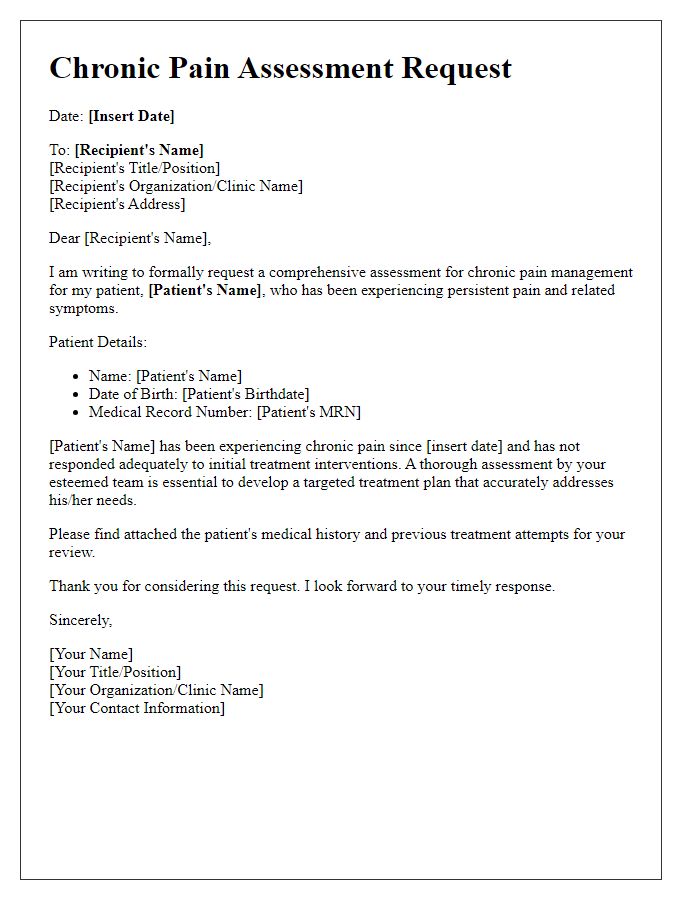
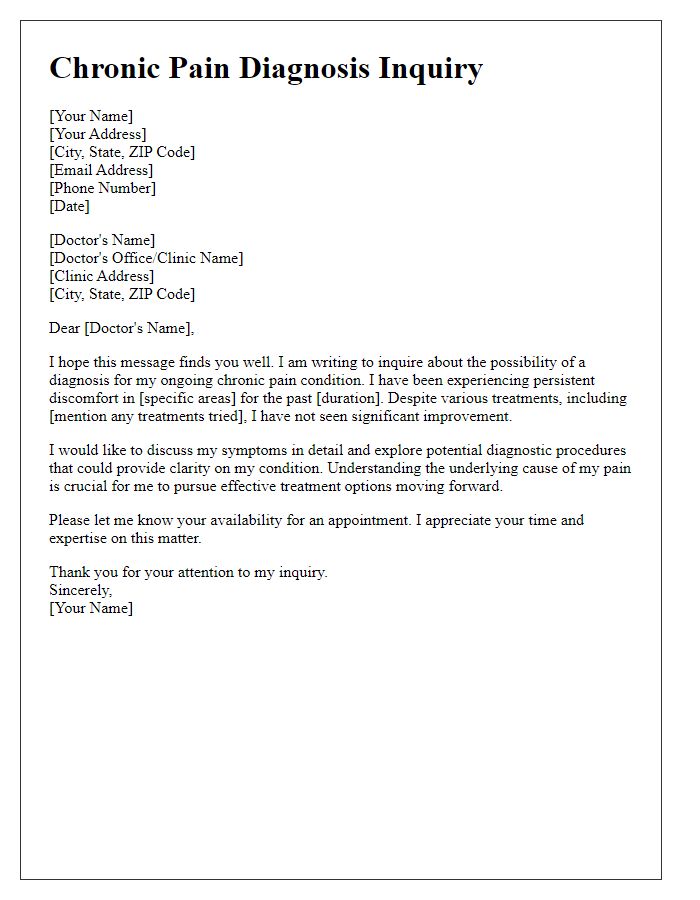
Are you navigating the complex and often frustrating journey of a chronic pain evaluation? If so, you're not alone, as many individuals find themselves uncertain about the necessary steps and documentation required for a thorough assessment. Understanding the evaluation process can empower you to advocate for your needs and secure the care you deserve. Join us as we delve into the essential components of this process and provide you with valuable insights to help you move forward confidently.
Patient Information and Medical History
Chronic pain evaluation necessitates a comprehensive understanding of the patient's medical background and symptomatology. The patient, aged 45 years, presents with a history of osteoarthritis (commonly affecting weight-bearing joints) and fibromyalgia (characterized by widespread musculoskeletal pain). Past medical records indicate an initial diagnosis of rheumatoid arthritis at age 30, managed by various non-steroidal anti-inflammatory drugs (NSAIDs), including ibuprofen and naproxen. Family history reveals a pattern of chronic pain conditions, with both parents experiencing similar ailments. The patient reports persistent pain levels averaging 7 out of 10 on the pain scale, impacting daily activities, sleep quality, and overall quality of life. Associated symptoms include fatigue, depression, and anxiety, complicating the overall pain management strategy. Current medication regimen includes gabapentin and duloxetine, prescribed to alleviate neuropathic pain and improve mood, respectively. Previous interventions encompass physical therapy and acupuncture, yielding limited relief. This detailed patient profile serves as a foundation for tailoring an effective pain management approach.
Symptom Description and Duration
Chronic pain, often characterized by persistent discomfort lasting more than three months, requires thorough evaluation to determine its origin and impact. Patients frequently describe their symptoms as varying in intensity; for instance, a pain scale from 1 to 10 can range from a dull ache at 3 to excruciating sensations at 10. Specific locations, such as the lower back or knees, contribute to functional limitations, making daily tasks challenging. Duration of these symptoms can vary from episodes of sharp pain occurring intermittently over weeks to a constant throbbing sensation present daily for years. Additionally, factors such as inflammation, emotional stress, and previous injuries, including falls or surgeries, can exacerbate chronic pain conditions, highlighting the necessity for a multidimensional assessment approach.
Impact on Daily Activities and Quality of Life
Chronic pain conditions, often characterized by persistent discomfort lasting more than three months, significantly hinder daily activities and overall quality of life. Common conditions like fibromyalgia or arthritis affect physical functions, limiting mobility (often resulting in difficulty walking or standing for prolonged periods). Many individuals experience fatigue due to disrupted sleep patterns caused by pain, leading to reduced productivity at work or school. Emotional well-being suffers due to feelings of frustration and isolation, impacting mental health conditions such as anxiety and depression. Social interactions diminish, with individuals avoiding gatherings or activities they once enjoyed, further contributing to a cycle of loneliness. The economic impact is also profound, with increased medical expenses and potential loss of income due to an inability to work, affecting financial stability.
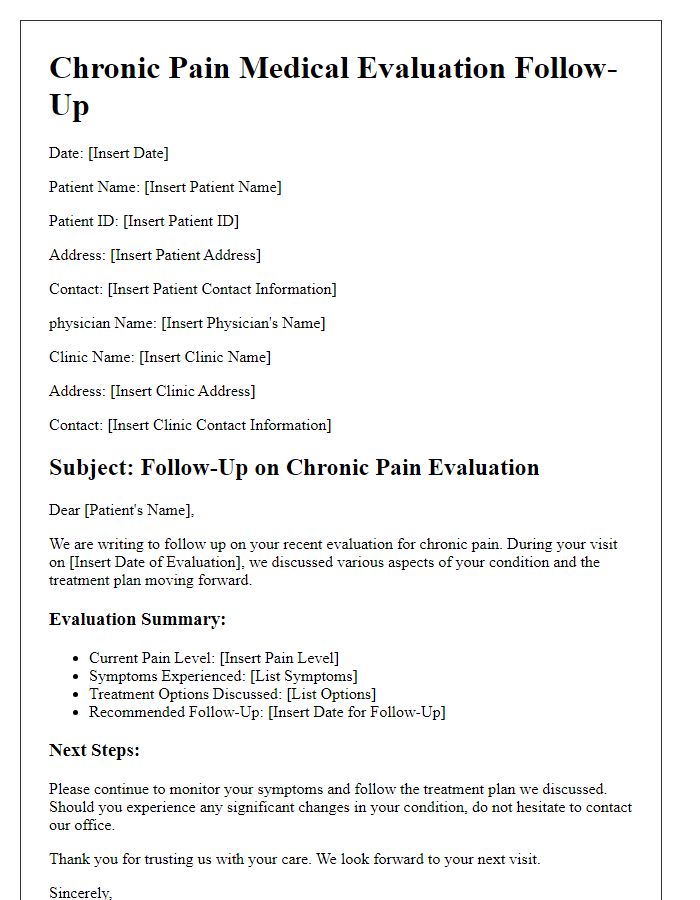
Current and Previous Treatments
Chronic pain management involves a comprehensive evaluation process that includes detailed documentation of current and previous treatments undertaken by the patient. Current treatments may include medication regimens such as Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), opioids, or antidepressants specifically prescribed for pain relief, often administered at doses tailored to individual tolerance, often dosed in milligrams. Physical therapy sessions, commonly occurring two to three times a week, focus on improving mobility and strength tailored to the patient's specific diagnoses, such as fibromyalgia or osteoarthritis. Complementary therapies, including acupuncture, massage therapy, or cognitive behavioral therapy, are also vital in addressing both the physical and psychological aspects of chronic pain. Previous treatments may include invasive procedures like epidural steroid injections performed in a clinic setting or surgical interventions such as joint replacements or spinal fusion conducted in a hospital environment. Documenting the timelines of previous treatments, patient responses, and any side effects encountered is crucial for formulating an effective management plan. Regular follow-ups and patient-reported outcomes inform ongoing adjustments necessary for optimizing care and improving quality of life.
Specialist Referrals and Future Recommendations
Chronic pain evaluation requires meticulous assessment from healthcare professionals across various specialties. The process often begins with initial consultations at pain management clinics, where practitioners gather detailed patient histories (including pain duration, intensity, and impact on daily activities). Specialist referrals typically include physiatrists, rheumatologists, and neurologists, each contributing unique insights into underlying conditions such as fibromyalgia or neuropathy. Diagnostic imaging (like MRIs and X-rays), blood tests, and psychological evaluations play crucial roles in diagnosis. Recommendations for future care may involve multidisciplinary approaches, incorporating physical therapy, medication management, and possibly interventions such as nerve blocks or cognitive-behavioral therapy. Adherence to follow-up schedules, generally within three to six months, ensures ongoing support and optimization of treatment plans tailored to individual patient needs.


Comments