When it comes to planning for hospice care, having a clear and compassionate letter can make all the difference for families faced with difficult decisions. This guide will walk you through creating a heartfelt template that addresses the needs and wishes of your loved one while considering their comfort and dignity. By personalizing key elements, you can ensure that your message resonates with caregivers and family members alike. Ready to explore how to craft the perfect hospice care planning letter? Let's dive in!
Personal information and identifiers
In hospice care planning, personal information and identifiers are crucial for ensuring tailored support and effective communication. Key elements include the patient's full name, date of birth (essential for age-related considerations), and identification numbers (such as Medicare or Medicaid identifiers that facilitate access to services). Documentation should also encompass the primary caregiver's contact information and relationships with the patient, vital for coordinating care and support. Furthermore, it is important to include the patient's address, which is significant for home care arrangements, and any advance directives or healthcare proxies, which outline the patient's wishes regarding medical treatment. Identifiers ensure that all team members involved in the hospice care process have access to accurate, confidential information essential for delivering comprehensive and compassionate care.
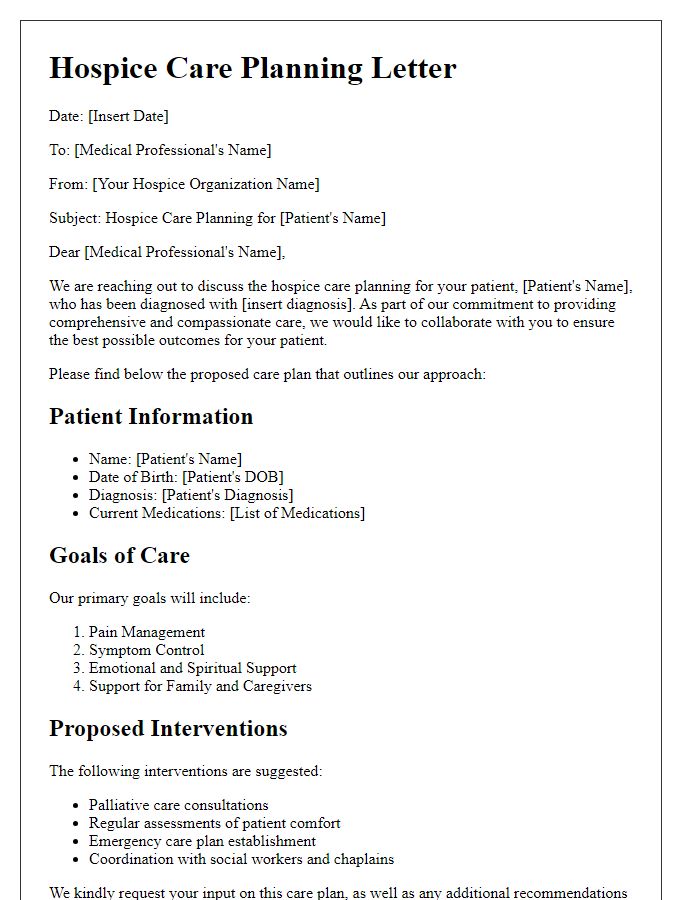
Patient's medical history and current condition
A comprehensive review of a patient's medical history is essential in hospice care planning, especially for individuals with terminal illnesses like metastatic cancer or advanced heart failure. The patient's previous diagnoses should include significant health events, such as surgeries (for instance, a coronary artery bypass graft in 2019) and hospitalizations (like a recent stay for pneumonia in June 2023). Current conditions, such as pain levels (rated at 8 out of 10), mobility restrictions (requiring assistance with activities of daily living), and psychological factors (like depression or anxiety related to end-of-life transitions), significantly influence the care approach. Furthermore, understanding medications, including their dosages and side effects, plays a critical role in pain management and overall patient comfort, while noting any allergies is crucial for preventing adverse reactions. Regular assessments by a multidisciplinary team can enhance personalized care plans tailored to the patient's needs and family preferences.
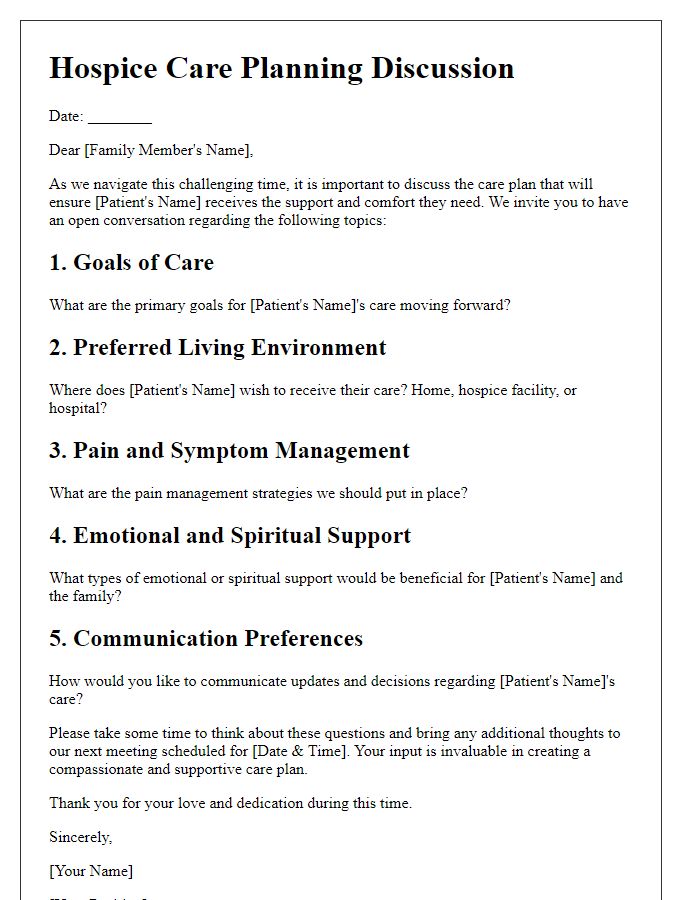
Care preferences and goals
Hospice care planning focuses on individualized care preferences and goals for patients nearing the end of life. Essential components include establishing comfort measures tailored to patient needs, such as pain management protocols that prioritize medications like opioids (e.g., Morphine), emotional support systems involving counselors or chaplains, and creating personalized care plans that reflect patient wishes regarding life-sustaining treatments. Advanced directives, such as Do Not Resuscitate (DNR) orders, are critical for ensuring that patients' end-of-life choices are honored. Family involvement is vital, allowing loved ones to express their concerns and help facilitate discussions with healthcare providers about desired care environments, whether at home or in specialized facilities like hospice centers, ensuring a supportive atmosphere during final moments.
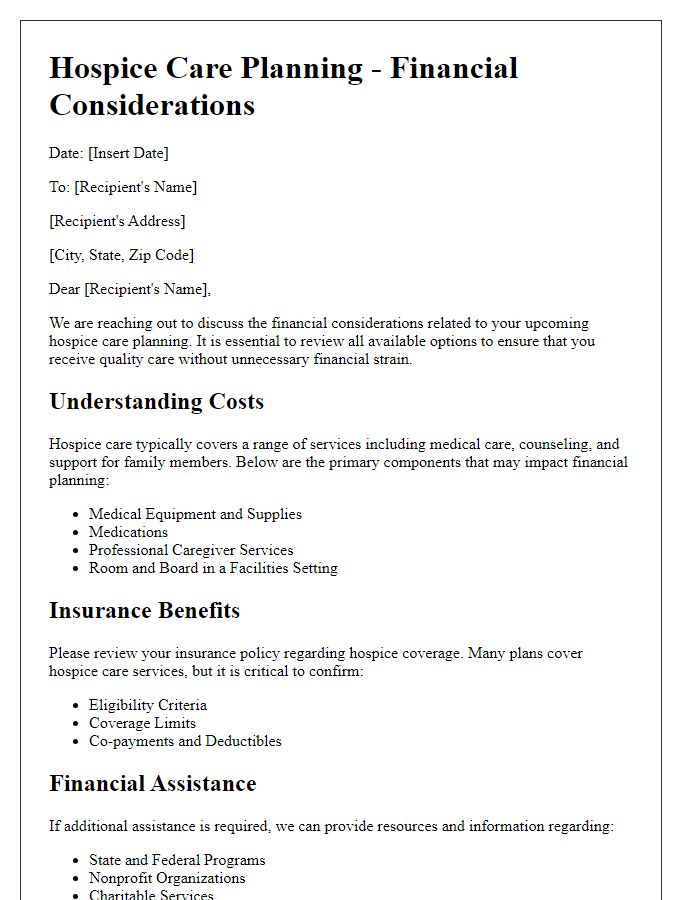
Legal and financial considerations
Hospice care planning requires careful attention to legal and financial factors to ensure patients receive appropriate end-of-life care while minimizing family burdens. Advance directives are critical documents, such as Living Wills and Durable Powers of Attorney, which outline a patient's healthcare preferences and designate an individual to make healthcare decisions when the patient is unable. This ensures that medical professionals at facilities like Hospice of the Valley in Arizona can follow the patient's wishes accurately. Financial considerations include reviewing costs associated with hospice services, which may vary across different providers and states, understanding insurance coverage, Medicare benefits, and potential out-of-pocket expenses to alleviate the financial strain on families. Additionally, establishing a trust or designating beneficiaries can help manage financial assets effectively, ensuring funds are available for the patient's care throughout the hospice journey.
Contacts and communication plan
Hospice care planning requires a structured communication plan to ensure the coordination of services among healthcare providers, family members, and patients. Key contacts in this plan typically include the primary care physician, hospice nurse, social worker, and family caregivers. The primary care physician oversees medical treatment and can offer insights into the patient's condition, while the hospice nurse provides day-to-day care and symptom management. Social workers facilitate emotional support and practical assistance, such as arranging for respite care or counseling services for the family. Clear guidelines for communication methods, including scheduled meetings, phone calls, or emails, ensure that everyone involved is informed about the patient's status and changes in care preferences. Regular updates and documentation also help maintain continuity of care, improving overall patient experience and supporting families during difficult times.


Comments