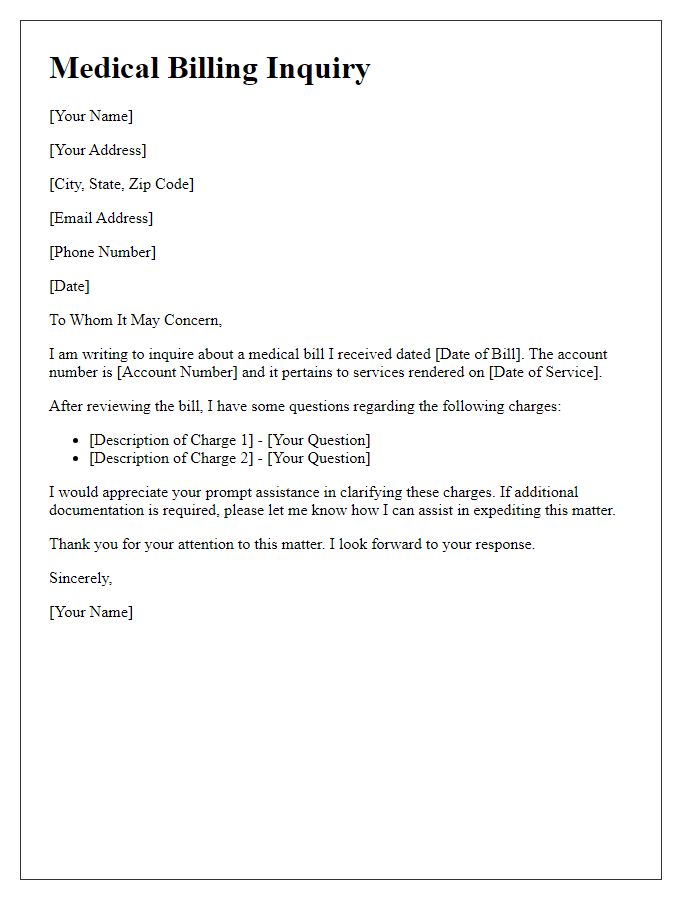
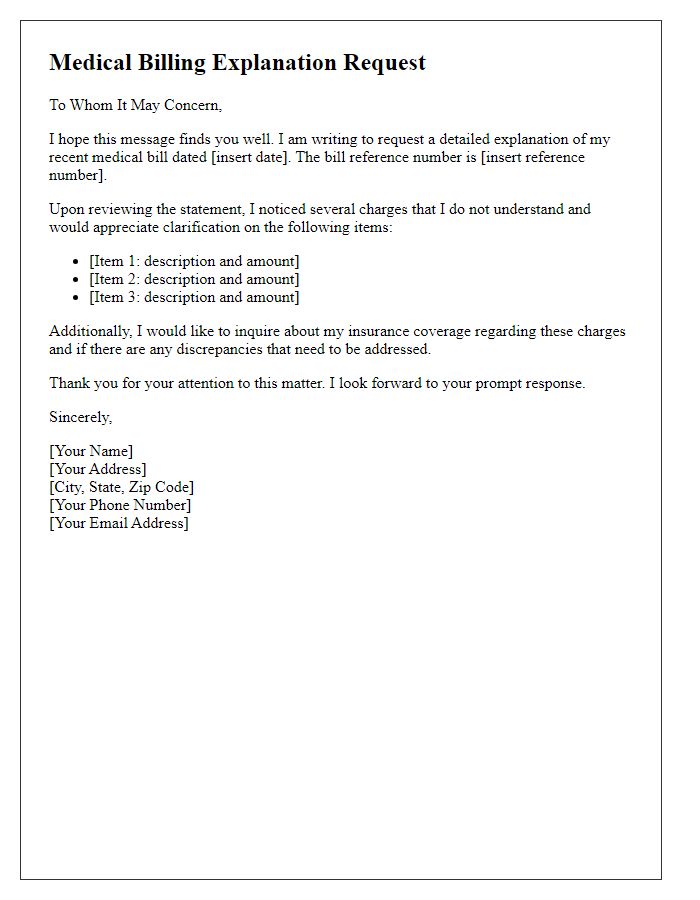
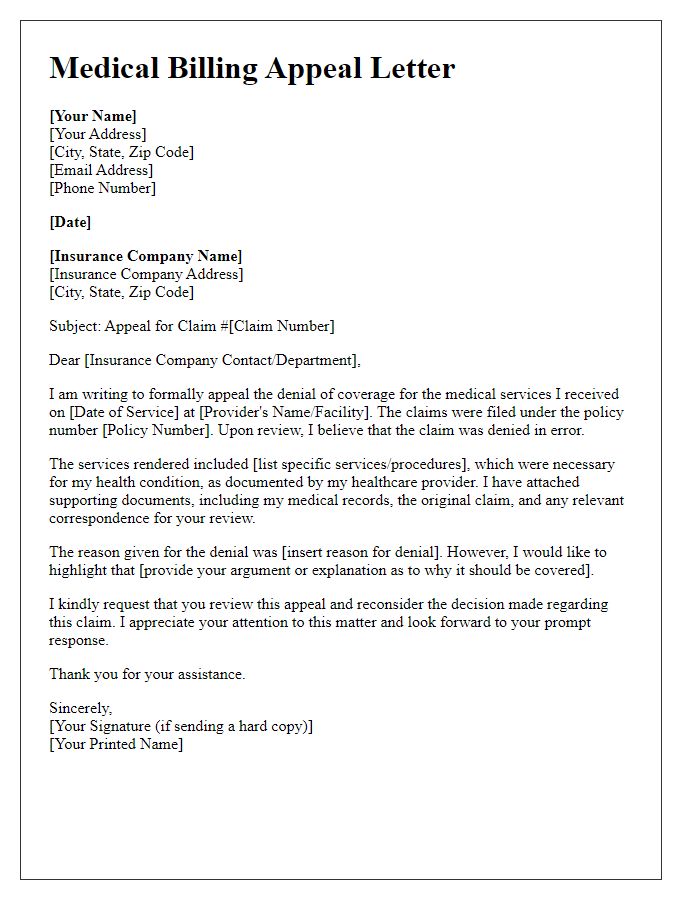
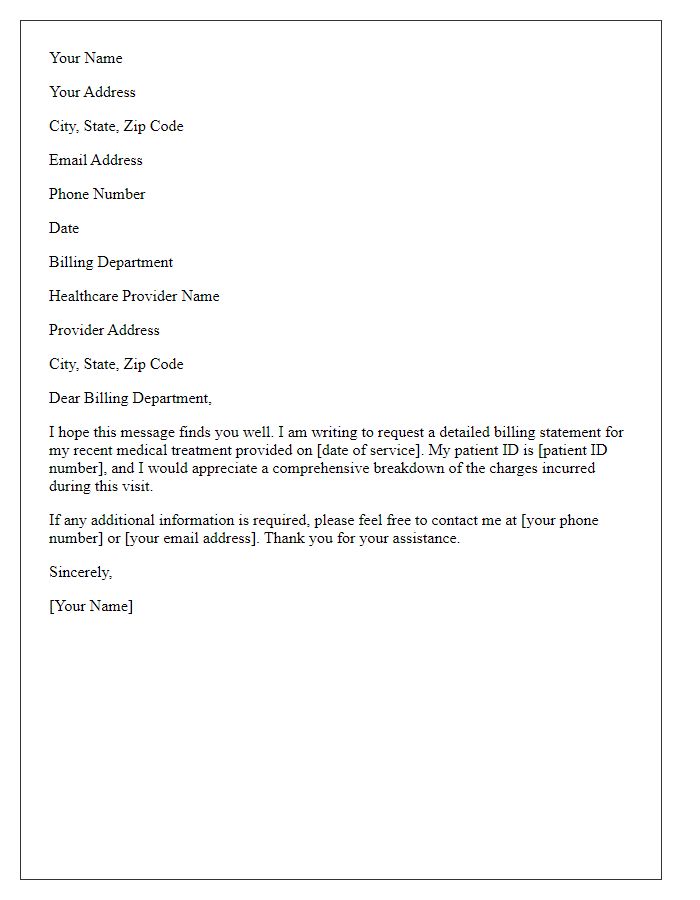
Request for Clarification
Medical billing processes often involve intricate details that require clear communication. A request for clarification typically addresses specific discrepancies in charges, service codes, or patient information. For instance, a patient may notice discrepancies in charges related to diagnostic tests (like MRI or CT scans) billed by a hospital or provider (such as XYZ Medical Center). The notice may cite claim numbers, dates of service, and amounts billed versus amounts paid. Clarifying questions might include inquiries about specific CPT codes (Current Procedural Terminology) used, copayment amounts, or insurance coverage limits pertaining to procedures. Ensuring comprehensive understanding can prevent potential billing errors and foster transparent relationships between patients, providers, and insurers.
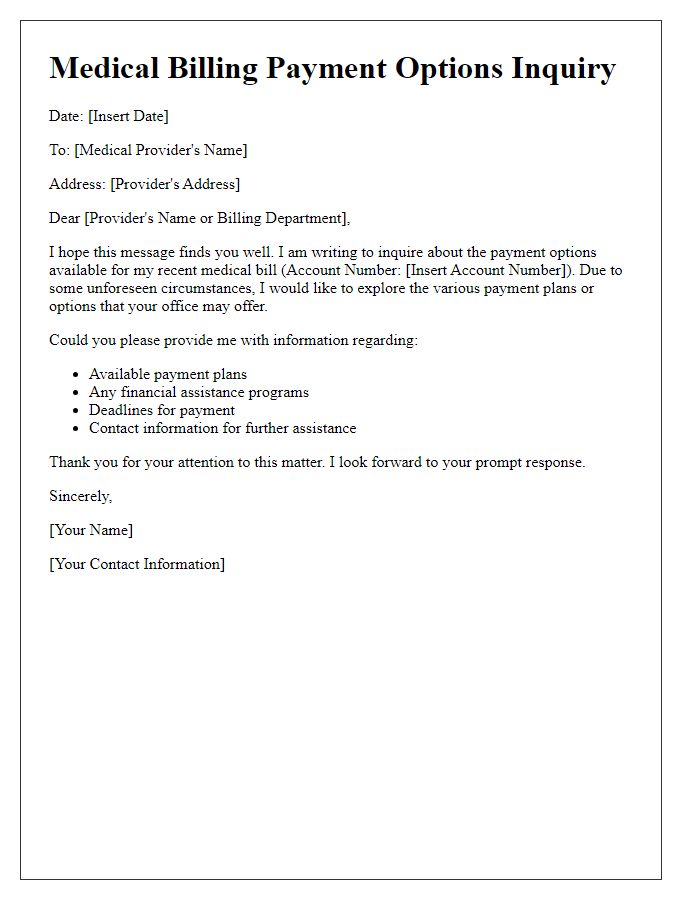
Contact Information and Preferred Response Method
Contact information accuracy is crucial in medical billing to ensure timely communication. Patients often provide phone numbers, email addresses, and mailing addresses for correspondence regarding billing issues or clarifications. Preferred response methods may include direct phone calls for immediate assistance, email for written documentation, or postal mail for formal correspondence. Clarifications regarding charges, insurance coverage, or payment plans can streamline the billing process and enhance patient satisfaction, reducing confusion and delays in payments. Keeping records up-to-date, including any changes in contact information, contributes to efficient billing management and effective resolution of discrepancies.



Comments