Are you looking for a way to ensure seamless continuity of care with your primary care physician? Maintaining a strong relationship with your healthcare provider is essential for managing your health effectively, and a well-crafted letter can help facilitate this connection. In this article, we'll explore the key elements to include in your letter to your physician, ensuring your needs and preferences are clearly communicated. Join us as we guide you through the process and provide tips for creating an impactful message that fosters ongoing collaboration!
Message Clarity and Tone
Clear communication with a primary care physician (PCP) is vital for maintaining continuity of care. A consistent tone that balances professionalism with warmth fosters a trusting patient-physician relationship. Specific details regarding patient history, including medications, allergies, and previous treatments, should be conveyed upfront for comprehensive understanding. Scheduled follow-up appointments serve as benchmarks for ongoing health management, ensuring that chronic conditions are addressed in a timely manner. Incorporating patient feedback in treatment plans enhances engagement, while reminders for preventive screenings such as blood pressure checks and cholesterol assessments contribute to proactive health measures. Overall, maintaining clarity in messages and a respectful tone encourages patients to voice concerns and assures them that their healthcare is a shared responsibility.
Personalized Patient Information
Continuity of care in primary healthcare settings ensures patients receive consistent and coordinated medical attention, fostering better health outcomes over time. Personalized patient information, including medical history, allergy documentation, and recent laboratory results, enhances this continuity. For instance, a patient's chronic conditions, such as diabetes (which affects approximately 34 million Americans) and hypertension, require regular monitoring and specific treatment plans tailored to individual needs. Effective communication between healthcare providers and patients about medication schedules, appointment reminders, and lifestyle recommendations plays a critical role in maintaining health. Additionally, the integration of technology, such as electronic health records, facilitates seamless sharing of information across different healthcare settings, allowing for a comprehensive understanding of the patient's health journey and preferences.
Medical History Overview
Creating a comprehensive medical history overview for a primary care physician can significantly enhance continuity of care. This document includes critical information such as previous diagnoses (e.g., hypertension from 2015), major surgeries (e.g., appendectomy in 2018), and any allergies (e.g., penicillin allergy). Medication lists should encompass current prescriptions (e.g., lisinopril 10 mg daily for blood pressure management), dosages, and durations of treatment. Furthermore, pertinent family medical history (e.g., father with type 2 diabetes, mother with breast cancer) can provide insights into potential hereditary conditions. Lifestyle factors, including smoking status (e.g., nicotine use for five years until 2021), alcohol consumption (e.g., moderate intake of one glass of wine per week), and exercise habits (e.g., walking 30 minutes daily), should also be documented. This thorough overview ensures that the primary care physician has a complete picture, facilitating effective monitoring and tailored healthcare strategies.
Continuity of Care Plan
A Continuity of Care Plan outlines the coordinated approach in patient management among healthcare providers, particularly emphasizing primary care physicians' role. A seamless transition among specialists ensures consistent monitoring for chronic conditions such as diabetes or hypertension, particularly for patients undergoing treatments requiring multi-disciplinary input. Regular follow-up appointments scheduled at intervals (e.g., every three months) can facilitate timely adjustments in treatment plans. Utilizing electronic health records (EHR) enables information sharing regarding medication changes, allergy updates, or test results among physicians. Furthermore, clear communication strategies, like designated contact points for patient inquiries, enhance patient engagement and satisfaction, which is especially important in communities with limited access to healthcare facilities.
Contact Information and Accessibility
Effective continuity of care in primary healthcare settings requires clear communication and accessibility for patients. Contact information, including phone numbers, email addresses, and office locations, plays a crucial role in maintaining a seamless patient-physician relationship. Primary care offices, such as those found in urban centers like New York City, should be easily reachable during business hours, typically from 8 AM to 5 PM, with an emergency contact hotline available after hours. Accessibility also includes provisions for patients with disabilities, ensuring they can navigate office spaces comfortably. Online patient portals enhance this experience, allowing individuals to schedule appointments, view medical records, and communicate with their healthcare providers efficiently. In 2023, the emphasis on telehealth options has further transformed accessibility, enabling patients in remote areas to receive care through video consultations.
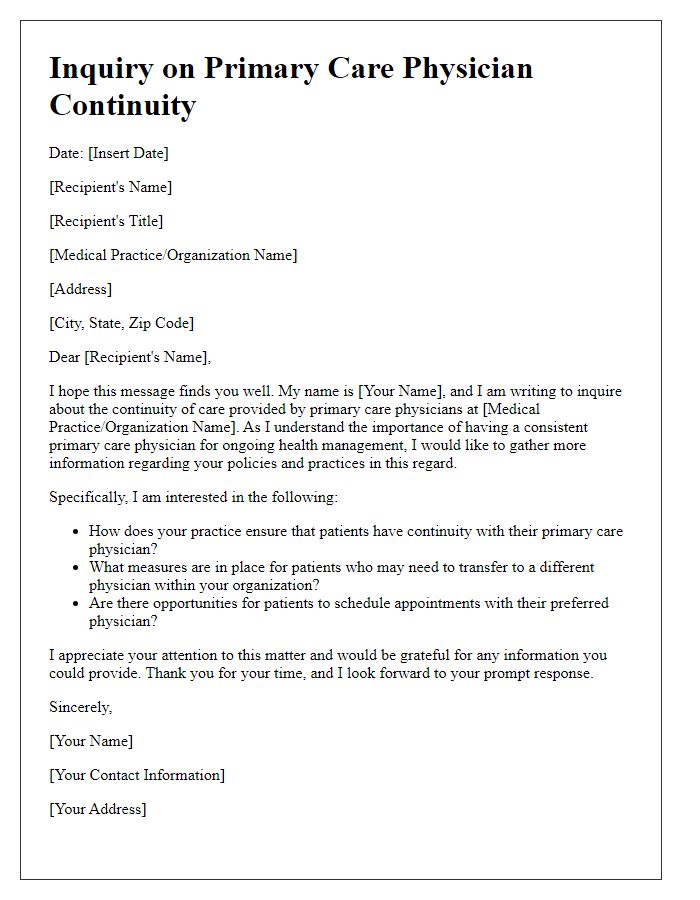
Letter Template For Primary Care Physician Continuity Samples
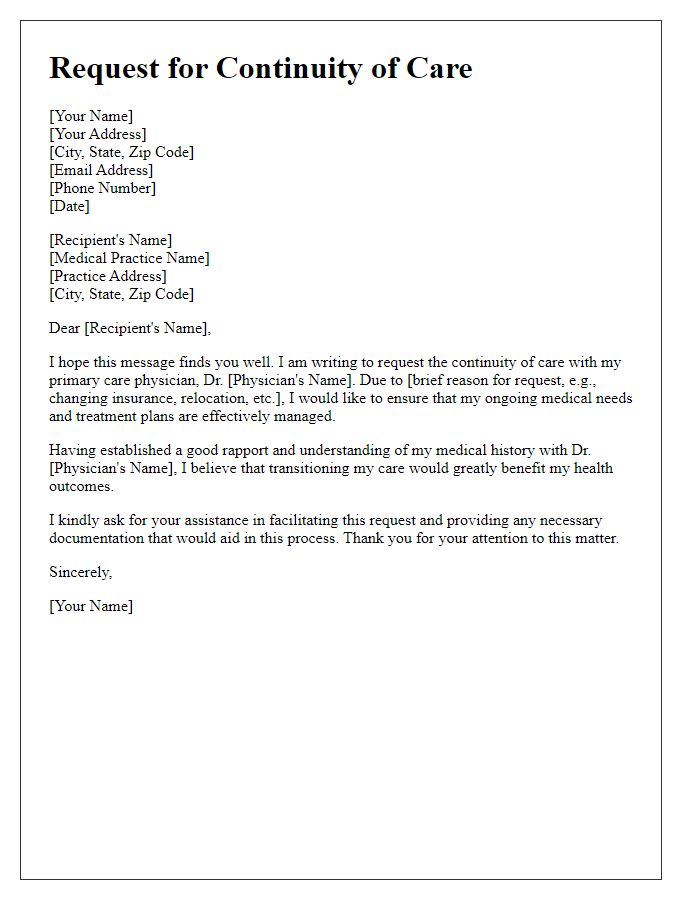
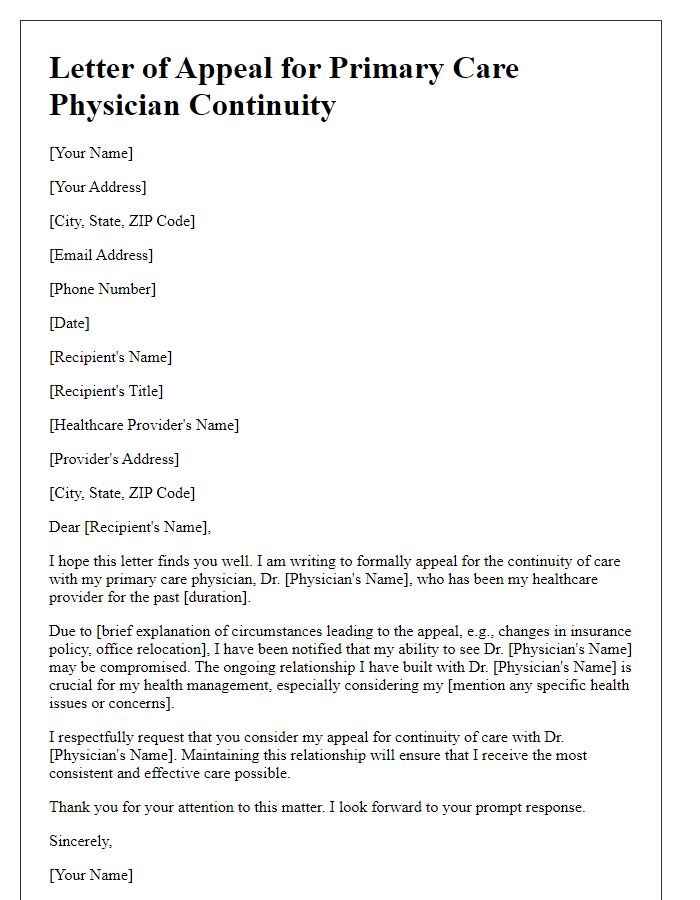
Letter template of request for primary care physician continuity of care.
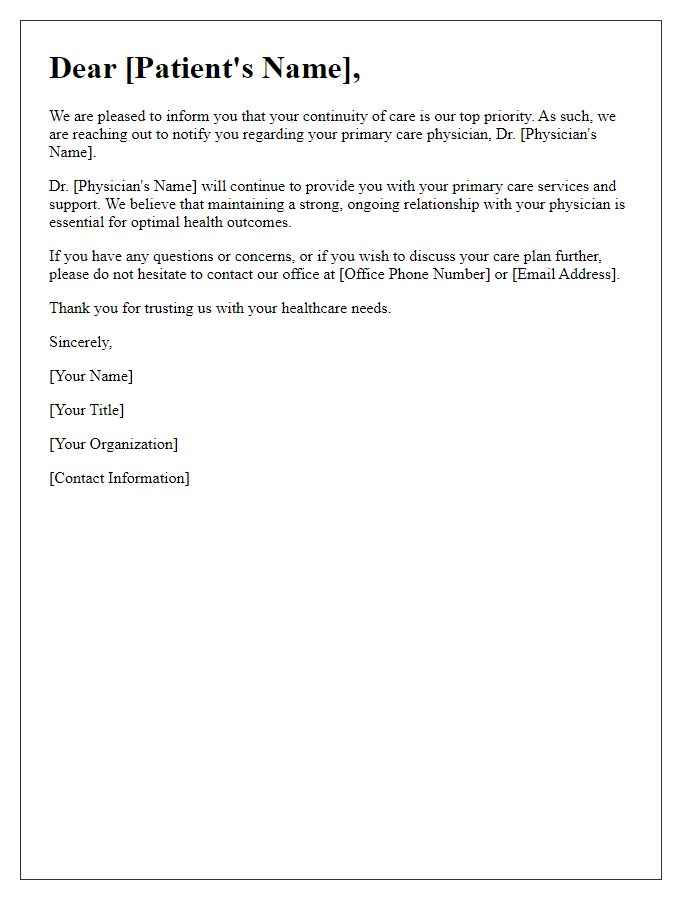
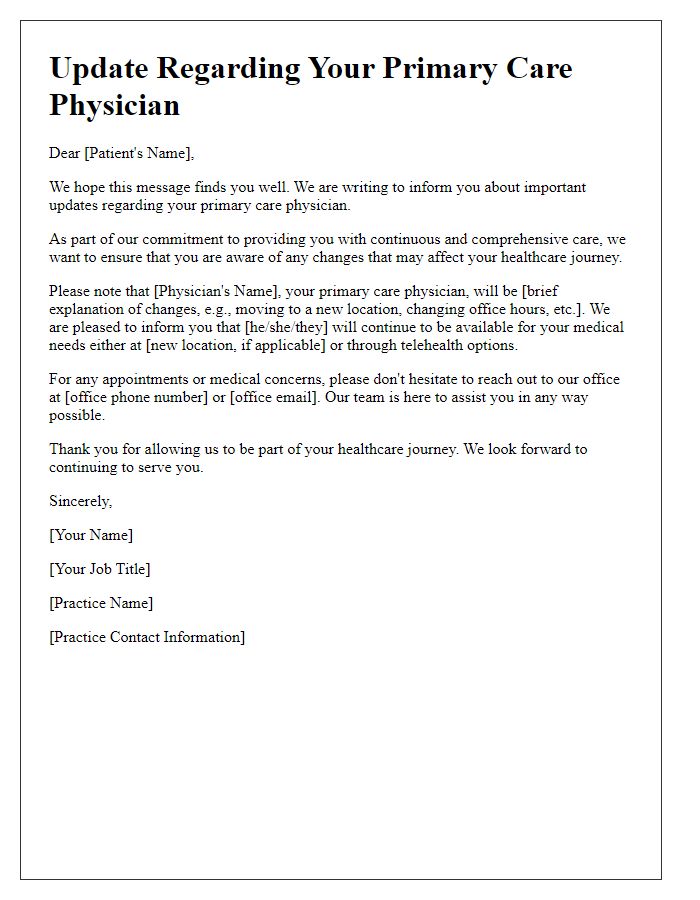
Letter template of notification about primary care physician continuity.
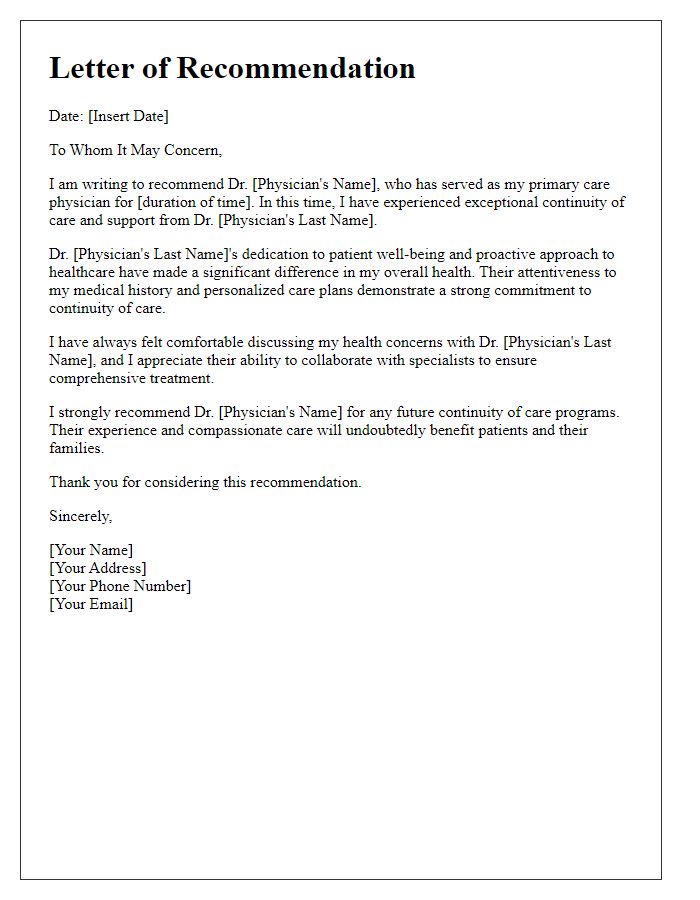
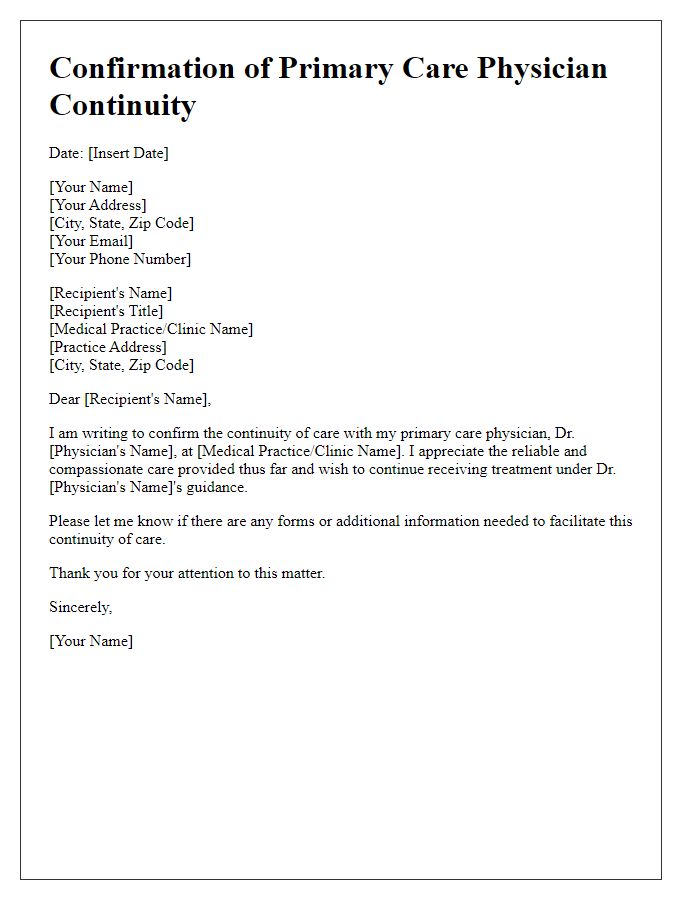
Letter template of recommendation for primary care physician continuity.


Comments