In today's fast-paced healthcare environment, ensuring patient eligibility for services is more crucial than ever. Navigating the complexities of insurance and coverage can be overwhelming, but a well-crafted verification letter can simplify the process. This template is designed to help healthcare providers communicate effectively with insurers, ensuring that patients receive the care they need without unnecessary delays. Ready to streamline your patient eligibility verification process? Let's dive in!
Patient and Provider Information
Patient eligibility verification ensures that healthcare providers can identify patient coverage with insurance plans before medical services are rendered. Accurate patient information includes full name, date of birth, and insurance policy details. Provider information consists of the healthcare facility's name, National Provider Identifier (NPI) number, and contact information. Verification processes often involve communicating with insurance companies, requiring details like member ID and group number. These steps help ascertain coverage levels, copayment responsibilities, and any pre-authorization needs for specific medical procedures or treatments. Proper documentation expedites the claims process and reduces denials.
Insurance Details
Patient eligibility verification involves assessing insurance details such as policyholder information, coverage limits, and specific plan benefits. In medical settings, insurance providers like Aetna, UnitedHealthcare, and Blue Cross Blue Shield are commonly involved. Policy numbers typically consist of alphanumeric characters uniquely identifying a patient's plan. It is critical to confirm coverage against procedures such as laboratory tests or specialist consultations, especially in cases requiring pre-authorization. Many insurance companies have specific eligibility criteria that dictate the extent of coverage for treatments like physical therapy or surgical procedures, often influenced by state regulations or the Affordable Care Act guidelines.
Eligibility and Benefits Verification
Eligibility and benefits verification serves as a critical process in the healthcare system, ensuring patients qualify for specific services before they receive treatment. This procedure typically involves checking insurance provider databases to confirm coverage details, co-payment requirements, and any pre-authorizations needed for procedures. Patients may present various forms of health insurance, including private plans like Blue Cross Blue Shield or public programs such as Medicare. Key benefits can include preventive services, hospital stays, and outpatient care, all of which have different eligibility criteria based on patient age, medical history, and policy specifics. Accurate verification protects both patients and providers from unexpected costs, enhancing the overall efficiency of healthcare delivery.
Services Requested or Scheduled
Patient eligibility verification is essential for ensuring access to healthcare services. Specific services requested, such as consultations or diagnostic imaging (e.g., MRI or CT scans), require prior approval based on individual insurance policies. Verification is typically conducted through detailed checks against health insurance provider databases (like Aetna or UnitedHealthcare) to confirm coverage details. Essential information includes patient identification details (e.g., date of birth, insurance ID), scheduled service dates, and the specific healthcare provider's National Provider Identifier (NPI) number. Accurate completion of this process helps prevent delays in service delivery and ensures that patients receive necessary care without unexpected out-of-pocket expenses.
Contact Information for Follow-up
Patient eligibility verification requires accurate contact information for follow-up inquiries. Essential details include the patient's full name, date of birth, and insurance policy number to streamline communication processes. Phone numbers (preferably mobile) should be provided to facilitate immediate outreach for clarifications. Email addresses are also vital for sending documents or additional requests promptly. Additionally, including secondary contacts, such as a family member or caregiver, is beneficial for instances where direct communication with the patient is not feasible. Verify that all information is current and accessible to ensure a smooth verification process.
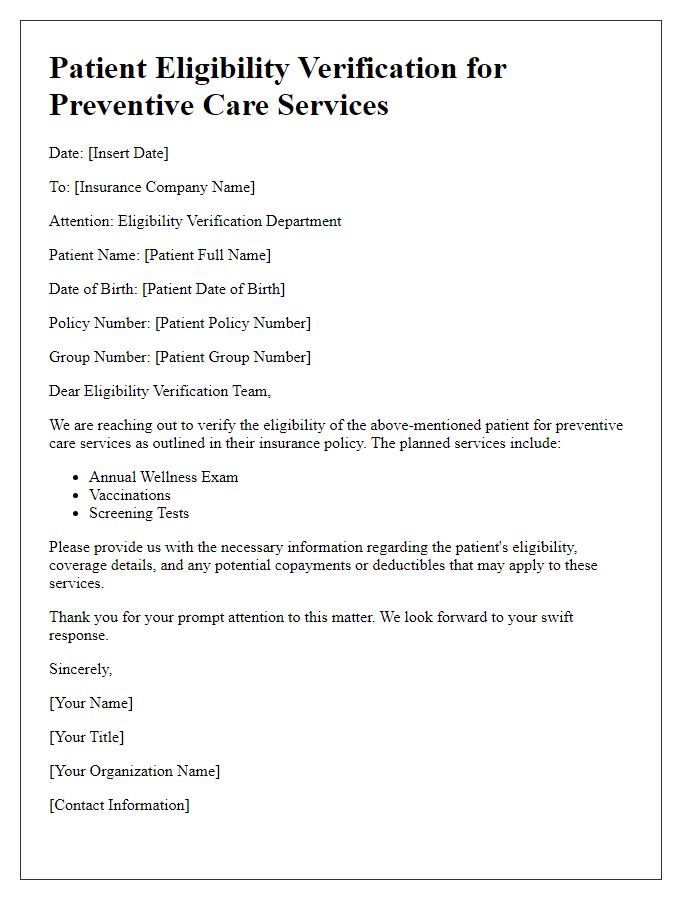
Letter Template For Patient Eligibility Verification Samples
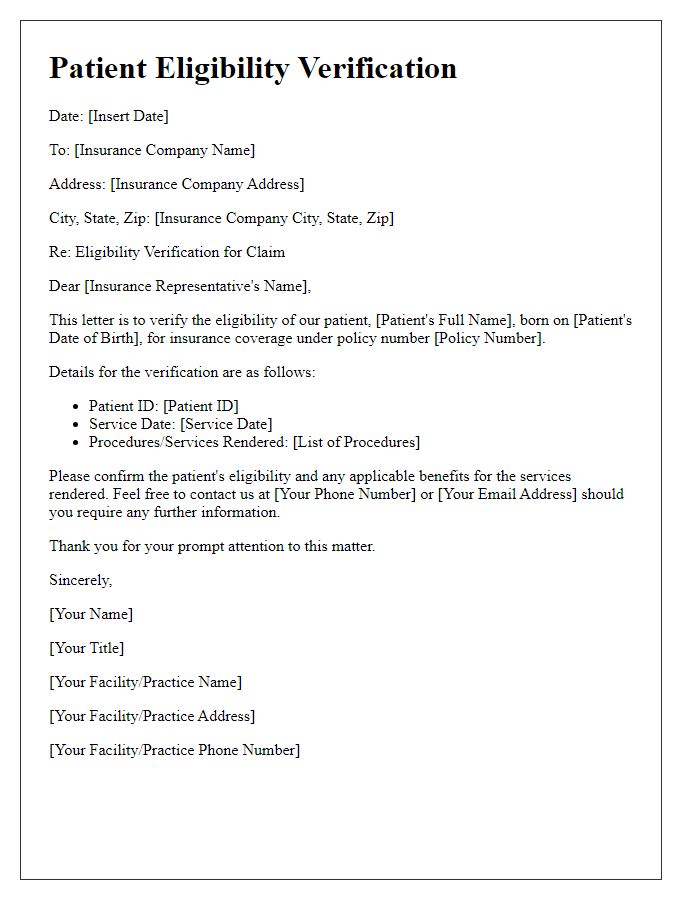
Letter template of patient eligibility verification for insurance claims.
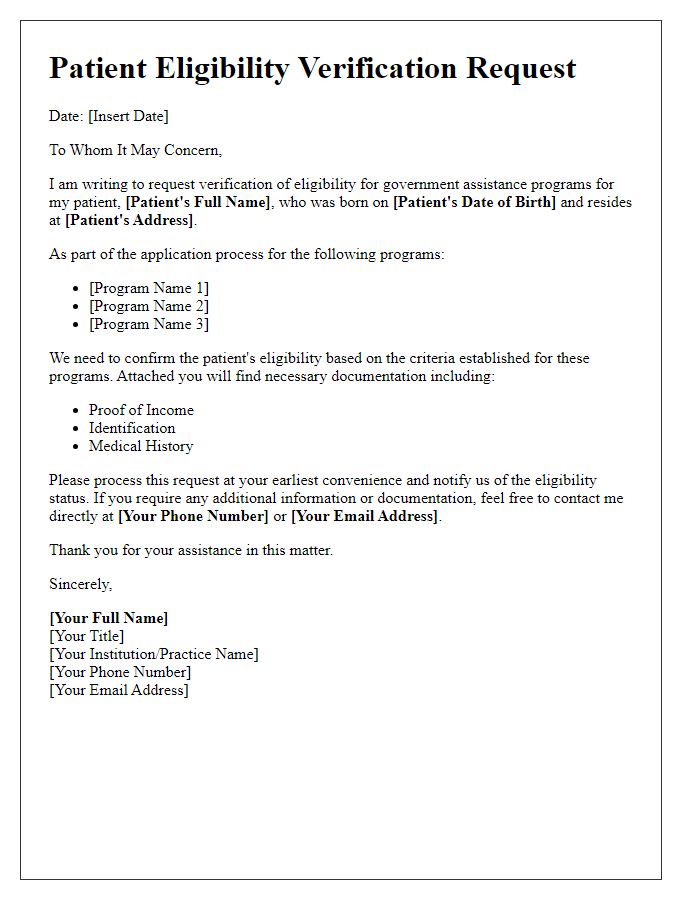
Letter template of patient eligibility verification for government programs.
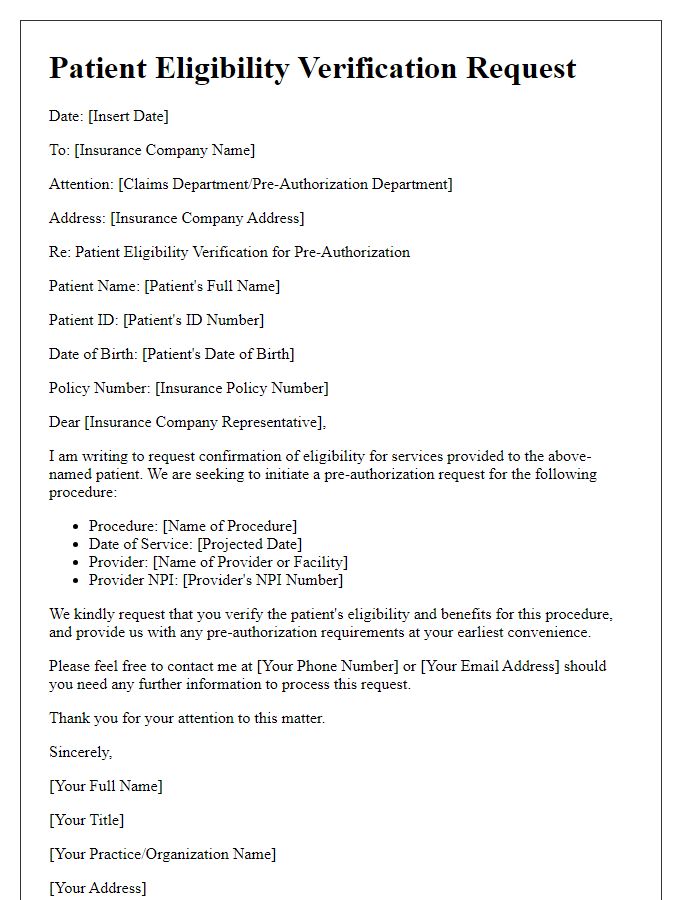
Letter template of patient eligibility verification for pre-authorization requests.
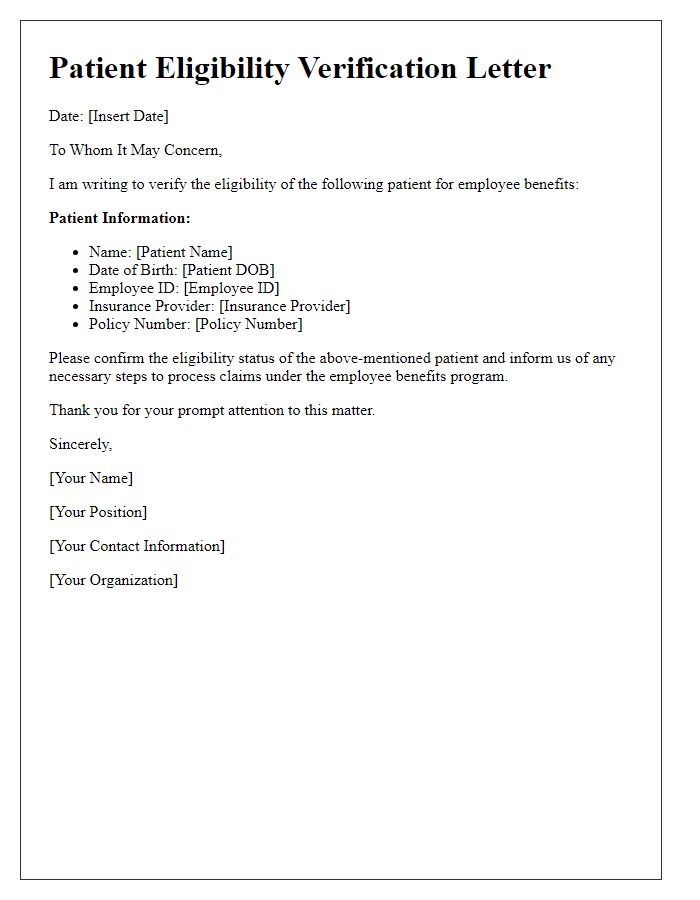
Letter template of patient eligibility verification for employee benefits.
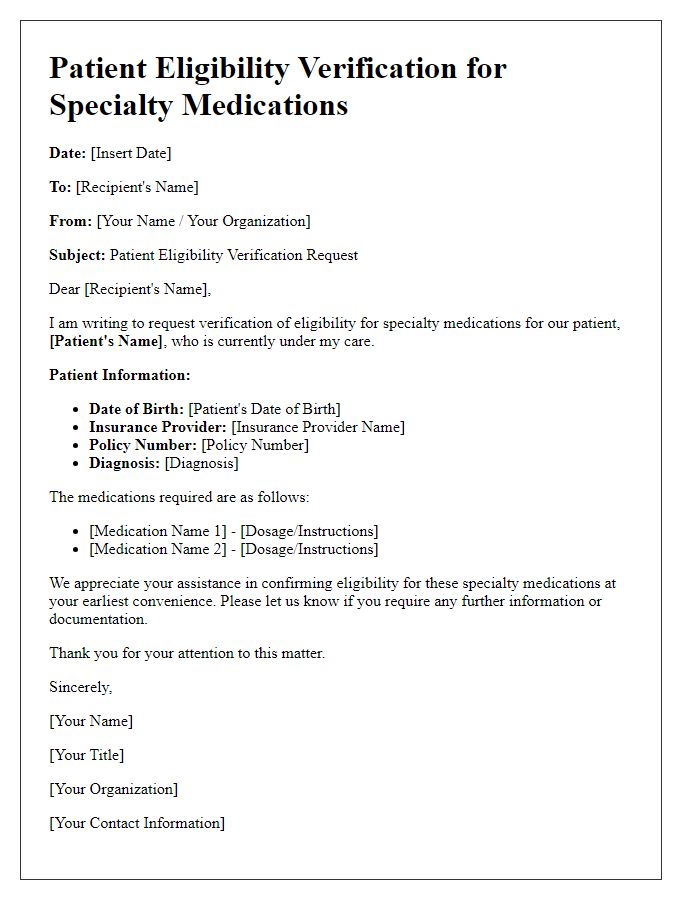
Letter template of patient eligibility verification for specialty medications.
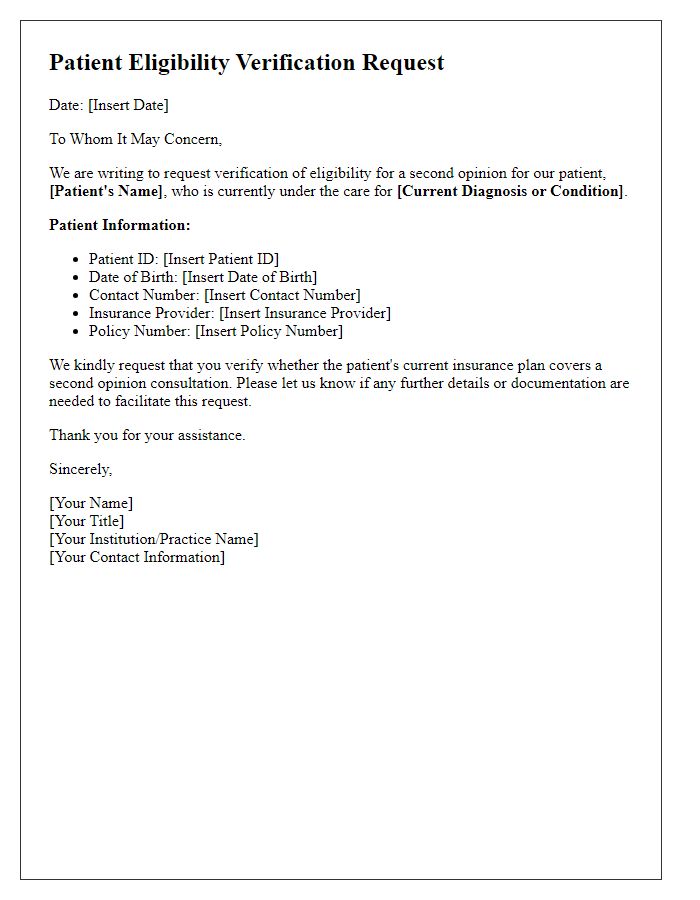
Letter template of patient eligibility verification for second opinions.
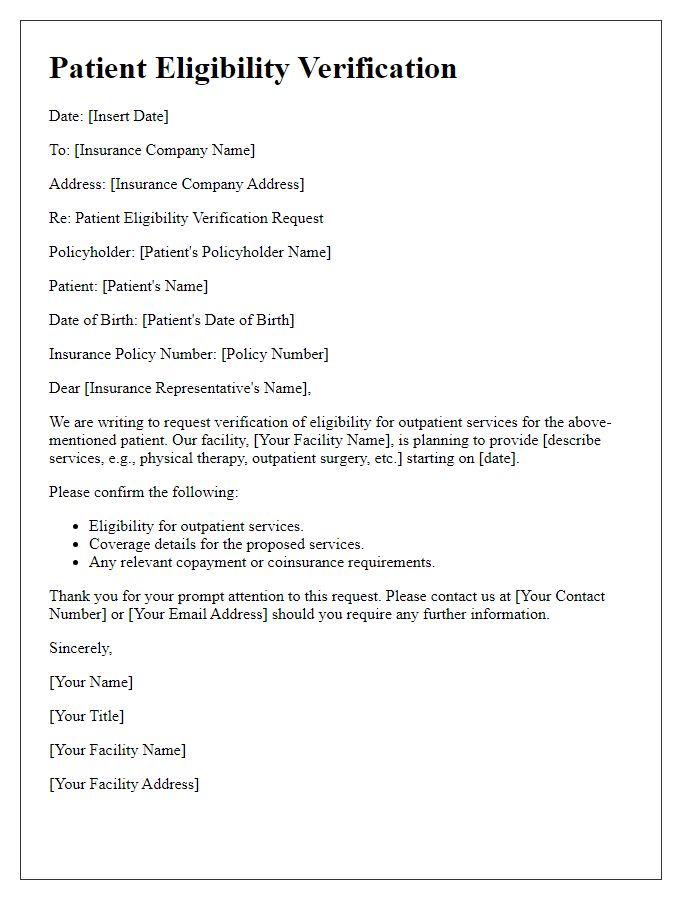
Letter template of patient eligibility verification for outpatient services.
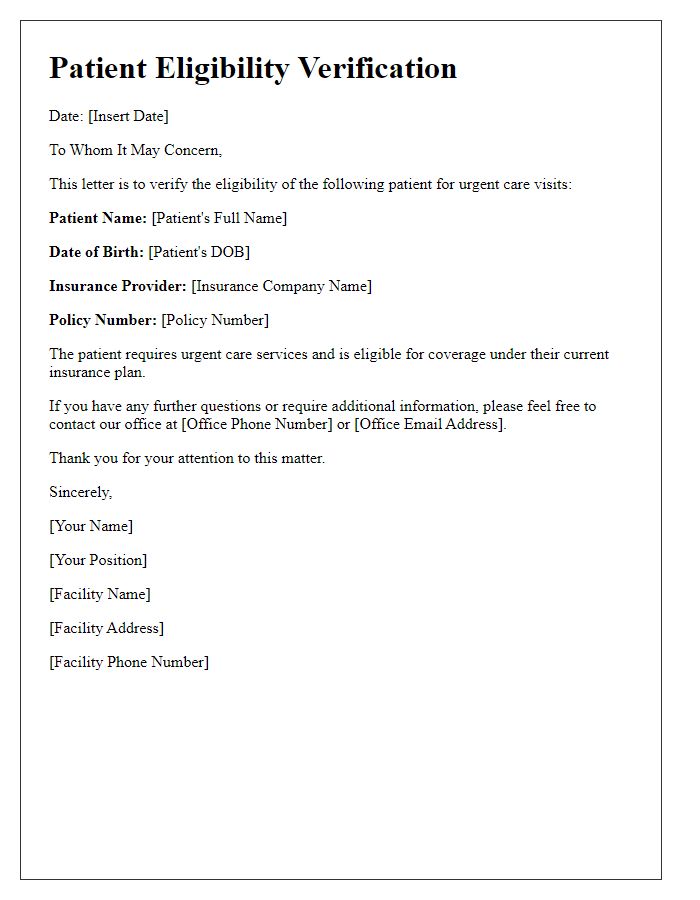
Letter template of patient eligibility verification for urgent care visits.
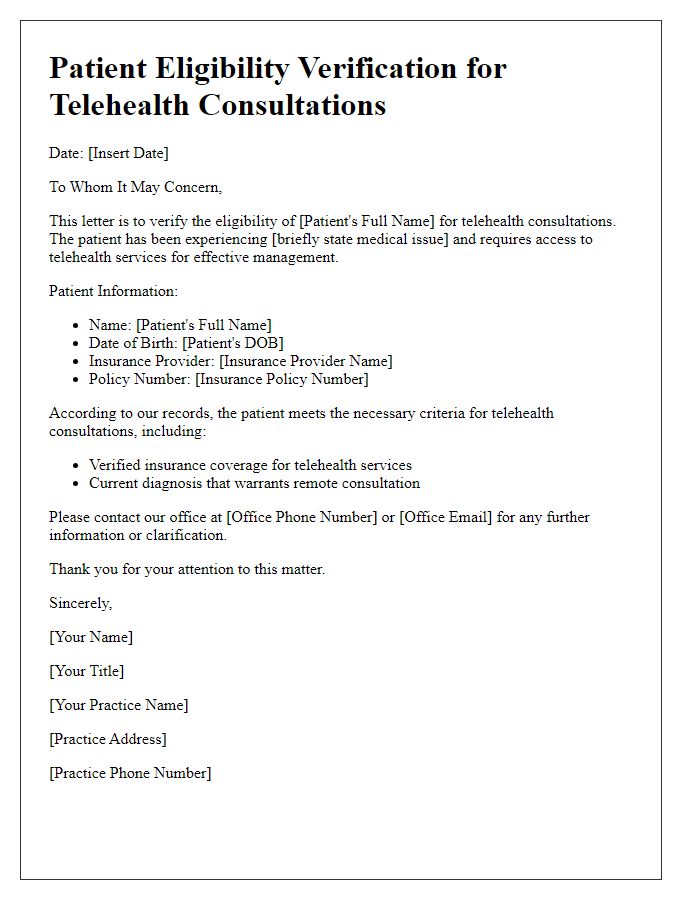
Letter template of patient eligibility verification for telehealth consultations.



Comments