Creating a chronic disease management plan can be a game-changer for those navigating the complexities of living with a long-term illness. It's essential to have a solid strategy in place to manage symptoms, appointments, and medications effectively. With the right tools and support, individuals can take charge of their health and improve their quality of life. If you're looking for guidance on crafting an effective letter template for a chronic disease management plan, keep reading to discover practical tips and insights!
Patient Information and Medical History
Chronic disease management plans provide essential strategies for ongoing health care, particularly for individuals diagnosed with conditions such as diabetes or hypertension. Patient information includes full name, age, and contact details, necessary for creating tailored care plans. Medical history encompasses existing diseases, past treatments, and medications currently being taken. Notable details might include blood pressure readings (e.g., top number exceeding 140 mmHg) or glucose levels (e.g., average above 200 mg/dL), which help in monitoring progress. Family history can also be important; for example, a family history of cardiovascular disease can necessitate proactive measures. Regular assessments of weight, laboratory results, and lifestyle habits like exercise frequency are crucial for effective management. Each element helps healthcare providers create personalized and effective chronic disease management strategies.
Diagnosis and Current Status
Chronic disease management plans are essential for individuals diagnosed with long-term health conditions such as diabetes, hypertension, or heart disease. These plans often include personalized strategies aimed at addressing various aspects of daily health management. For instance, individuals with diabetes may require blood sugar monitoring several times a day, with optimal target levels typically between 80 to 130 mg/dL before meals. Moreover, medications, such as Metformin for Type 2 diabetes, must be adhered to as prescribed, with regular consultations scheduled every three months to assess progress. In addition, lifestyle modifications, including a balanced diet rich in whole grains and lean proteins and at least 150 minutes of physical activity weekly, play a crucial role in managing symptoms and preventing complications. Regular follow-ups not only monitor the current status of the chronic condition but also support mental well-being, acknowledging the emotional burden of living with a chronic illness.
Treatment Goals and Objectives
Chronic disease management plans emphasize specific treatment goals and objectives essential for effective patient care. Clear target metrics, such as blood pressure levels below 130/80 mmHg for hypertension, guide therapeutic interventions. Weight management, aiming for a body mass index (BMI) of 25 or less, supports overall health improvements. Regular blood glucose monitoring targets maintaining levels between 70-130 mg/dL for diabetes management, enhancing long-term health outcomes. Collaboration with healthcare providers, including endocrinologists, dietitians, and primary care physicians, ensures comprehensive care tailored to individual needs. Scheduled follow-up appointments, typically every three months, facilitate ongoing assessment and adjustment of treatment strategies. Patient education on lifestyle modifications, such as dietary changes adhering to the DASH diet, plays a crucial role in attaining these objectives. Engaging support systems, like diabetes support groups or hypertension awareness programs, can provide encouragement and accountability, fostering adherence to the management plan.
Medication and Therapies
Chronic disease management plans must emphasize effective medication and therapies tailored to individual needs. Medications such as Metformin for Type 2 Diabetes, prescribed at a standard dosage of 500 mg, aim to regulate blood sugar levels. Additionally, Statins like Atorvastatin can manage cholesterol, often administered at 20 mg daily to reduce cardiovascular risk. Patient education is crucial; for instance, understanding potential side effects, including nausea or muscle pain, enhances adherence. Furthermore, therapies such as Cognitive Behavioral Therapy (CBT) can assist individuals dealing with the psychological impact of chronic diseases, providing tools for stress management and coping strategies. Regular follow-ups are essential to monitor progress, adjust medications, and ensure optimal patient outcomes in locations such as outpatient clinics or telehealth platforms.
Follow-up and Review Schedule
A chronic disease management plan focuses on the systematic approach to care for long-term health conditions, such as diabetes, heart disease, and arthritis. Regular follow-up appointments, scheduled every three months, are essential to monitor patient progress and adjust treatments as necessary. Each review session should include assessments of key health indicators, including blood pressure readings (ideally below 130/80 mmHg for optimal heart health) and blood sugar levels (usually targeted around 70-130 mg/dL for diabetics). Patients will also receive lifestyle modification support, such as nutritional counseling based on the Dietary Guidelines for Americans (2020-2025) and recommended physical activity levels (150 minutes of moderate exercise weekly). Additionally, educational resources regarding medication adherence and symptom tracking will be provided. Establishing a structured communication plan between healthcare providers and patients promotes adherence, enhances understanding of disease management, and ultimately improves health outcomes.
Letter Template For Chronic Disease Management Plan Samples
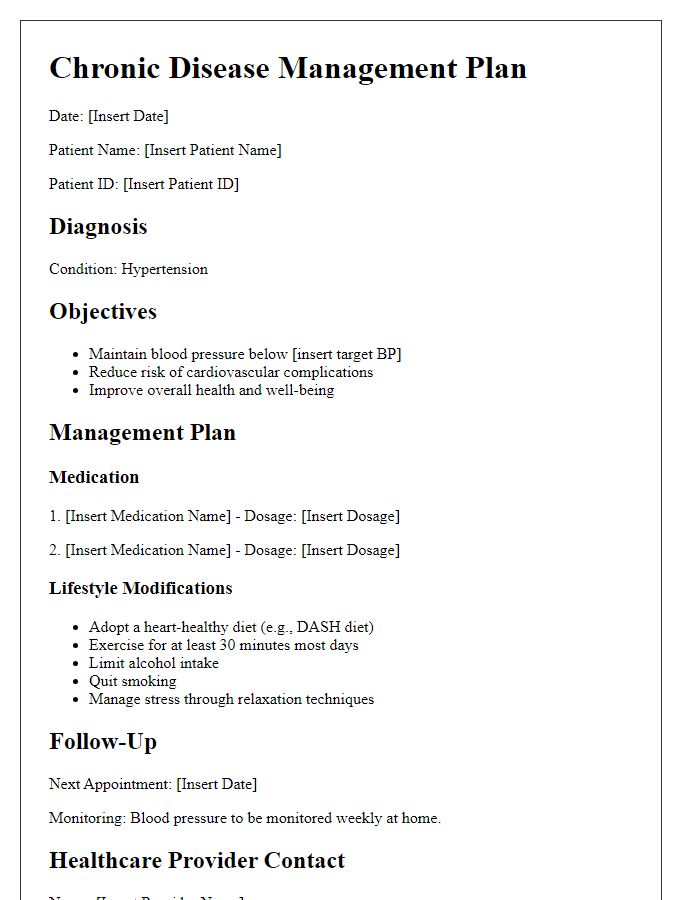
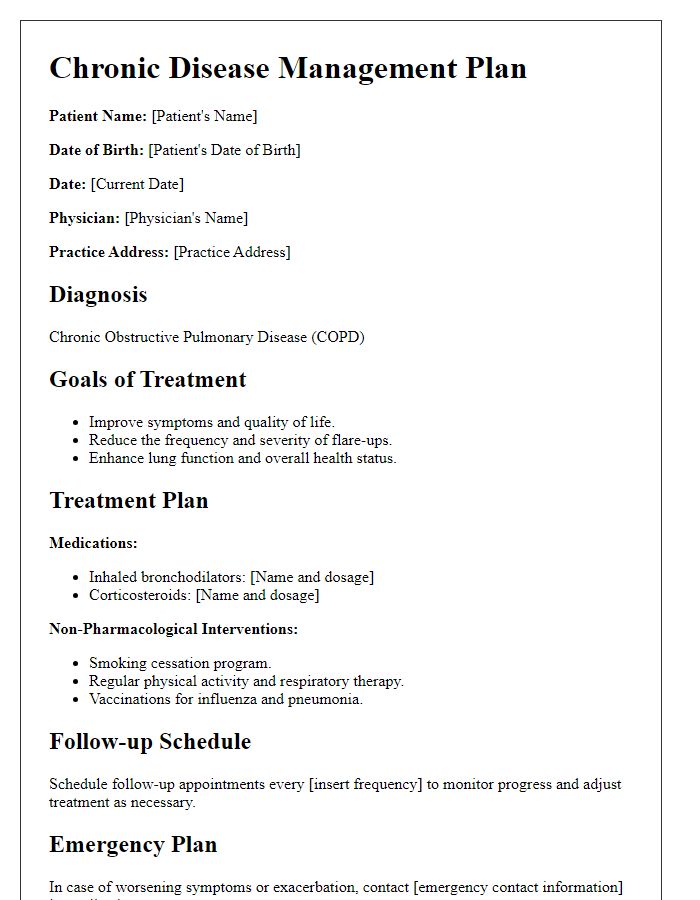
Letter template of Chronic Disease Management Plan for Hypertension Management
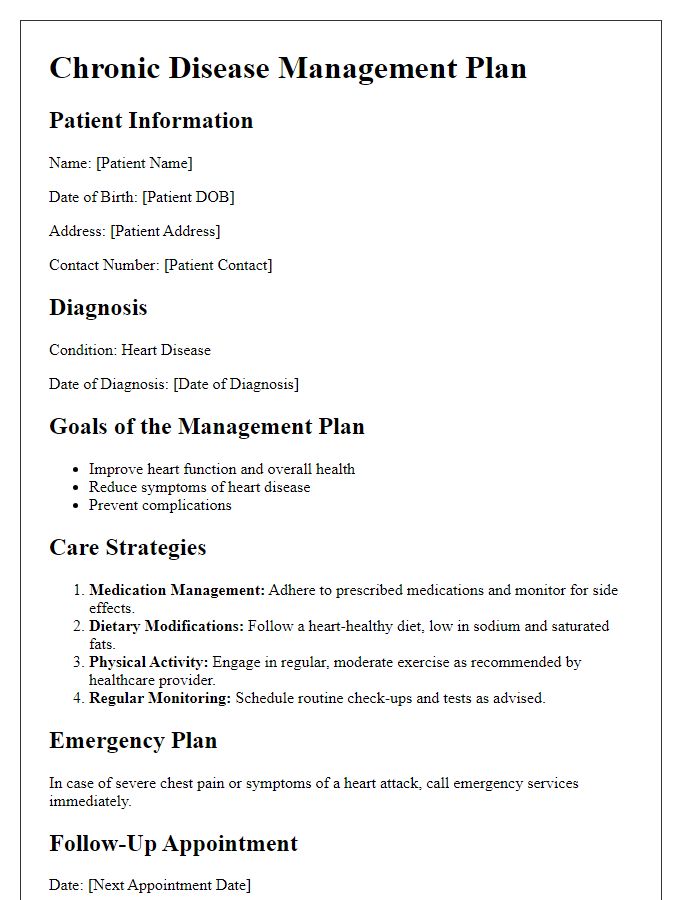
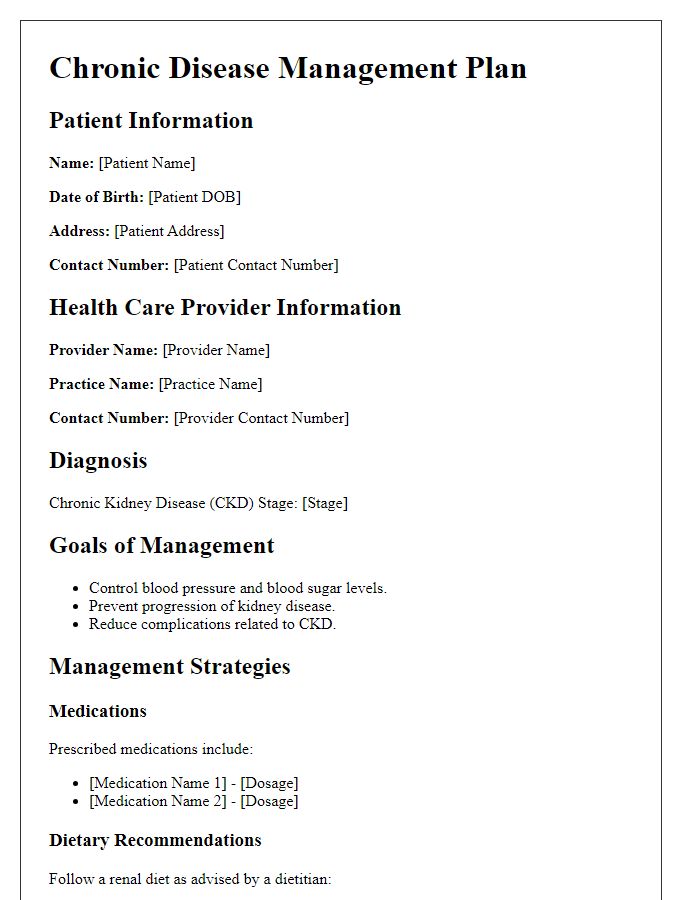
Letter template of Chronic Disease Management Plan for Heart Disease Management
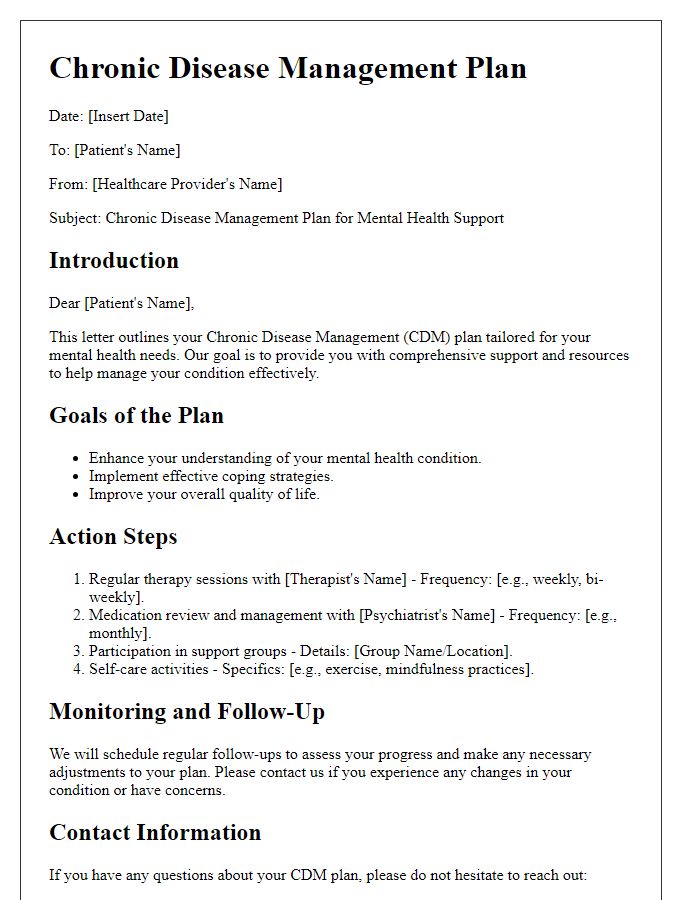
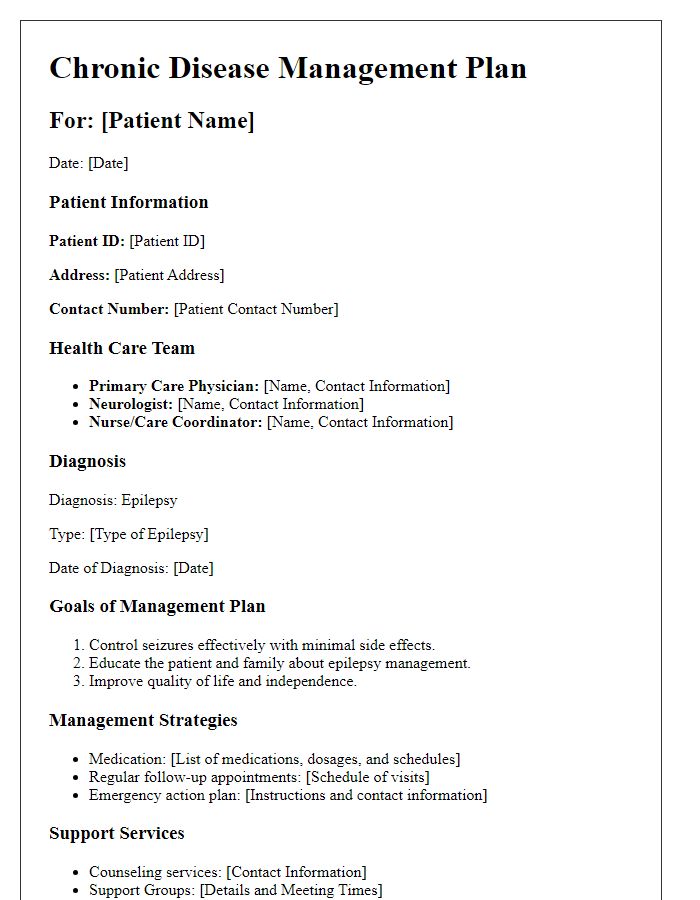
Letter template of Chronic Disease Management Plan for Mental Health Support
Letter template of Chronic Disease Management Plan for Obesity Management


Comments