Are you feeling confused about a recent bill from your healthcare provider? It's completely understandable, as medical billing can often feel like a labyrinth. In this article, we'll break down common billing inquiries and provide clear answers to help you navigate the process. So, let's dive in and unravel the mysteries of your patient billing questions together!
Patient Identification Information
Patient identification information is crucial for accurate billing and insurance processing in healthcare settings. Essential details include full name, date of birth (format: MM/DD/YYYY), account number, and insurance policy number. Incorrect or missing information can lead to delays in claims processing or billing disputes. Additionally, contact information such as phone number and mailing address ensures effective communication regarding billing statements or inquiries. Ensuring accuracy in patient identification also protects against fraud and identity theft in healthcare transactions, fostering a secure environment for both patients and providers. Prompt and thorough verification of these details is essential to maintain efficient operations within medical billing departments.
Billing Summary and Date Details
The patient billing summary provides a detailed overview of the charges incurred during hospital visits or medical procedures, specifying costs for services rendered and patient demographic information. Each entry includes the date of service, illustrating the timeline of procedures and consultations. For instance, a billing entry from March 15, 2023, may detail charges for a comprehensive exam, consultations, and laboratory tests. Itemized amounts clarify the total balance owed, which might include hospital fees, specialist services, and medication costs. Additional notes regarding insurance claims or payment arrangements can further assist in understanding outstanding balances and patient responsibilities.
Insurance and Payment Explanation
Patient billing inquiries often arise from confusion surrounding insurance coverage and payment responsibilities. Insurance companies, such as Aetna or Blue Cross Blue Shield, may have specific policies that dictate what procedures are covered under a patient's plan. The explanation of benefits (EOB) document clarifies details like deductibles (the amount patients pay before insurance coverage kicks in), copayments (fixed amounts paid for specific services), and coinsurance percentages (the portion of costs patients pay after their deductible is met). Medical services rendered at facilities like community hospitals or outpatient clinics may have varying payment structures, leading to potential discrepancies in patient billing. Clear communication regarding these factors, along with ensuring the patient's financial responsibility is accurately conveyed, is crucial for addressing inquiries effectively.
Contact Information for Further Assistance
Contact information (such as phone number, email address, and physical address) is essential for patients seeking assistance with billing inquiries. A dedicated billing department, often found within healthcare facilities like hospitals or clinics, typically operates during standard hours (e.g., 9 AM to 5 PM). Providing a direct line (e.g., a toll-free number) ensures that patients can easily reach representatives knowledgeable about their accounts or insurance claims. Additionally, email support allows for convenient documentation of concerns or questions, while a mailing address enables patients to send documents securely. Having this information readily accessible fosters trust and clarity in patient-provider financial interactions.
Privacy and Confidentiality Assurance
Patient billing inquiries often include concerns regarding privacy and confidentiality of personal health information. The Health Insurance Portability and Accountability Act (HIPAA) mandates strict guidelines for safeguarding patient data, ensuring that all billing records and personal information remain confidential. Institutions implement secure electronic systems (such as encrypted databases) to protect sensitive data during transmission and storage. Additionally, staff members are trained extensively on appropriate handling and sharing protocols to guarantee compliance with legal standards. Patients can feel secure knowing that their billing inquiries are handled with the utmost discretion, protecting their health information from unauthorized access while facilitating transparent communication about charges and insurance processes.
Letter Template For Patient Billing Inquiry Response Samples
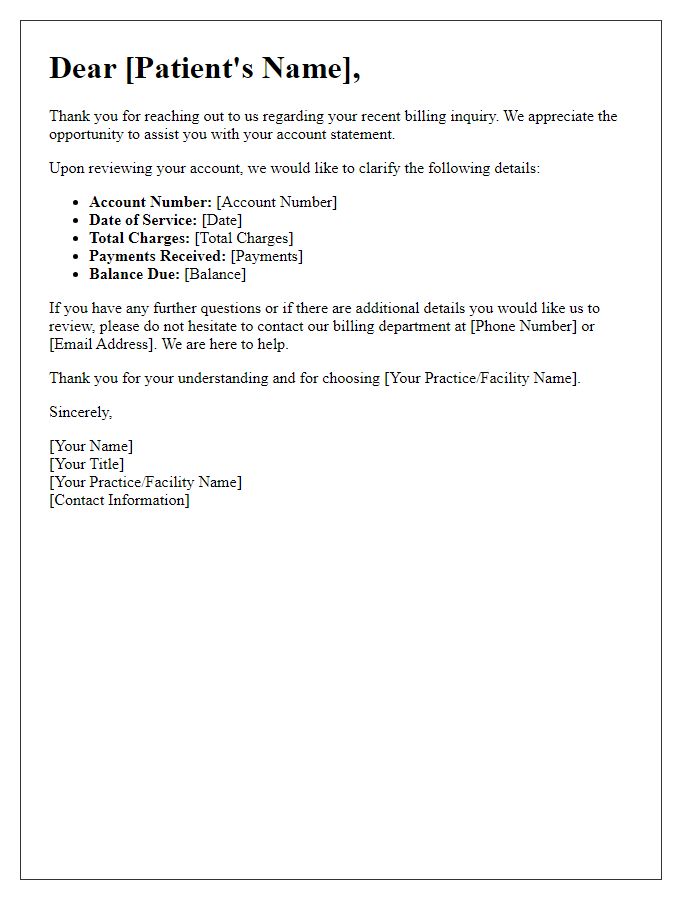
Letter template of response to patient billing inquiry regarding account statement.
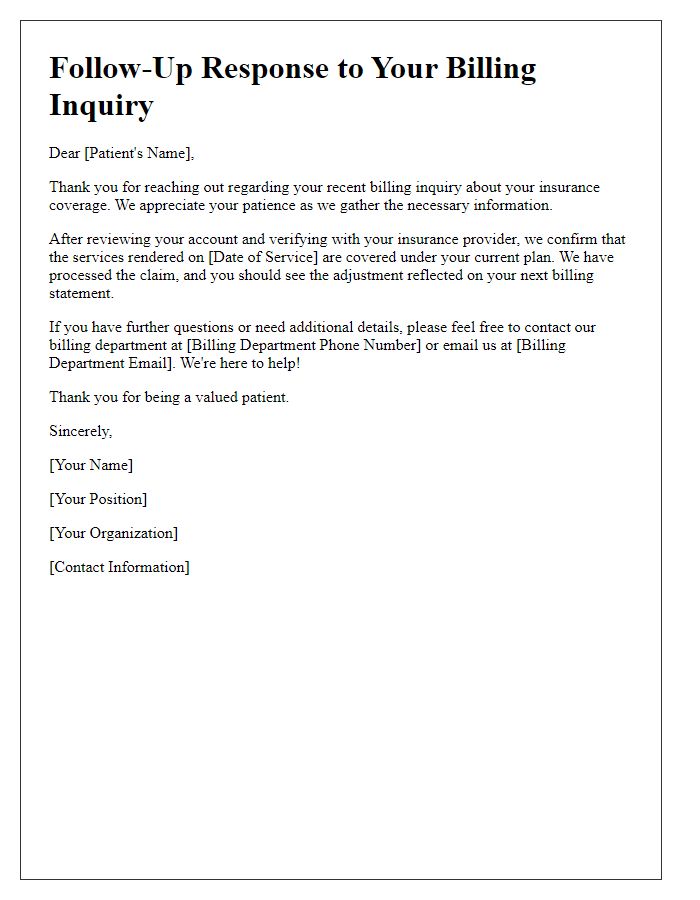
Letter template of follow-up response to patient’s billing inquiry about insurance coverage.
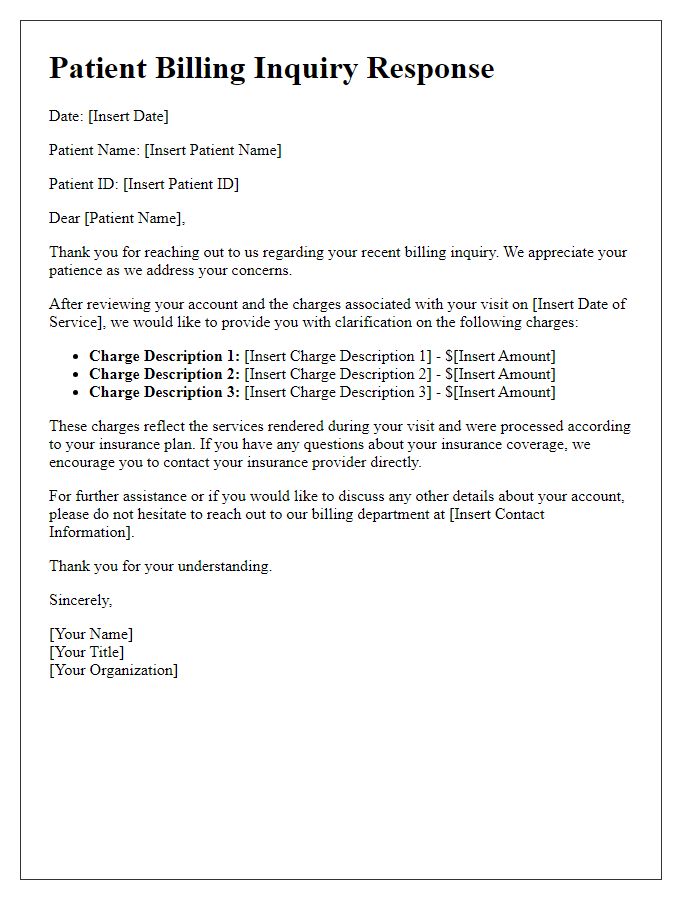
Letter template of explanation for charges in response to patient billing inquiry.
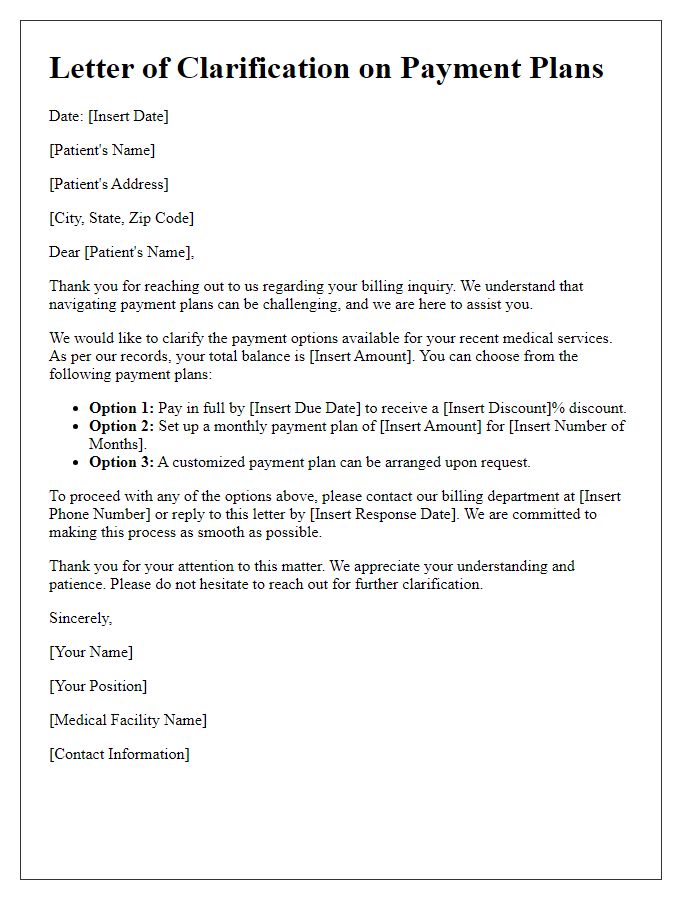
Letter template of clarification on payment plans for patient billing inquiry.
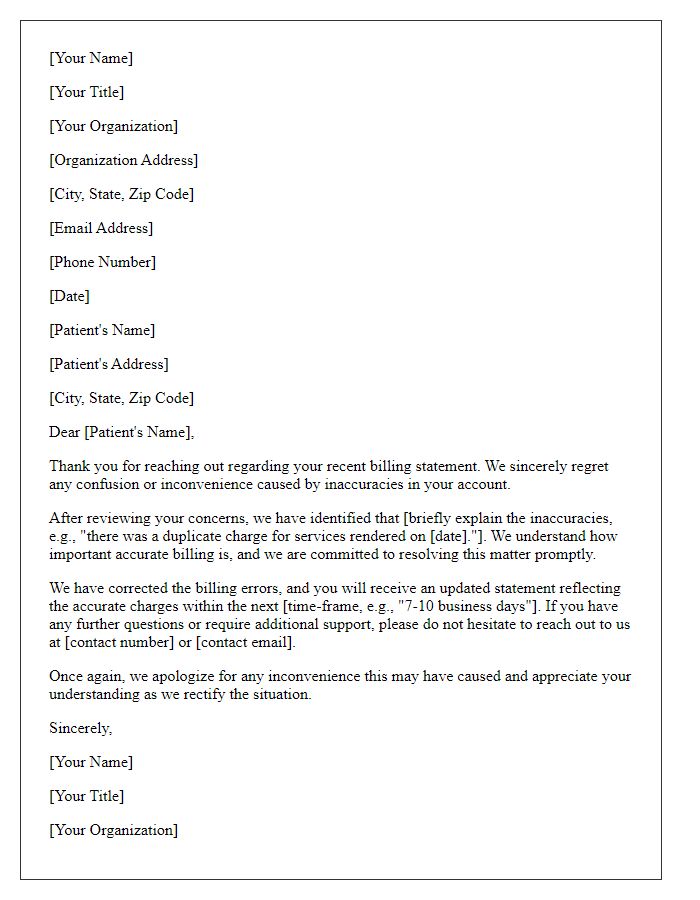
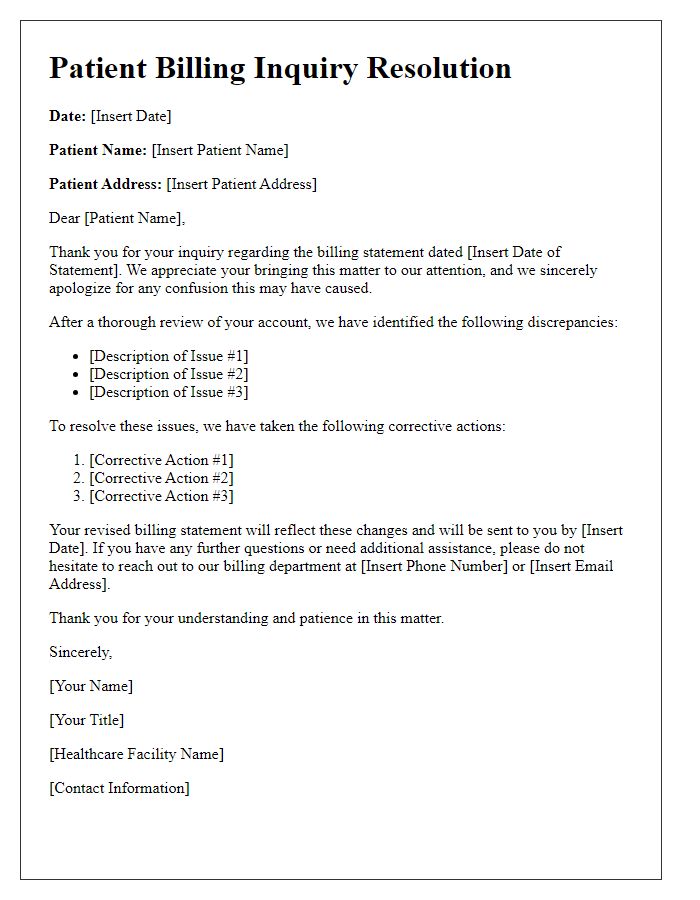
Letter template of regret for billing inaccuracies in response to patient inquiry.
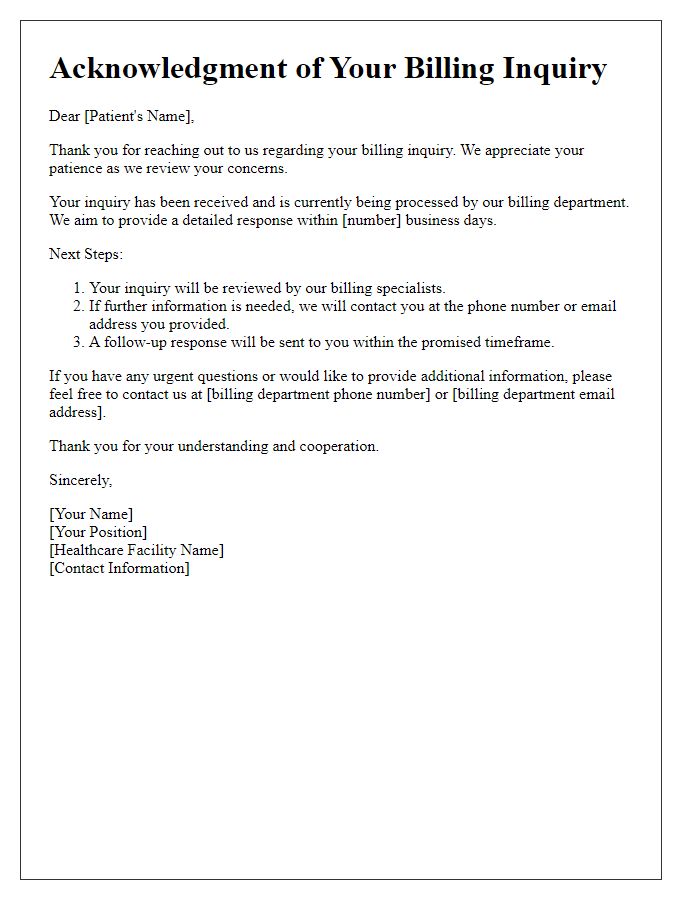
Letter template of acknowledgment of patient billing inquiry and next steps.
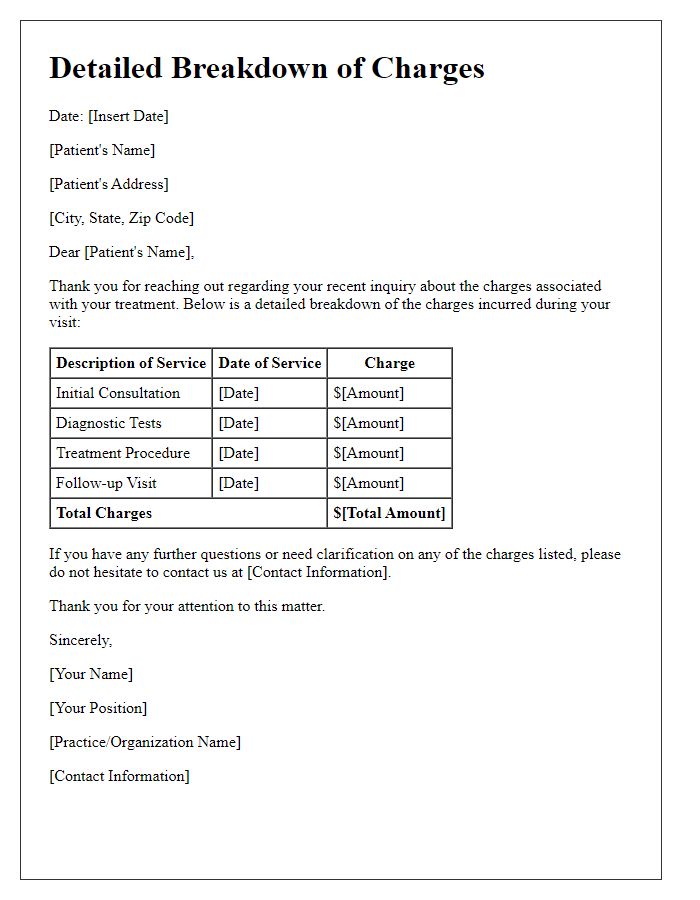
Letter template of detailed breakdown of charges in response to patient inquiry.
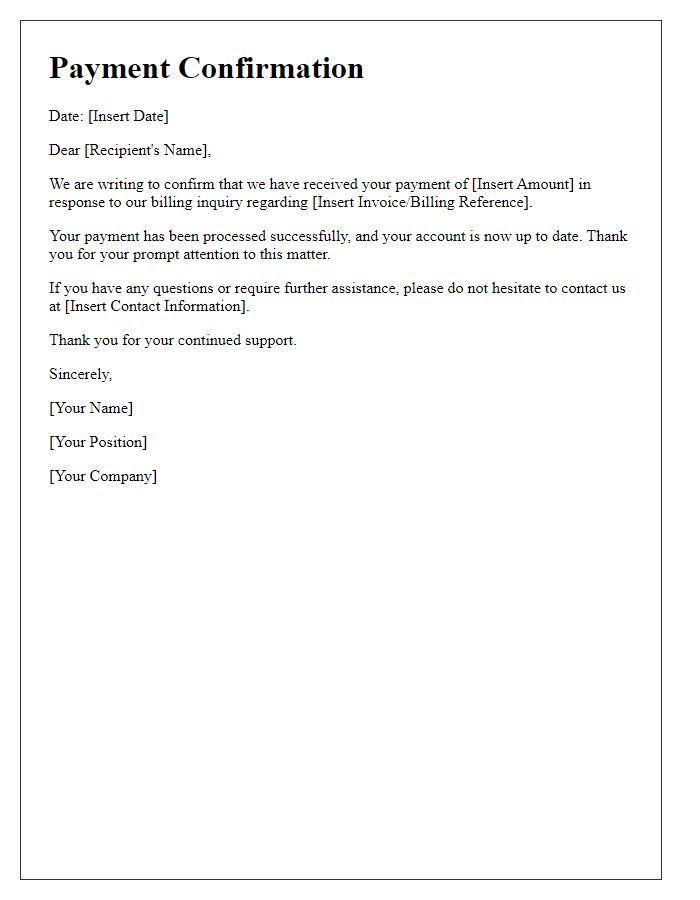
Letter template of confirmation of payment received in response to billing inquiry.


Comments