Navigating the world of healthcare billing can often feel overwhelming, especially when discrepancies arise. It's crucial to address these issues promptly to ensure that your financial responsibilities are accurately reflected. In this article, we'll outline an effective letter template designed for disputing healthcare billing errors and help you advocate for your rights as a patient. Stay with us as we provide tips and insights to empower you in resolving your billing disputes successfully!

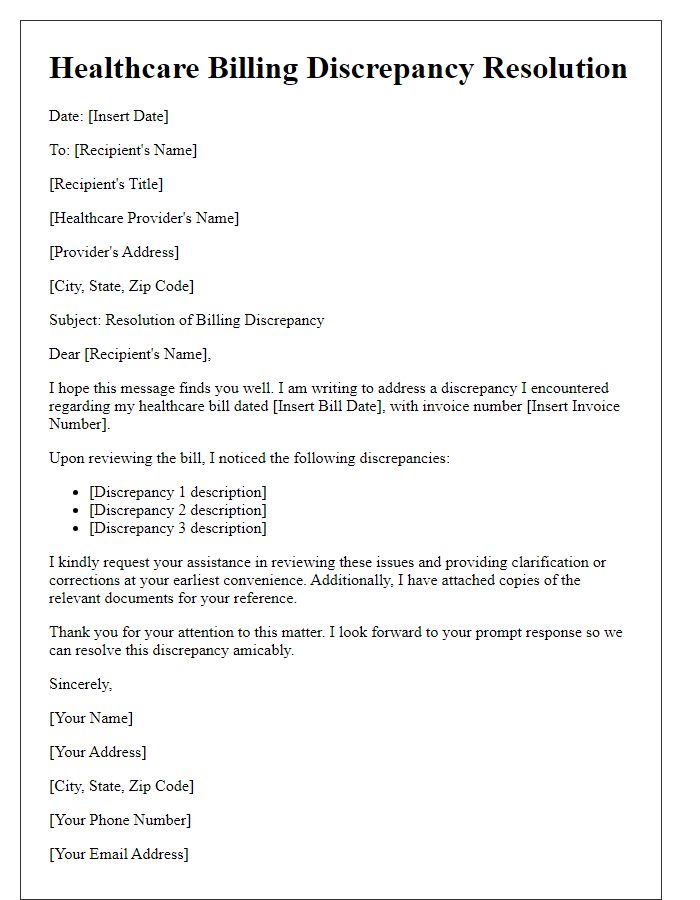
Patient Information and Account Details
Healthcare billing disputes often arise due to discrepancies between services billed and services received, impacting patient accounts. Critical details include patient information (name, date of birth, insurance policy number), account details (account number, statement date), and service dates (specific medical appointments or treatments). Clear description of the disputed charges is essential, often referencing CPT codes (Current Procedural Terminology) linked to specific medical services. Documentation should support the claim, including medical records, EOB (Explanation of Benefits) from insurers, and notes from healthcare providers. Timely resolution is crucial, as delay can affect credit ratings and prompt payment requirements.
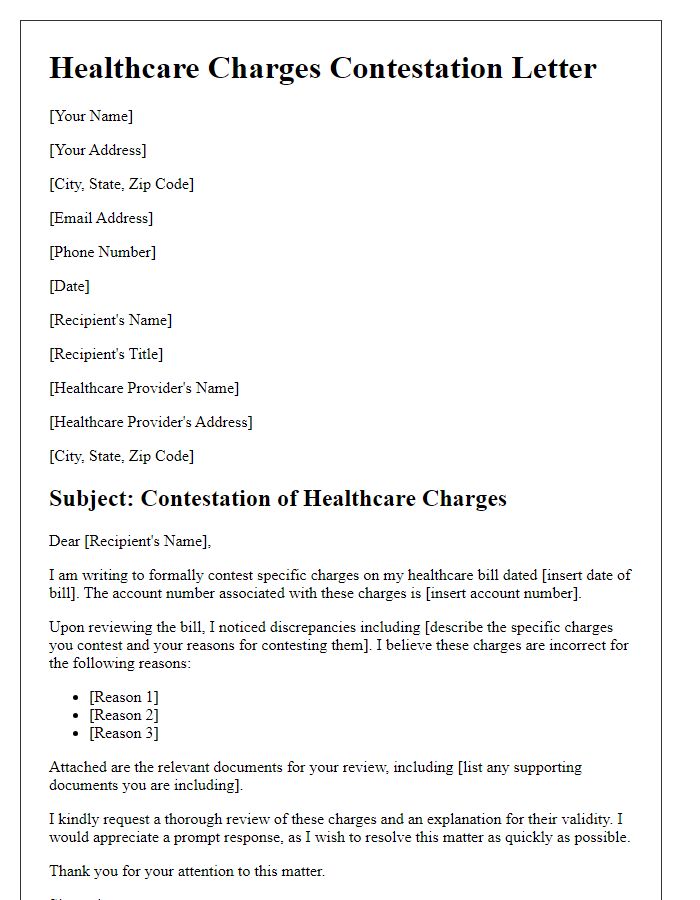
Disputed Charges with Specific Codes
Disputed healthcare charges can lead to confusion and frustration among patients. Medical Billing Codes, such as CPT (Current Procedural Terminology) or ICD (International Classification of Diseases), play a critical role in categorizing services and determining costs. An example includes CPT Code 99213, typically used for an established patient office visit, which may be contested if the billed service does not match the provided care level. Charge discrepancies might arise for specific services, such as lab tests, surgical procedures, or imaging. The process for resolving these disputes often includes submitting a formal billing dispute letter to the provider or billing department, referencing specific dates of service, description of services, and the associated codes in question, supported by relevant documentation such as EOB (Explanation of Benefits) statements or medical records. Timely follow-ups with the insurance company or healthcare provider can facilitate quicker resolutions.
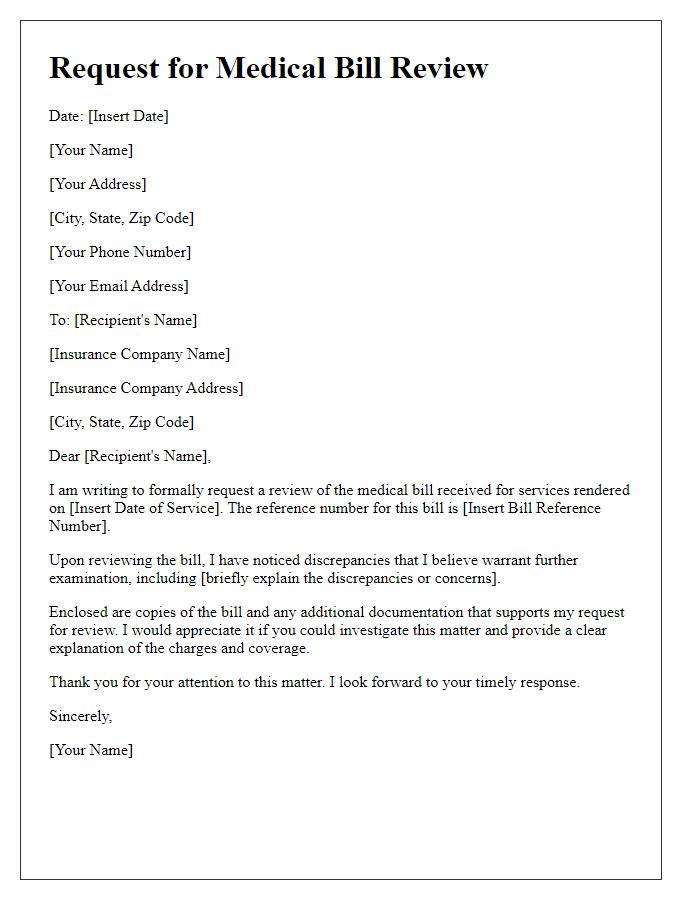
Clear Explanation of Discrepancy
Healthcare billing discrepancies often occur due to incorrect coding, coverage issues, or unexpected charges. For instance, a patient receiving treatment for a sprained ankle at a facility like Mercy Hospital (notably recognized for orthopedic care) might encounter a billing issue where the charge for an X-ray is labeled as "out-of-network," despite the hospital being an in-network provider. This can lead to confusion regarding the copayment amount and balance due. Additionally, the explanation of benefits (EOB) from the insurance company, such as Blue Cross Blue Shield, may reflect an incorrect procedure code, resulting in a denial of coverage for essential services. Such discrepancies demand clear documentation, including itemized bills and EOB statements, to facilitate effective dispute resolution.
Supporting Documentation
Healthcare billing disputes often arise from discrepancies in charges or misunderstandings regarding services rendered. Comprehensive supporting documentation is essential for resolution. Important items include the initial medical bill dated March 15, 2023, which outlines specific charges for services at Springdale Hospital, a facility known for its emergency care. Items like explanation of benefits (EOB) received from Acme Health Insurance, correlating to the same date, detail payment responsibilities and adjustments. Additionally, copies of medical records from Dr. John Smith, the attending physician, demonstrate the necessity of services provided. Clear documentation ensures that all parties have access to accurate information, facilitating an efficient resolution process.
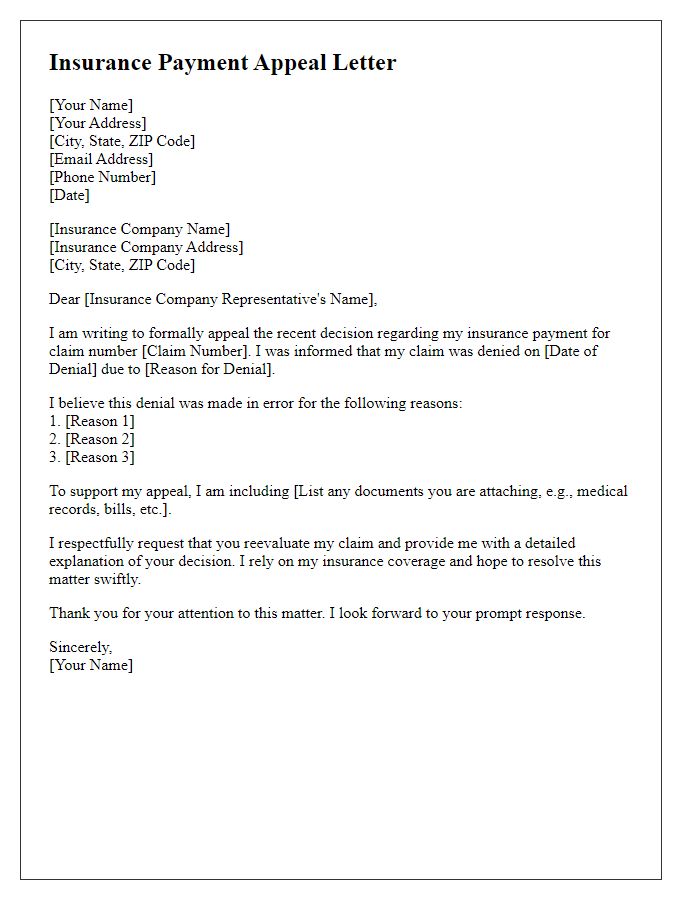
Contact Information for Follow-Up
Effective communication plays a vital role in healthcare billing dispute resolution. Important contact information includes names of dedicated billing representatives, phone numbers, and email addresses for prompt follow-up. Often, healthcare facilities such as hospitals or outpatient centers provide a specific billing department hotline (for example, 1-800-555-0199) for resolving disputes. It is essential to keep a record of correspondence, including dates and times of phone calls, and visit documentation related to the billing question. Referencing specific dates of service (e.g., January 15, 2023) and account numbers enhances clarity in ongoing discussions. Timely follow-up is crucial to ensuring that disputes are addressed satisfactorily within the billing cycle.



Comments