When it comes to undergoing a surgical procedure, understanding the consent agreement is crucial for both the patient and the medical team. This document not only outlines the specifics of the surgery but also ensures that you are informed about the risks, benefits, and alternatives available to you. Engaging with this process allows you to ask questions and voice any concerns, fostering a collaborative spirit in your healthcare experience. Ready to learn more about the importance of surgical consent? Let's dive in!
Patient Information
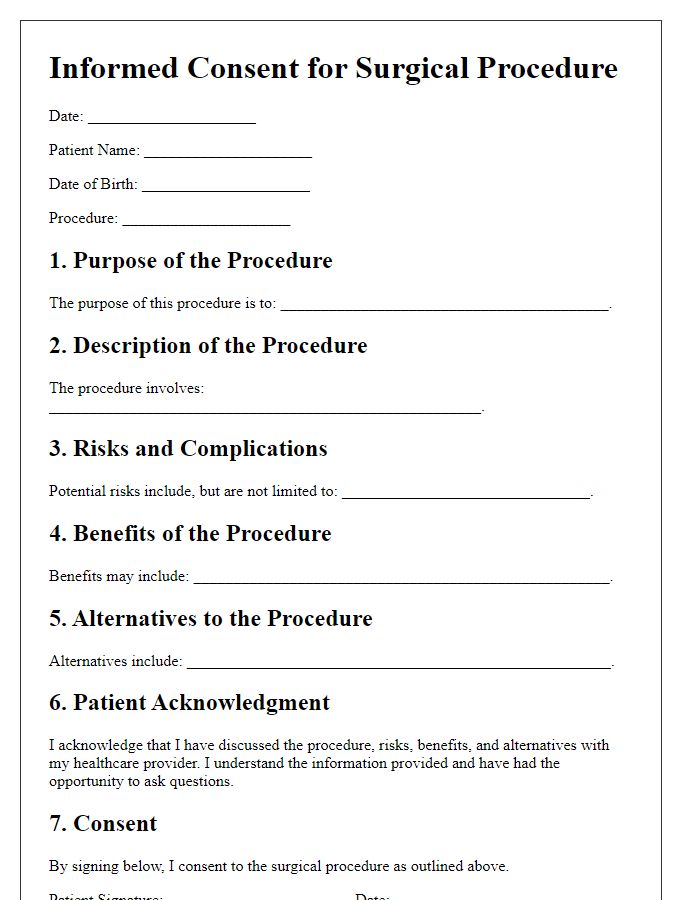
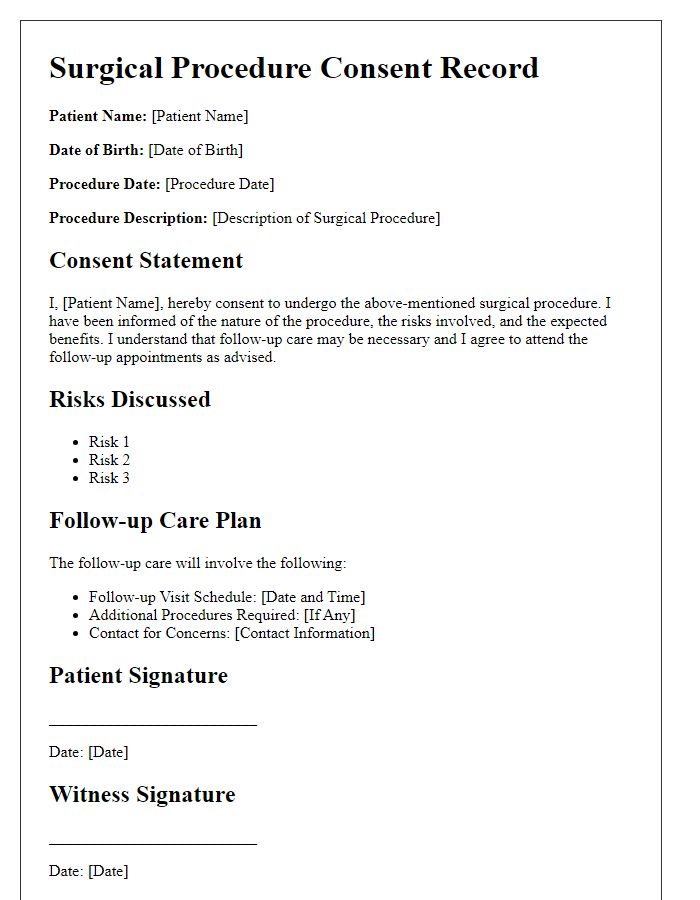
The surgical procedure consent agreement requires detailed patient information, including full name, date of birth (commonly in the format of MM/DD/YYYY), and contact information. Additionally, medical history is crucial, documenting prior surgeries, allergies (such as penicillin or latex), and pre-existing conditions (like diabetes or hypertension). Insurance details should be included, noting the company name and policy number, as well as emergency contact information (name and relationship). Finally, capturing the patient's understanding of the procedure, including risks, benefits, and alternatives, is essential for informed consent, ensuring that the patient is fully aware of the upcoming surgical intervention.
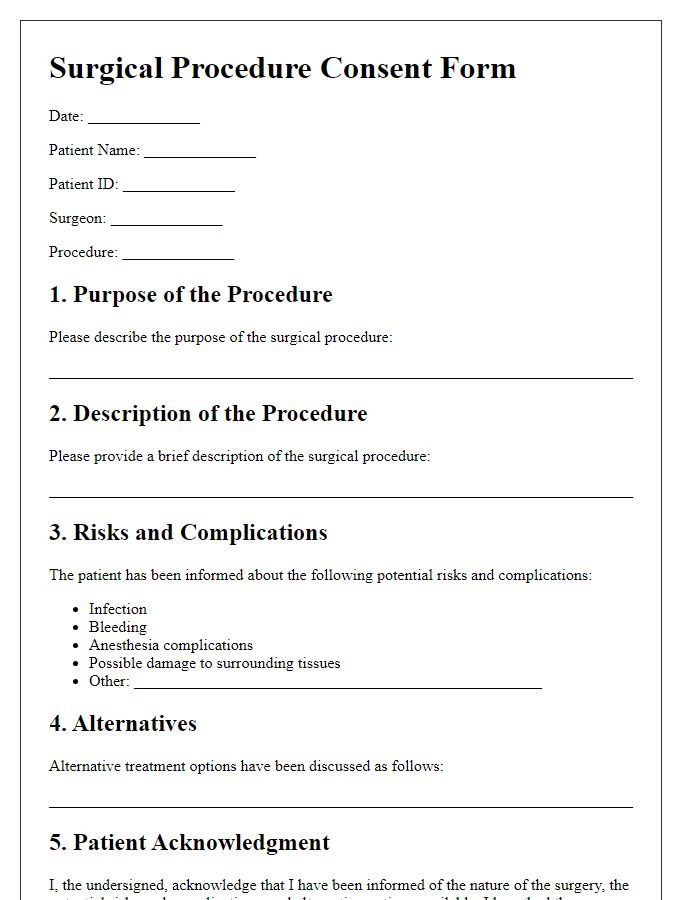
Procedure Description
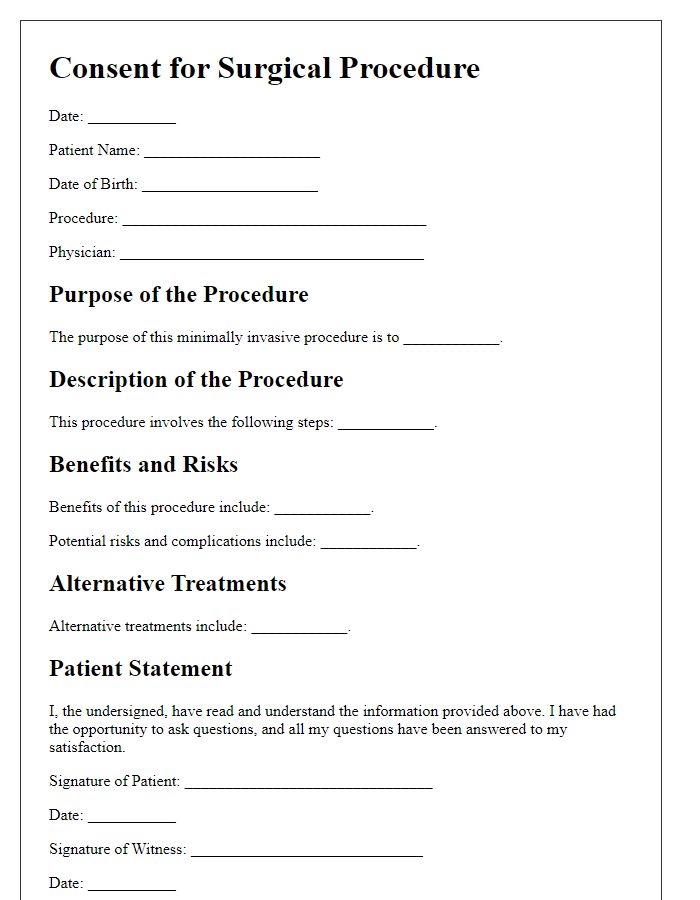
Surgical procedures, such as laparoscopic cholecystectomy, involve the removal of the gallbladder through small incisions in the abdomen, utilizing specialized instruments and a camera. This minimally invasive technique, performed in a hospital setting, typically lasts between one to two hours. Patients undergo preoperative assessments, including blood tests and imaging studies like ultrasound or MRI, to evaluate gallbladder health. Anesthesia may include general anesthesia administered intravenously, where monitoring for vital signs occurs closely throughout the procedure. Postoperative care involves observation in recovery rooms for complications, pain management, and instructions for follow-up appointments. Risks associated with surgery include bleeding, infection, and injuries to surrounding organs such as bile ducts or intestines. Consent is crucial, encompassing understanding of benefits, risks, and alternatives related to the surgical intervention.
Risks and Benefits
Informed consent for surgical procedures requires clear understanding of risks and benefits associated with specific interventions, such as laparoscopic cholecystectomy. Common risks include infection, bleeding, and organ damage, particularly to surrounding structures like the bile ducts. Benefits typically encompass relief from symptoms, such as gallbladder attacks or biliary colic. The procedure can lead to improved quality of life, with many patients experiencing reduced abdominal pain and digestive issues after recovery. For complex surgeries, awareness of potential complications--like anesthesia risks, post-operative complications, or prolonged recovery--remains essential for patient-centered care. Comprehensive discussions of these elements reinforce patient autonomy and safety.
Alternatives and Options
Informed consent for surgical procedures encompasses discussing the various alternatives and options available for patients. For instance, minimally invasive techniques such as laparoscopic surgery versus traditional open surgery present differing recovery times and risks, with minimally invasive approaches typically resulting in shorter hospital stays and reduced post-operative pain. Non-surgical alternatives, such as physical therapy or medication, may also be viable for conditions like hernias or joint surgery, potentially avoiding the need for surgical intervention altogether. Additional options like robotic-assisted surgery have transformed fields such as urology and gynecology, offering increased precision and smaller incisions. Understanding these alternatives empowers patients to make educated decisions about their healthcare journey, weighing the benefits and drawbacks of each method to align with their personal preferences and health goals.
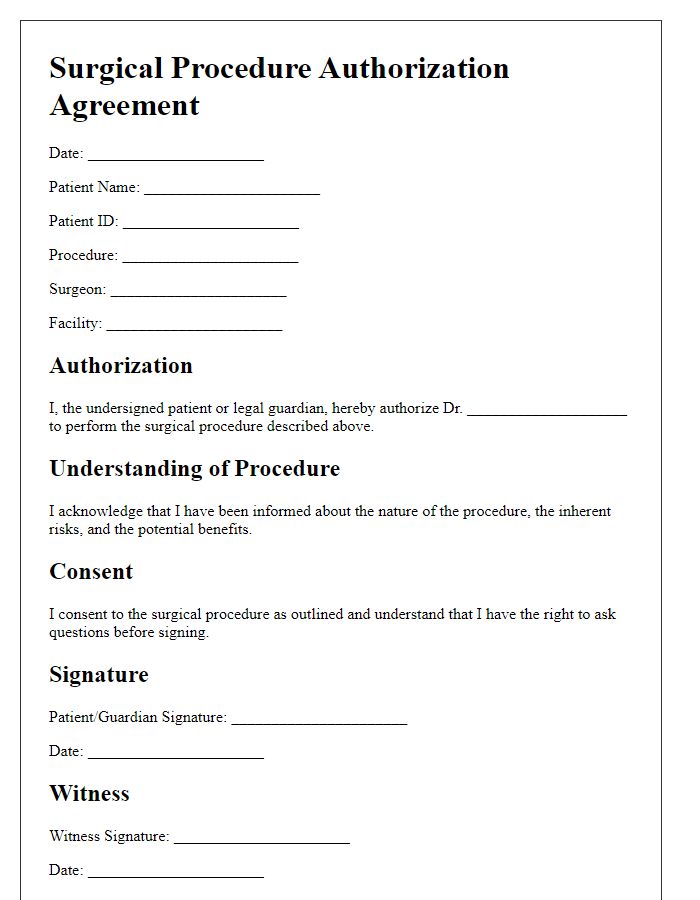
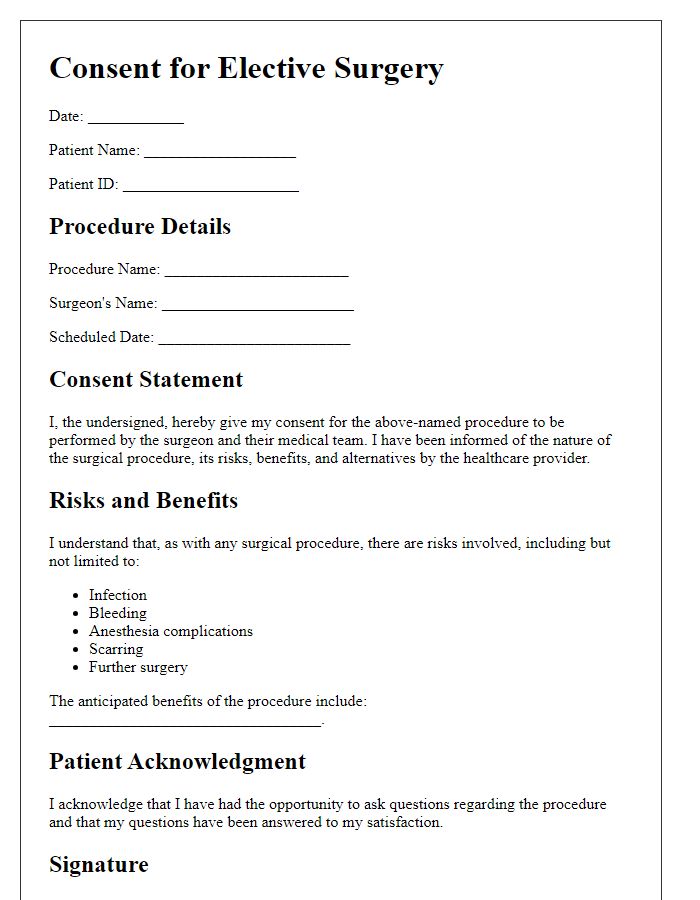
Consent and Authorization Signature
Surgical procedures require explicit consent from the patient to ensure understanding and agreement regarding the intervention. The consent agreement should detail the specific procedure (e.g., laparoscopic appendectomy), associated risks (such as infection or bleeding), and potential benefits (like symptom relief). Patients must be informed about alternatives (e.g., medication, observation) and complications, with emphasis on the importance of preoperative assessments (like blood tests) and postoperative care (including follow-up appointments). The signature section serves as a formal acknowledgment of the patient's understanding and acceptance of the outlined information, empowering them in their healthcare decisions.
Letter Template For Surgical Procedure Consent Agreement Samples
Letter template of surgical procedure informed consent for outpatient procedures
Letter template of surgical procedure authorization agreement for major surgeries
Letter template of surgical procedure consent letter for minimally invasive techniques
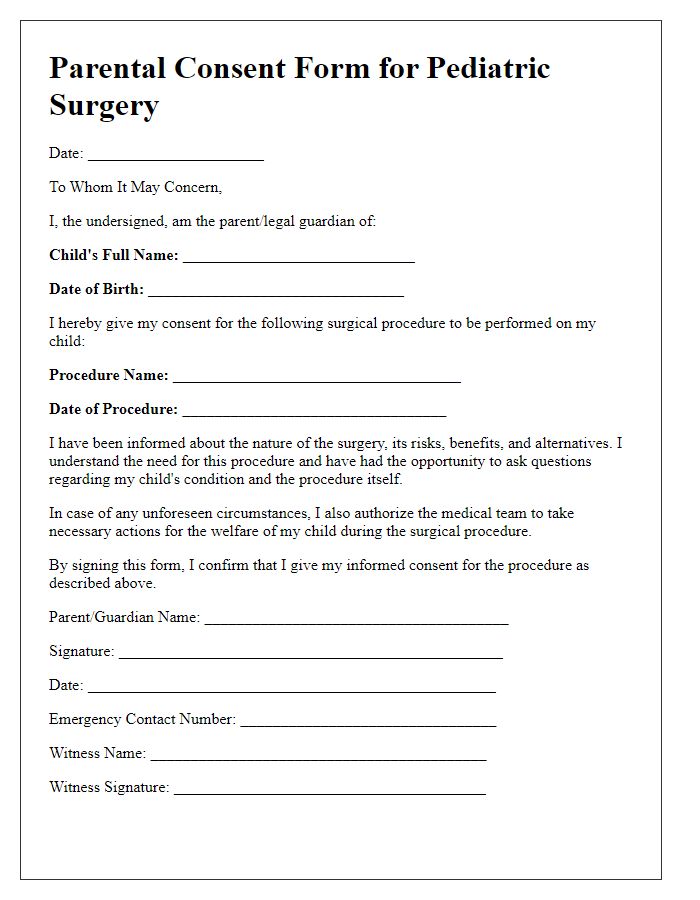
Letter template of surgical procedure parental consent for pediatric surgeries
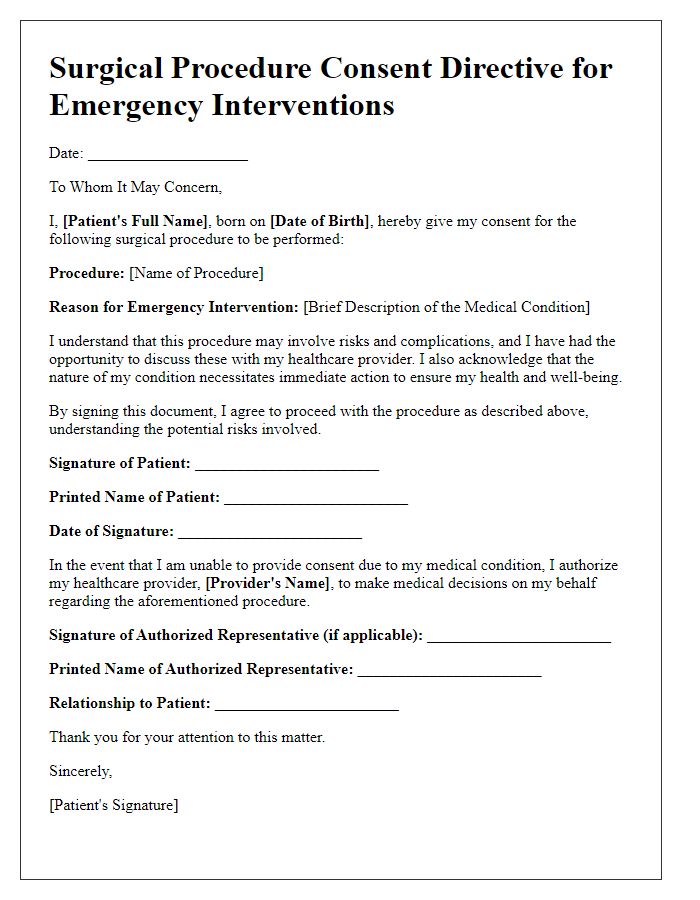
Letter template of surgical procedure consent directive for emergency interventions
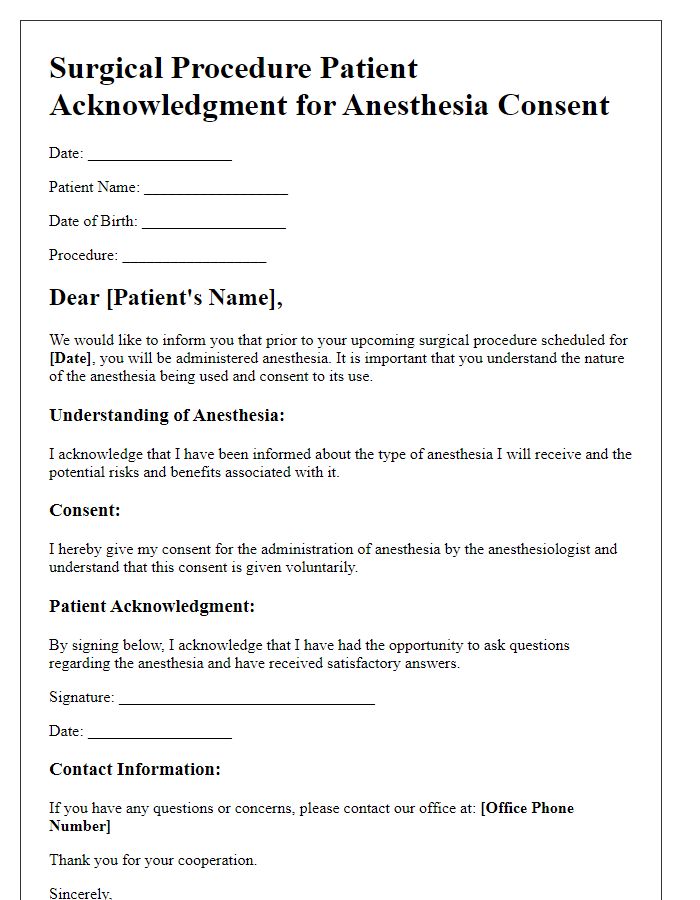
Letter template of surgical procedure patient acknowledgment for anesthesia consent
Letter template of surgical procedure consent documentation for high-risk surgeries
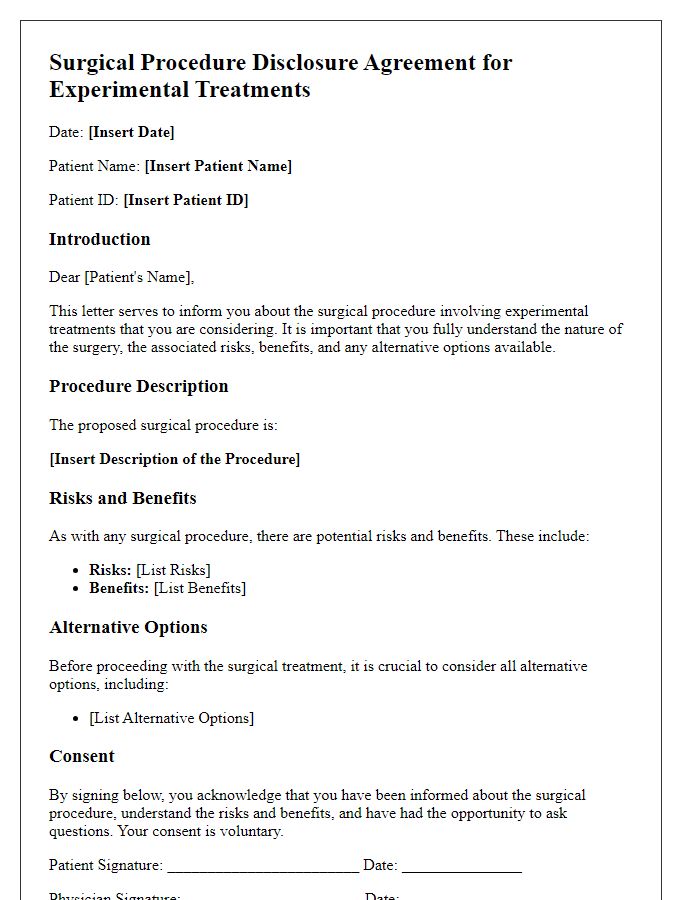
Letter template of surgical procedure disclosure agreement for experimental treatments


Comments