When it comes to surgical procedures, having a clear understanding of the consent process is crucial for both patients and medical professionals. Many individuals may feel overwhelmed by the paperwork and technical jargon, which can lead to confusion or uncertainty about what they're agreeing to. It's important to clarify any questions or concerns, as informed consent is essential to ensure patients feel comfortable and empowered in their healthcare decisions. So, let's dive deeper into the nuances of surgical consent and explore what you need to know before the big day!
Patient identification details
When obtaining surgical consent, accurate patient identification details are crucial. These details typically include the patient's full name, date of birth (usually formatted as month/day/year), medical record number (a unique identifier assigned to the patient), and contact information (such as phone number or email). Additional identifiers may include the patient's address and insurance information for billing purposes. Ensuring that these details are correct helps to avoid potential errors during the surgical process, supports the patient's safety, and enhances communication between medical staff. It's essential to verify these details against official documentation, such as a driver's license or national ID card, particularly in high-stakes surgical environments.
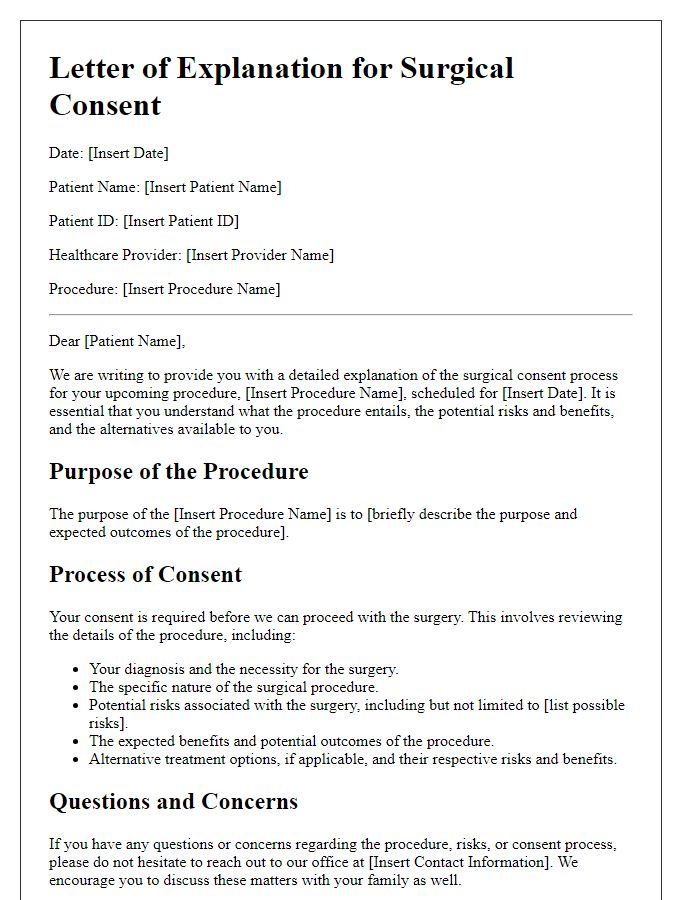
Detailed description of the surgical procedure
Surgical consent clarification involves an in-depth explanation of the specific operation to be performed, such as laparoscopic cholecystectomy, a minimally invasive procedure for gallbladder removal. Surgeons utilize a laparoscope, a thin tube with a camera, inserted through small incisions in the abdomen, typically about 5 to 10 millimeters in size. The procedure aims to alleviate symptoms related to gallstones, including severe abdominal pain and nausea, impacting approximately 10 to 15 percent of adults in the United States. The surgical team closely monitors vital signs throughout the operation, which usually lasts between 1 to 2 hours. Post-operative care includes potential risks such as infection or bleeding at incision sites, with recovery time generally spanning 1 to 2 weeks before resuming normal activities.
Potential risks and complications
Surgical procedures, such as appendectomies or knee replacements, carry inherent risks and complications that patients must understand prior to consenting. Infection rates for surgical sites can range from 1% to 3%, depending on the procedure and patient health. Anesthesia-related complications, including severe allergic reactions or respiratory issues, occur in approximately 1 in 1,000 general anesthesia cases. Hemorrhage or excessive bleeding may necessitate blood transfusions in about 2% of surgeries. Additionally, patients face potential damage to surrounding structures, with nerve or organ injury occurring in 1% to 2% of certain procedures. Delayed recovery, leading to extended hospital stay or chronic pain, is also a consideration. Understanding these risks ensures informed consent and prepares patients for possible outcomes.
Alternatives and outcomes
Surgical consent clarification involves informing patients about their options, potential outcomes, and risks associated with procedures. Alternatives to surgery may include non-invasive treatments such as medication, physical therapy, or lifestyle changes, depending on the medical condition. It's essential to discuss the likelihood of success for each alternative, considering average recovery times and potential side effects. Outcomes of surgical procedures often vary; for example, joint replacements can lead to a significant reduction in pain (over 70% improvement in some cases) but may carry risks like infection (occurring in 1-2% of cases) or complications from anesthesia. Providing patients with comprehensive information fosters informed decision-making, allowing them to weigh the benefits and drawbacks of each option effectively.
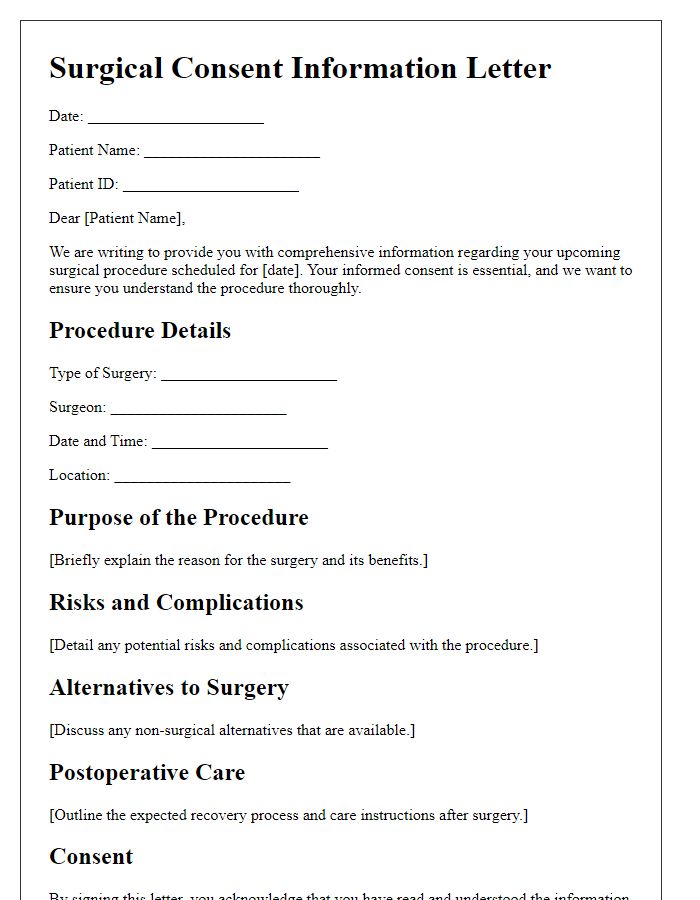
Confirmation of understanding and consent
A surgical consent form plays a crucial role in confirming that patients fully understand the risks, benefits, and alternatives associated with surgical procedures. This form is typically presented in a healthcare setting, often in hospitals like Mayo Clinic or Cleveland Clinic, where a detailed explanation of the specific surgery, such as laparoscopic cholecystectomy to remove the gallbladder, is given. Patients might be informed about potential risks, including infection rates (approximately 1-3%), anesthesia complications (affecting 1 in 10,000 patients), and the likelihood of needing follow-up procedures. Understanding is emphasized through discussions around recovery time (often ranging from 1 to 2 weeks) and post-operative care instructions. The patient's signature signifies not just consent but also comprehension of the surgical process and associated medical terminologies, ensuring informed decision-making in regards to surgical interventions.
Letter Template For Surgical Consent Clarification Samples
Letter template of clarification request for surgical procedure understanding


Comments