Hey there! If you've ever found yourself needing a clearer picture of clinical documentation standards, you're not alone. Understanding the intricacies of clinical documentation can seem daunting, but it's essential for ensuring quality patient care and accurate billing. In this article, we'll break down the key elements you need to know, making it easier for you to navigate the maze of clinical requirements. So, let's dive in and uncover what you need to enhance your documentation skills!
Patient Information
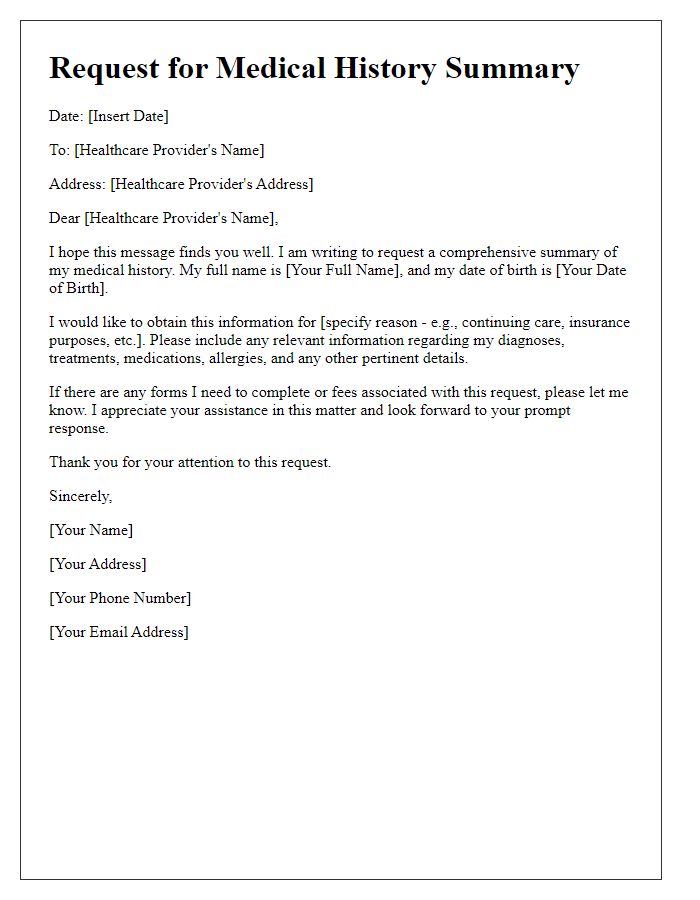
Patient information, including essential health records, personal identification data, and demographic details, serves as a critical foundation for clinical documentation. Details such as full name, date of birth (e.g., January 15, 1985), medical history (including pre-existing conditions like diabetes or hypertension), and contact information (with current address and phone number) assist healthcare providers in delivering effective care. Additionally, insurance details, including provider name and policy number, ensure proper billing and access to coverage for treatment services. Accurate and comprehensive patient information enhances communication and supports decision-making among multidisciplinary healthcare teams, ultimately improving patient outcomes.
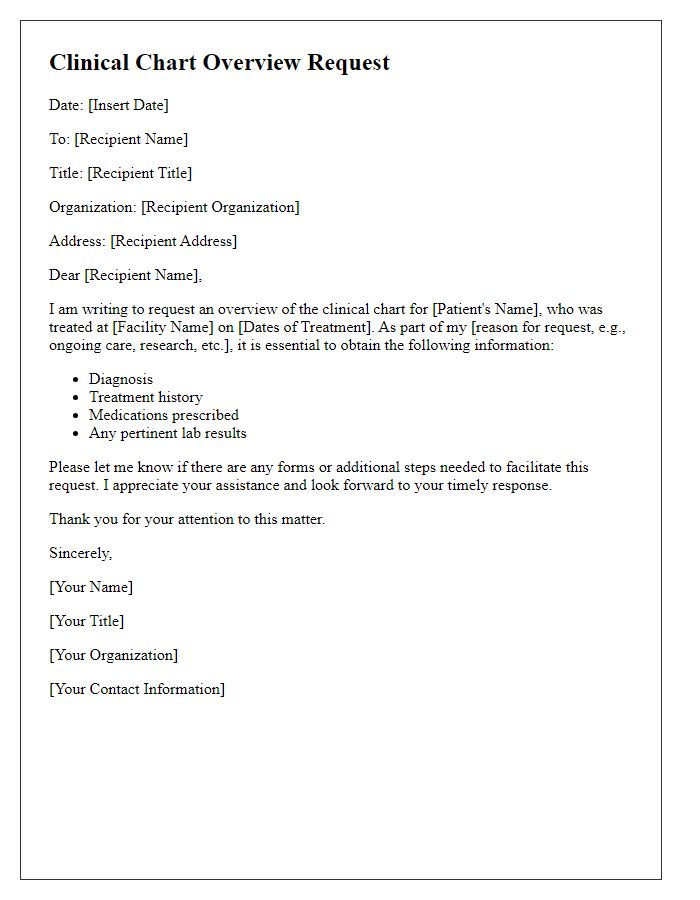
Request Purpose
Clinical documentation overview requests facilitate comprehensive reviews of patient records, ensuring accuracy and completeness. Healthcare providers, such as hospitals or clinics, often seek these overviews to prepare for audits, reviews, or continuous quality improvement initiatives. These requests typically involve accessing specific documents, including patient charts, treatment plans, and progress notes, to evaluate adherence to clinical guidelines. Additionally, thorough documentation reviews can enhance communication among healthcare teams, optimize patient care, and comply with regulatory standards set forth by organizations like the Joint Commission or Centers for Medicare & Medicaid Services.
Specific Documentation Needed
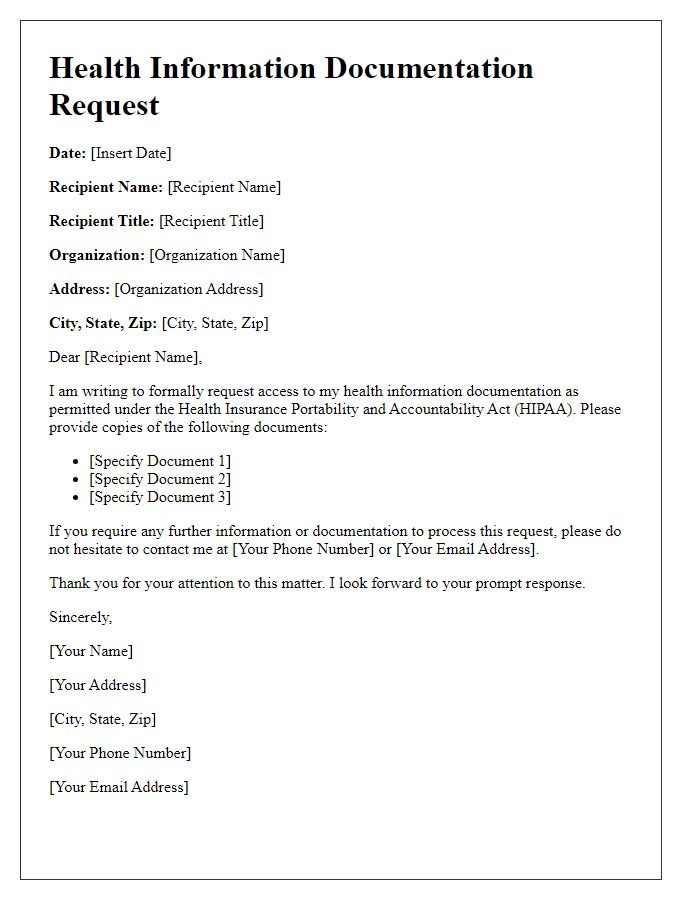
Clinical documentation plays a crucial role in patient care and healthcare management. A comprehensive overview of specific documentation types, including patient medical histories, treatment plans, diagnostic test results, and discharge summaries, is essential for effective communication among healthcare providers. In addition, accurate billing records alongside insurance claims must be included to ensure proper reimbursement. These documents, often housed in electronic health record (EHR) systems, must adhere to regulations set by entities like the Health Insurance Portability and Accountability Act (HIPAA), ensuring patient confidentiality and data security. Each component must be meticulously organized to facilitate seamless access, enabling healthcare professionals to make informed decisions regarding patient safety and treatment efficacy.
Contact Information
Clinical documentation requests typically involve collecting comprehensive data related to patient care within healthcare systems. Essential elements include patient identification (name, date of birth, medical record number), contact details of healthcare providers (names, phone numbers, email addresses), and the specific documents needed (progress notes, discharge summaries, lab results). These records, often kept in electronic health record (EHR) systems, serve as a crucial resource for continuity of care and facilitate communication among medical professionals involved in treatment. Timely and accurate documentation is critical for maintaining high standards of patient safety and ensuring compliance with legal and regulatory requirements in healthcare facilities.
Compliance with Privacy Regulations
Requesting compliance with privacy regulations is crucial for maintaining patient confidentiality and adhering to legal standards in healthcare. The Health Insurance Portability and Accountability Act (HIPAA) mandates strict guidelines for safeguarding protected health information (PHI), ensuring that only authorized personnel access sensitive data. Regular audits and employee training programs help healthcare organizations comply with these federal regulations, reducing the risk of data breaches. In addition, implementing secure electronic health record (EHR) systems and utilizing encryption methods for data transmission provide layers of security crucial for protecting patient information in clinical documentation.


Comments