Are you feeling puzzled by some unusual neurological symptoms? It can be overwhelming to navigate the complexities of brain health and the myriad factors that could be at play. Understanding your symptoms is a crucial first step in seeking the right care and getting answers. If you'd like to learn more about assessing neurological symptoms and discovering the pathways to diagnosis and treatment, keep reading!
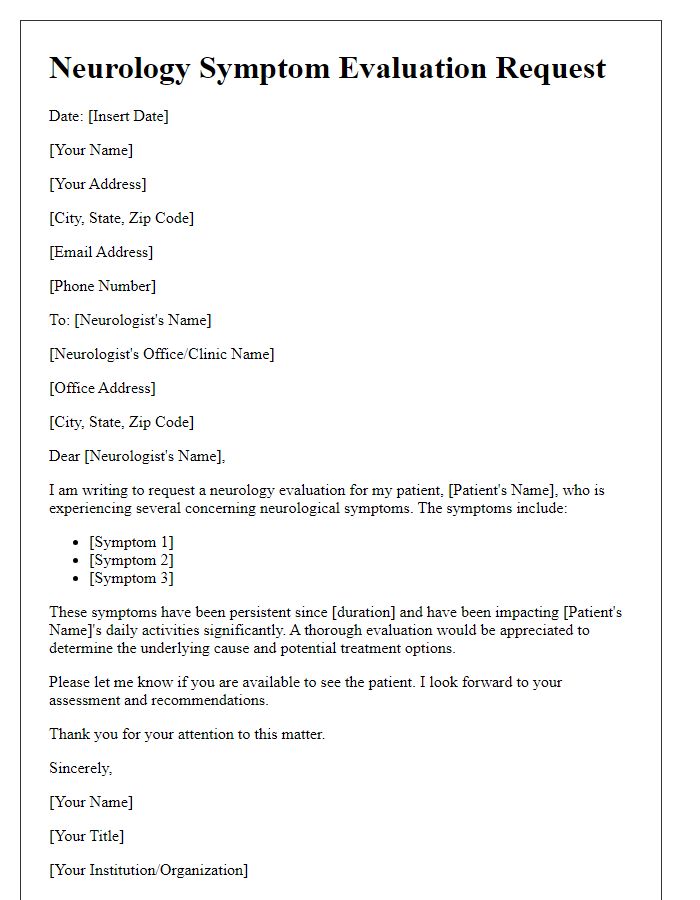
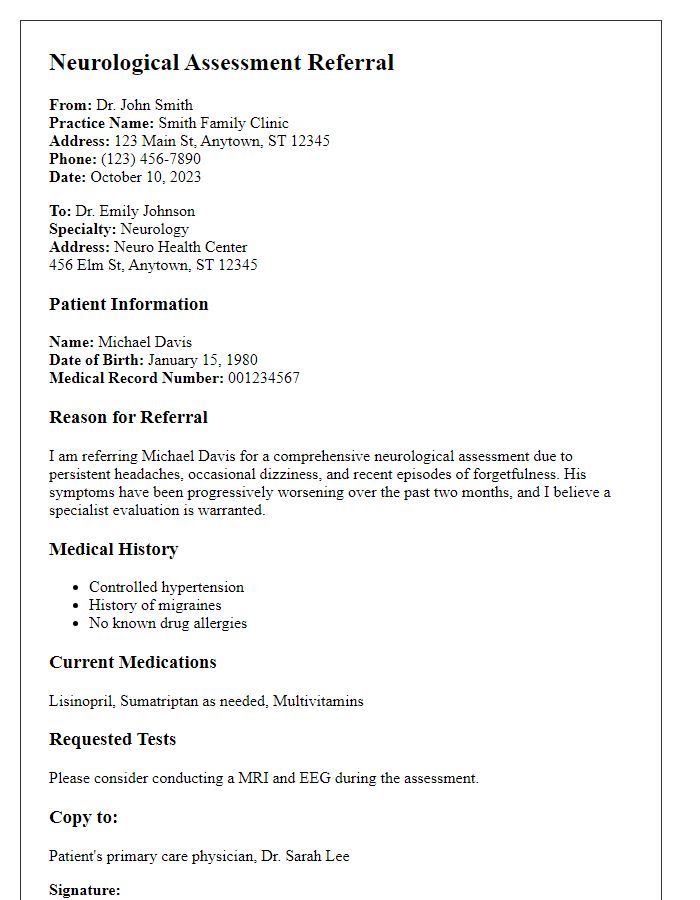
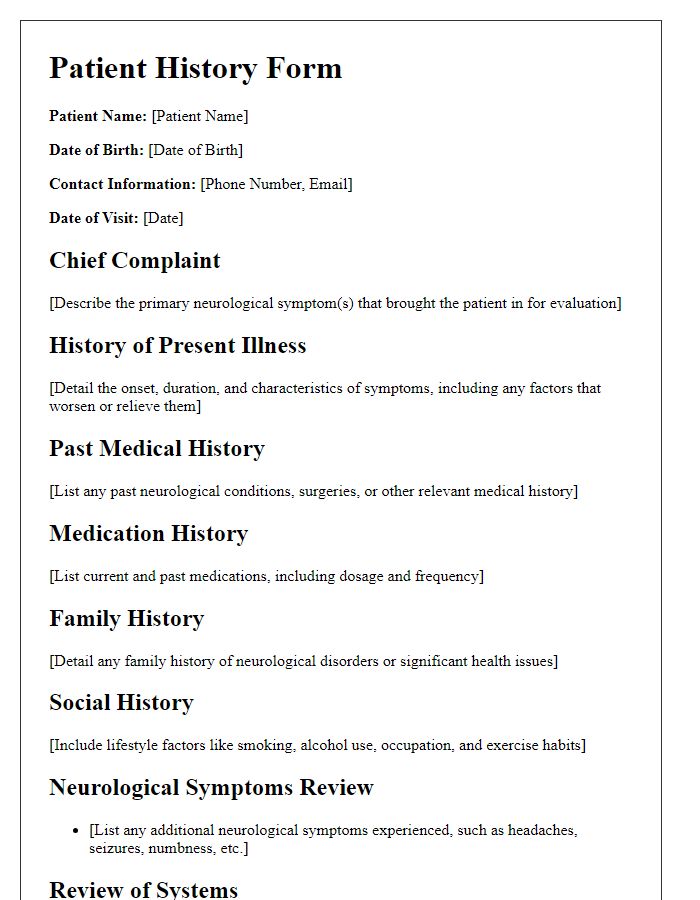
Patient's demographic information
Patient demographic information includes age, gender, race (Caucasian, African American, Hispanic, etc.), ethnicity (Hispanic or Latino, Not Hispanic or Latino), address (including city, state, and zip code), and contact number. Additional details may include occupational history (current job and prior employment), education level (high school, college, graduate degree), date of birth (specific day, month, year), and marital status (single, married, divorced). Notable medical history involves neurological disorders (epilepsy, multiple sclerosis) and family history of neurological conditions (Alzheimer's disease, Parkinson's disease). Emergency contacts can play an important role in severe cases, indicating immediate relatives (spouse, parent, sibling) and their phone numbers for quick communication during assessments.
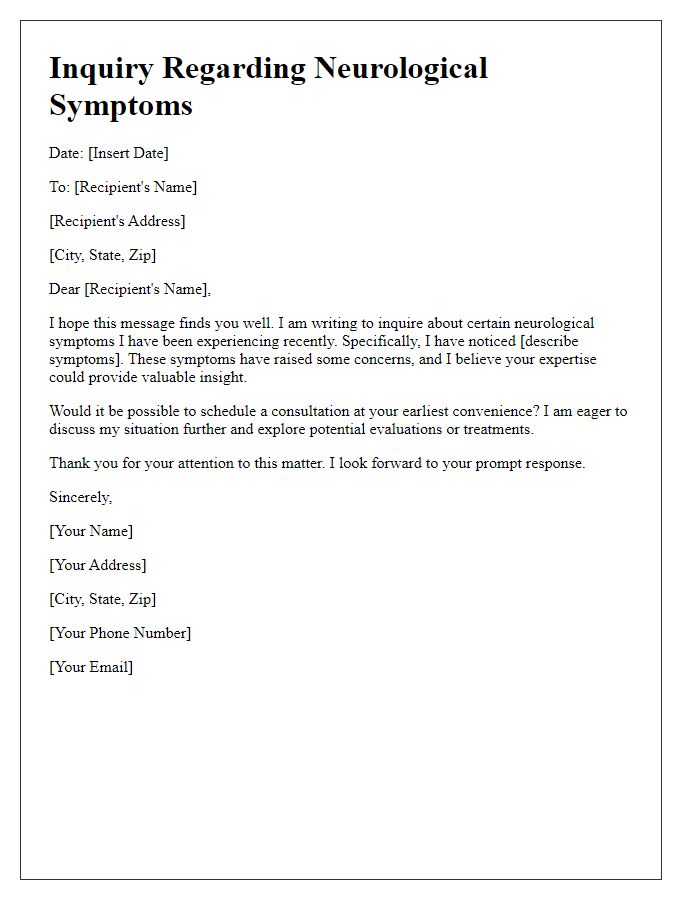
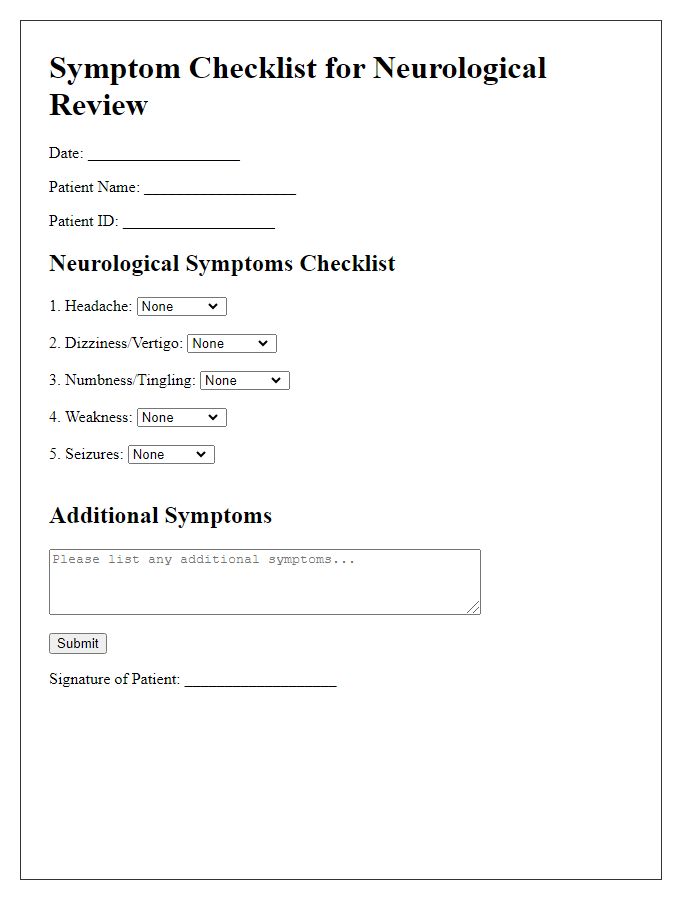
Detailed description of symptoms
Neurological symptoms such as persistent headaches often experienced in migraine patients can be accompanied by aura manifestations like visual disturbances or sensory changes. Additionally, seizures may present as episodes of temporary confusion, muscle spasms, or loss of consciousness, affecting daily activities and quality of life. Cognitive impairments, including memory loss or difficulty concentrating, could indicate conditions like dementia or traumatic brain injury, with varying impacts based on age and overall health. Motor function impairments like weakness or tremors may signal disorders such as Parkinson's disease or multiple sclerosis, making everyday tasks challenging. Sensory symptoms, including numbness or tingling in extremities, are commonly associated with neuropathy, potentially resulting from diabetes or vitamin deficiencies. Each symptom's duration, intensity, and triggering factors are crucial for accurate diagnosis and effective treatment planning.
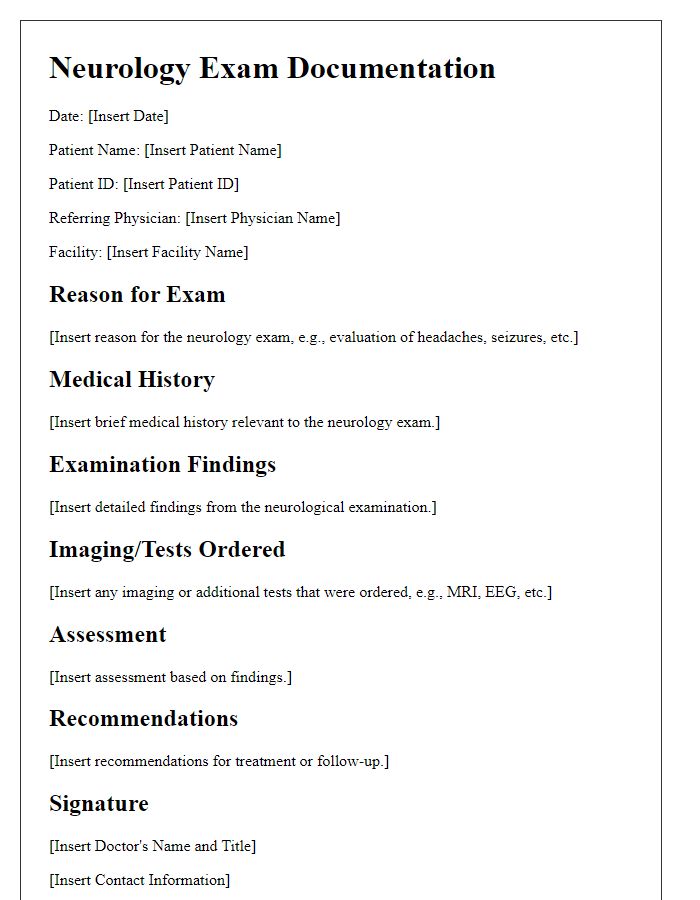
Onset and duration of symptoms
The onset and duration of neurological symptoms play crucial roles in diagnosing various conditions affecting the central and peripheral nervous systems. For instance, symptoms such as recurrent headaches may indicate tension-type headaches or migraines, typically displaying a gradual onset over several hours to days. Conversely, sudden onset of weakness, often distinguishing signs of a stroke, can manifest within minutes. Duration varies significantly; episodic migraines might last from four hours to three days, while transient ischemic attacks (TIAs) resolve within 24 hours. Monitoring these factors is essential for healthcare providers in assessing the patient's medical history and determining appropriate diagnostic tests, such as MRI or CT scans, to rule out serious conditions. Understanding these temporal patterns assists in narrowing down differential diagnoses and developing tailored treatment plans.
Medical history and medications
Neurological symptoms assessment involves a comprehensive review of a patient's medical history and current medications. Key aspects include past neurological conditions such as epilepsy or migraines and family history of neurodegenerative disorders like Alzheimer's disease or Parkinson's disease. Additionally, documentation of previous surgeries, injuries, or treatments related to neurological health is critical. Current medications must be meticulously listed, including dosage and frequency, highlighting any antiepileptic drugs, antidepressants, or anti-anxiety medications that may influence symptoms. Monitoring for side effects or interactions from polypharmacy is essential, especially in elderly patients or those with comorbidities. This thorough approach facilitates accurate diagnosis and tailored treatment plans in neurology.
Family history and lifestyle factors
Assessment of family history regarding neurological symptoms can reveal genetic predispositions to conditions such as multiple sclerosis (MS) or Alzheimer's disease. Surveys indicate that first-degree relatives, like parents or siblings, significantly increase risks; for instance, individuals with an affected sibling have a 2-3 times higher chance of developing MS. Lifestyle factors also play a critical role in neurological health. Sedentary behavior correlates with increased rates of neurodegenerative diseases, while a balanced diet rich in omega-3 fatty acids (found in fish like salmon) and antioxidants (from fruits and vegetables) contributes positively to brain health. Stress management techniques, such as mindfulness or regular physical activity, can mitigate the risk of cognitive decline. Understanding these connections is essential for evaluating individual neurological health and formulating an effective management plan.



Comments