Are you or someone you know struggling to hear clearly? Hearing loss can significantly affect communication and quality of life, making early evaluations essential for timely intervention. In this article, we'll explore the importance of hearing loss evaluations, what to expect during the process, and how you can seek help. So, let's dive in and discover how to take the first step towards better hearing!
Patient Information
Patient information plays a crucial role in hearing loss evaluations, ensuring that healthcare professionals can provide accurate and personalized assessments. Key details to include are the patient's full name, age (particularly relevance in identifying age-related conditions), contact information, and medical history (including any known ear conditions or previous assessments). Additionally, it is essential to note the specific symptoms reported by the patient, such as difficulty hearing in noisy environments or issues understanding conversations. The patient's occupation can also provide insights into potential exposure to noise, which may contribute to hearing loss. Furthermore, family history of hearing impairment could indicate genetic predispositions to similar conditions. Effective documentation of these factors aids audiologists and ENT specialists in delivering comprehensive and targeted care.
Assessment Findings
Hearing loss evaluations play a crucial role in understanding an individual's auditory capabilities. Comprehensive assessments typically involve various tests, including pure-tone audiometry, which measures the faintest tones a person can hear across different frequencies, often ranging from 250 Hz to 8000 Hz. The findings can reveal degrees of hearing loss categorized as mild (26 to 40 dB), moderate (41 to 55 dB), moderately severe (56 to 70 dB), severe (71 to 90 dB), and profound (91 dB or greater). Speech discrimination scores assess clarity of understanding spoken words, which is vital for communication effectiveness. Additionally, tympanometry evaluates middle ear function by measuring eardrum movement, providing insights into potential conductive hearing issues. These combined results guide audiologists in recommending appropriate interventions like hearing aids, cochlear implants, or auditory rehabilitation strategies.
Medical History
Hearing loss evaluations often begin with a comprehensive medical history, detailing factors that may contribute to auditory impairment. Patients describe their age, with notable prevalence in individuals over 60 years old, and any current medications, including ototoxic drugs like aminoglycosides, commonly used to treat severe infections. Family history may reveal a genetic predisposition indicating the possibility of hereditary hearing loss conditions such as Usher syndrome. Occupation details highlight exposure to noise, particularly in industries like construction or manufacturing, where sound levels exceed 85 decibels over prolonged periods. Additionally, patients report any previous ear injuries or surgeries, such as tympanoplasty, which may affect auditory function. Symptoms assessed include tinnitus, a persistent ringing sensation in the ears, or vertigo, which can indicate underlying vestibular disorders. Ensuring a holistic understanding of these factors sets the foundation for effective hearing loss evaluations and interventions.
Recommendations
Hearing loss evaluations involve various assessments to determine the degree and type of hearing impairment in individuals. Audiometric tests typically measure hearing sensitivity at different frequencies (measured in Hertz), identifying difficulties in understanding speech, particularly in noisy environments. The assessment may also include tympanometry, which evaluates middle ear function, and speech audiometry, which assesses the ability to comprehend spoken words at varying volume levels. These evaluations can help audiologists recommend appropriate interventions, including the use of hearing aids (which can amplify sound) or cochlear implants (surgically implanted devices for severe cases). Regular follow-ups are essential to monitor changes in hearing capacity, along with utilizing assistive listening devices to enhance communication in everyday scenarios.
Follow-Up Instructions
Hearing loss evaluations are critical for determining the degree of auditory impairment, often requiring a comprehensive set of follow-up instructions tailored to patient care. Audiologists recommend scheduling a follow-up appointment within four to six weeks post-evaluation to assess hearing aid fitting, if applicable, or explore other treatment options. Patients should monitor for changes in auditory perception, noting any difficulty in understanding speech, particularly in noisy environments. Keeping a daily log of hearing experiences can provide valuable insight during discussions with healthcare professionals. It is crucial for individuals to safeguard their hearing health by minimizing exposure to loud noises, using protective ear equipment in industrial settings (such as decibel-reducing earmuffs), and maintaining regular check-ups with an audiologist for ongoing monitoring, especially if they work in environments with persistent high-decibel levels.
Letter Template For Hearing Loss Evaluations Samples
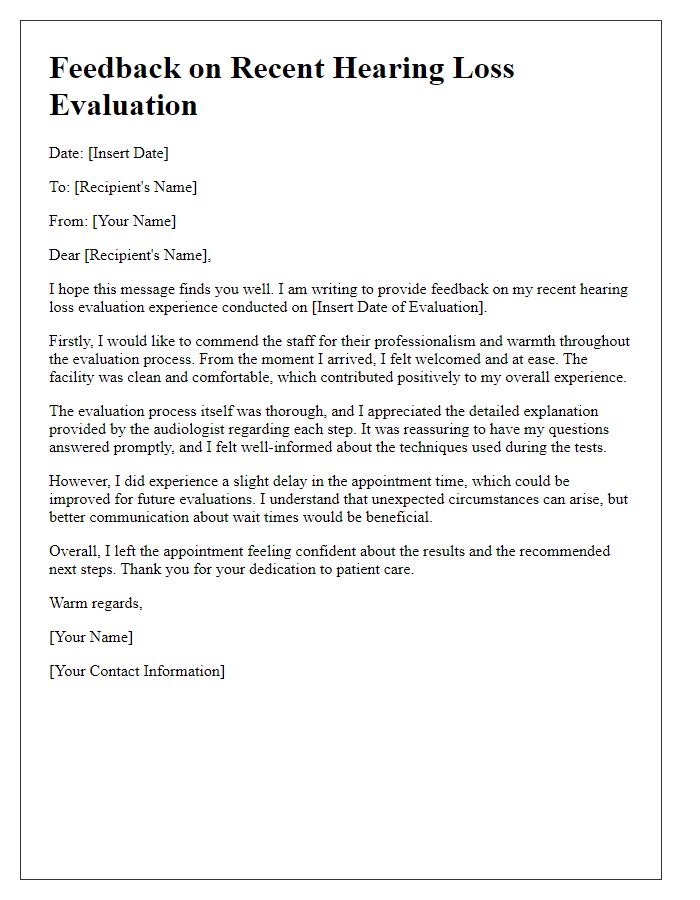
Letter template of feedback on recent hearing loss evaluation experience
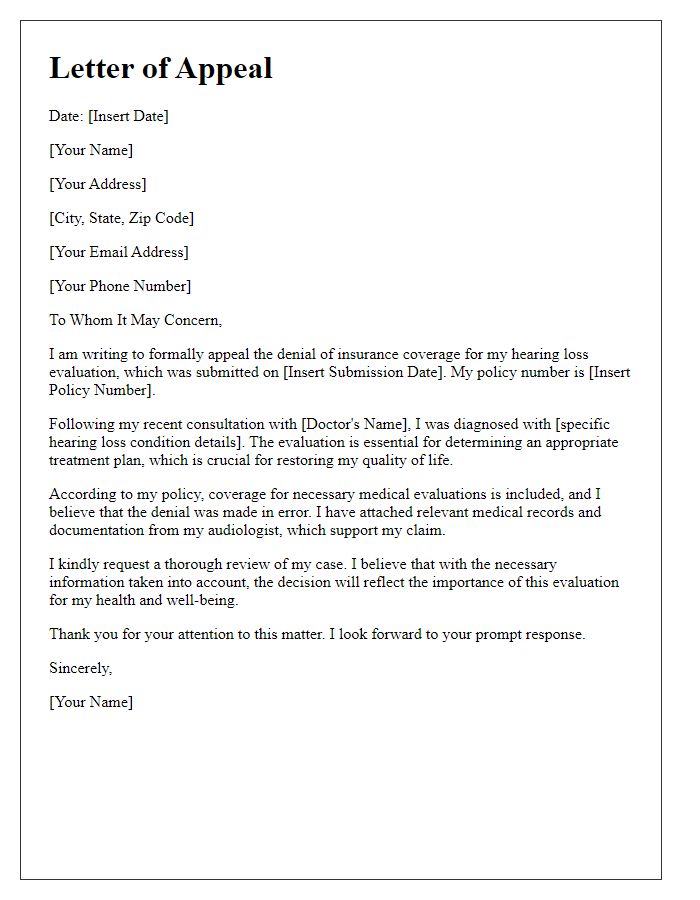
Letter template of appeal for hearing loss evaluation insurance coverage
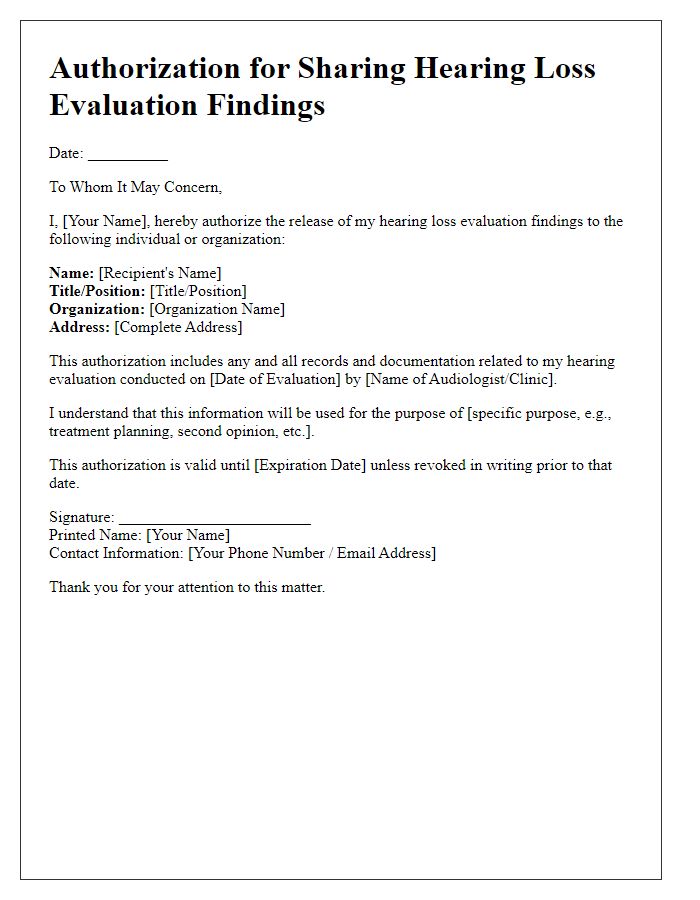
Letter template of authorization for sharing hearing loss evaluation findings


Comments