Are you feeling overwhelmed by the insurance pre-authorization process? You're not alone! Many individuals struggle with getting their necessary treatments approved, leading to frustration and confusion. In this article, we'll guide you through an effective appeal letter template that can help you navigate the hurdles of insurance approvals and advocate for your health needsâread on to learn more!
Clear Patient and Policy Information
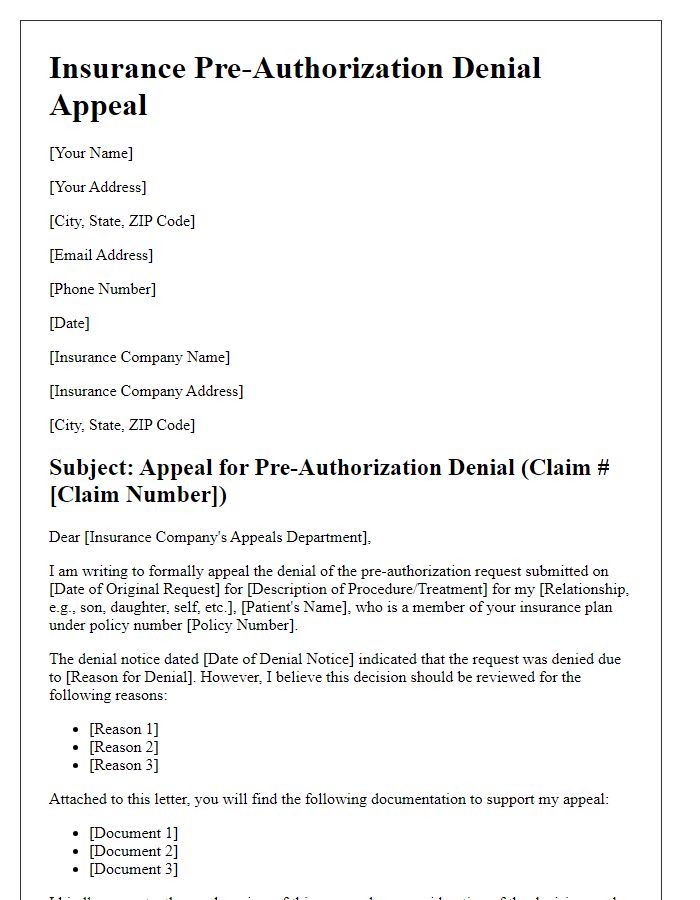
Clear patient information includes details such as the patient's full name, date of birth, and insurance policy number. Essential policy information features the insurance company's name, claim number, and relevant coverage details. Accurate documentation ensures that all necessary elements for the pre-authorization appeal are included, facilitating the review process. Specifically, including the correct patient address, policy expiration date, and diagnosis codes can significantly enhance clarity. Such meticulousness aids in swift processing by insurance adjusters, reducing turnaround times on appeals. Thoroughly addressing these details maximizes the chances of a successful pre-authorization outcome, particularly in complex cases requiring urgent medical services.
Detailed Medical Necessity Explanation
Insurance pre-authorization appeals often require a thorough explanation of medical necessity for the requested treatment or procedure. In cases such as a knee replacement surgery, the patient typically suffers from osteoarthritis, a degenerative joint condition affecting approximately 27 million Americans, leading to chronic pain and decreased mobility. Comprehensive evaluations, including MRI scans or X-rays, may reveal significant cartilage loss, impacting function and quality of life. Guidelines from the American Academy of Orthopaedic Surgeons suggest surgical intervention when conservative treatments, such as physical therapy or steroid injections, have failed after six months. Moreover, favorable outcomes demonstrated in large-scale studies indicate that over 90% of patients experience substantial pain relief and improved joint function post-surgery. Additionally, potential complications of delaying necessary surgery, such as muscle atrophy or further degradation of joint health, reinforce the urgency for timely intervention. These documented factors establish the imperative nature of the pre-authorization request, emphasizing the procedure's alignment with established medical protocols and appropriateness for the patient's health condition.
Relevant Medical Records and Documentation
Insurance pre-authorization appeals require thorough documentation to support claims for specific medical treatments. Medical records, including detailed assessments from healthcare providers such as primary care physicians or specialists, should clearly outline the patient's health condition, relevant diagnostic codes, and previous treatment attempts. For instance, records may include imaging studies like X-rays or MRIs, performed at accredited facilities like hospitals or imaging centers, which validate the necessity of the requested procedure. Furthermore, detailed notes on treatment plans, medications prescribed, and the patient's response to those treatments enhance the appeal's credibility. Including supporting letters from healthcare professionals and references to clinical guidelines or studies that advocate for the treatment can significantly strengthen the argument for approval.
Specific Insurance Policy References
The process of insurance pre-authorization appeals often involves specific policy references, such as plan numbers, coverage details, and relevant dates of service. Each insurance policy includes specific terms and conditions that outline the necessary criteria for approval of services. For instance, certain plans issued by Blue Cross Blue Shield may require additional documentation for procedures deemed non-emergency, while Aetna policies might stipulate pre-approval timelines of 72 hours for urgent cases. Understanding the unique aspects of the insurance provider's protocol enhances the ability to articulate a compelling argument when contesting a pre-authorization denial. Gathering supporting evidence, such as clinical guidelines, physician statements, and treatment history, can further strengthen the appeal.
Professional Healthcare Provider Endorsement
A professional healthcare provider endorsement represents a crucial step in the insurance pre-authorization appeal process. The endorsement, typically issued by a licensed physician or specialist, outlines the medical necessity of the requested procedure or treatment for individual patients. This document often includes key details such as the patient's medical history, specific diagnoses, and proposed interventions, ensuring that the insurance company understands the rationale behind the treatment recommendation. Statistics indicate that endorsements can significantly increase the likelihood of approval for procedures ranging from MRI scans to surgical operations, particularly for conditions requiring immediate attention, such as acute injuries or life-threatening illnesses. Providers must clearly reference relevant clinical guidelines and evidence-based practices, providing compelling arguments to support the case for coverage.
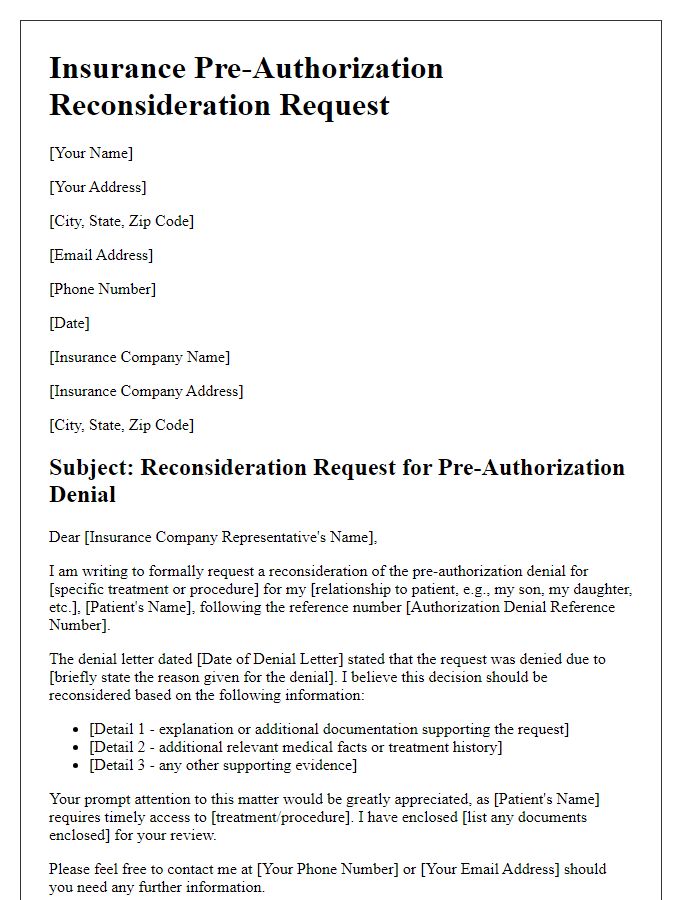
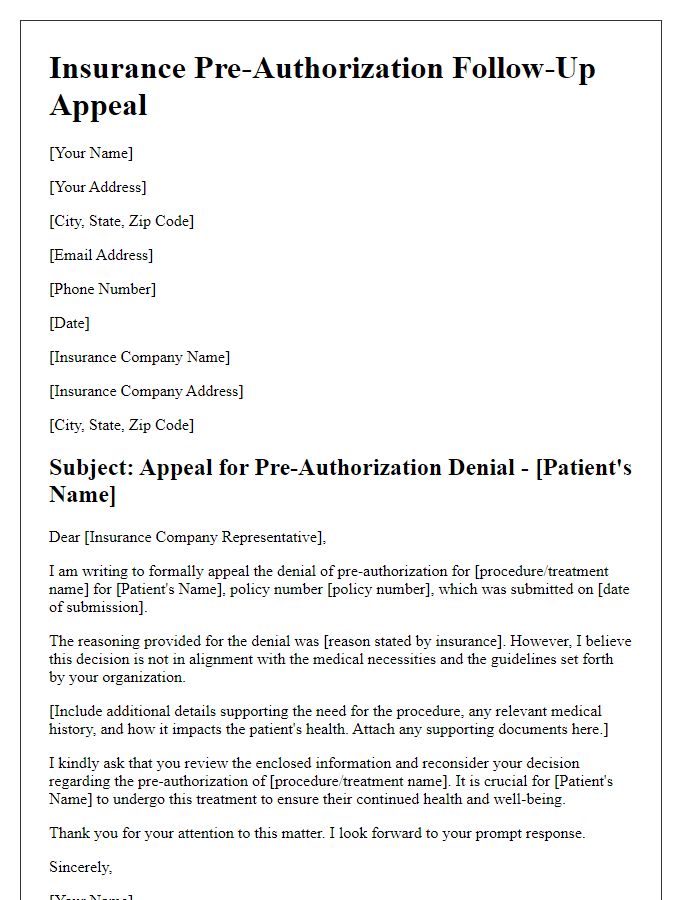
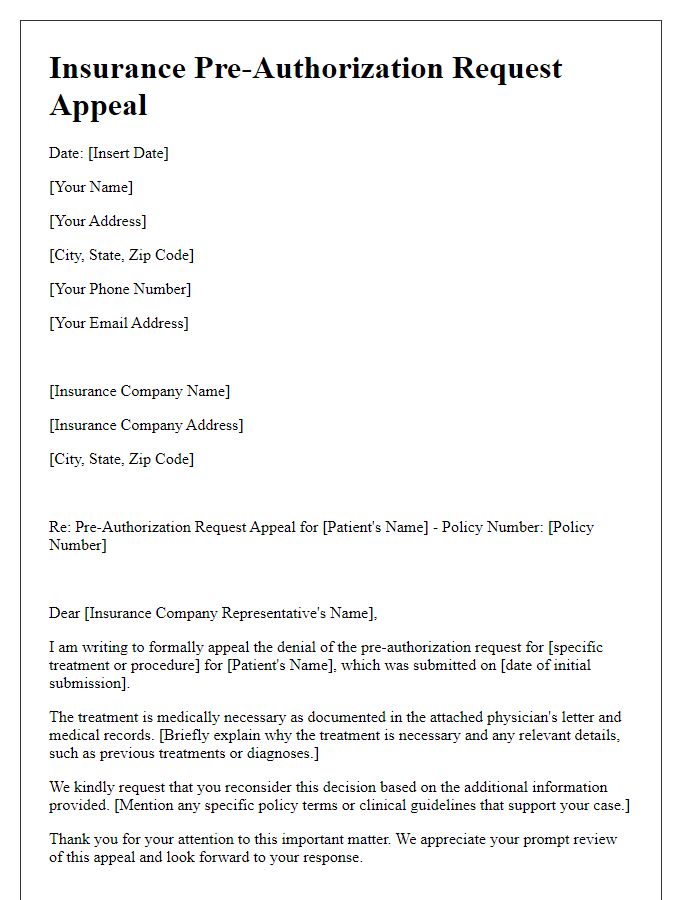
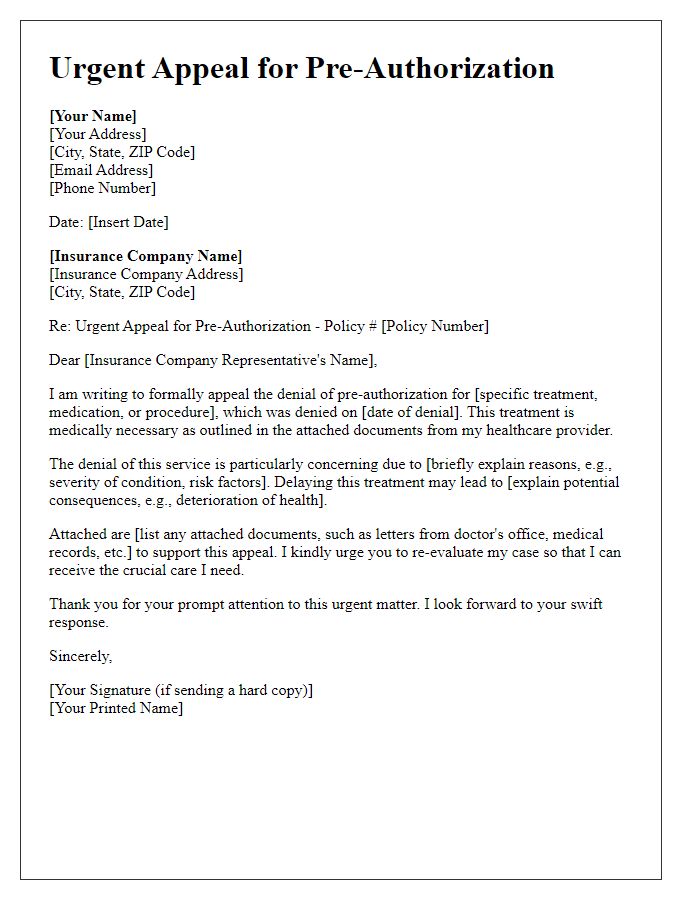
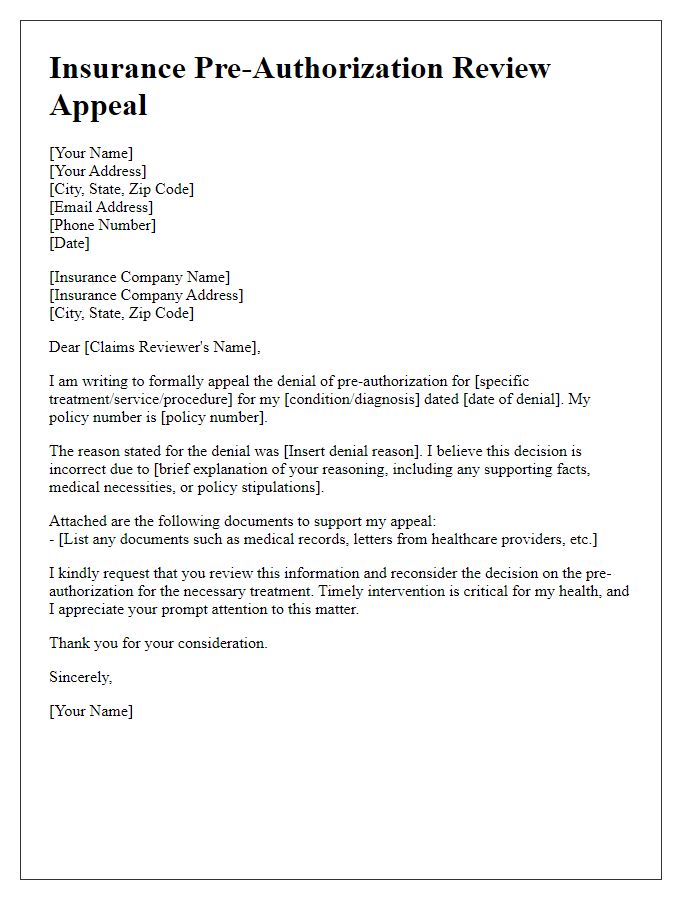
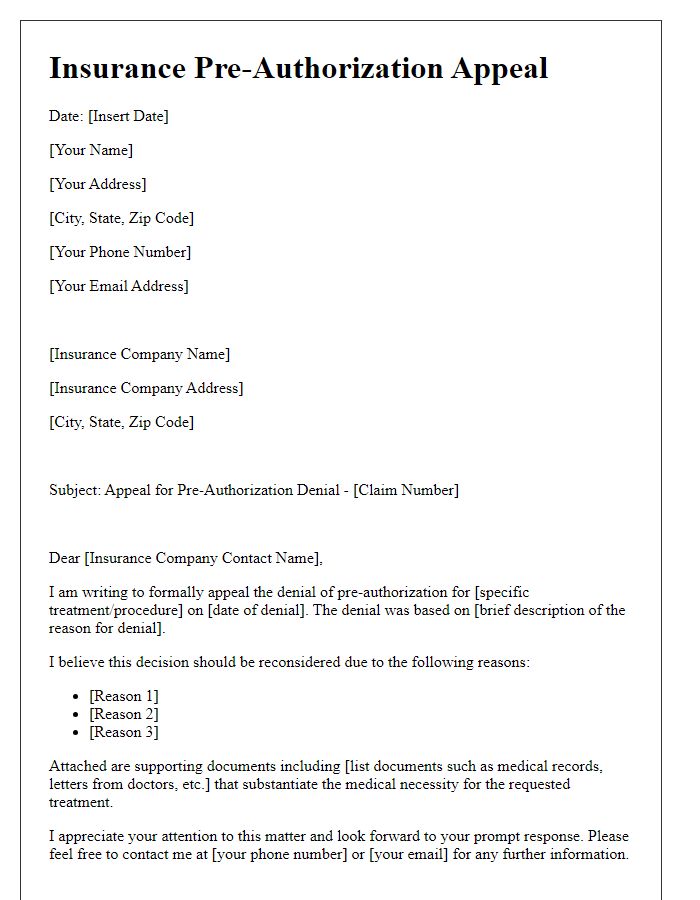
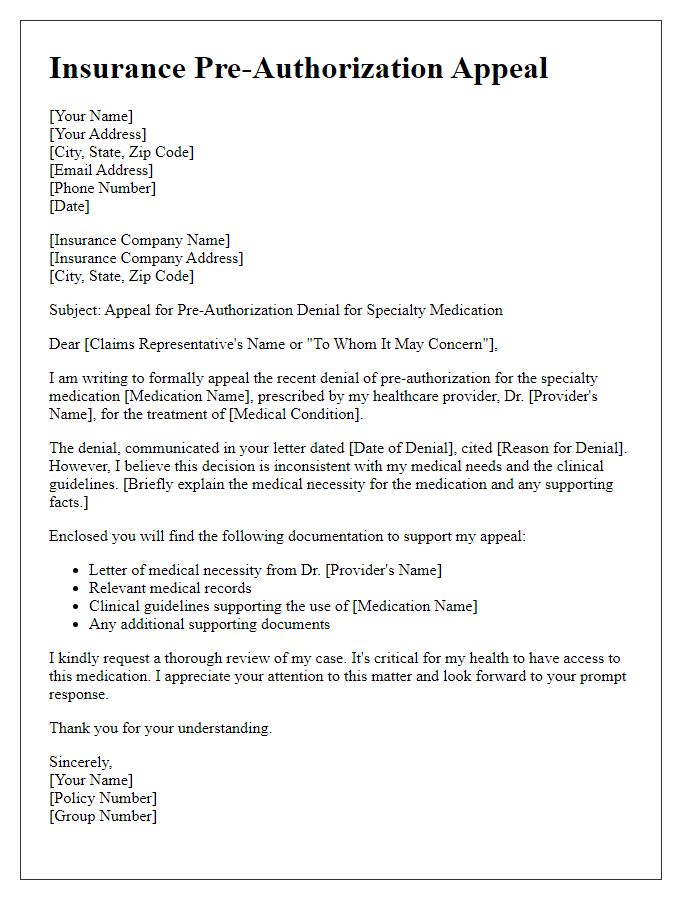
Letter Template For Insurance Pre-Authorization Appeal Samples
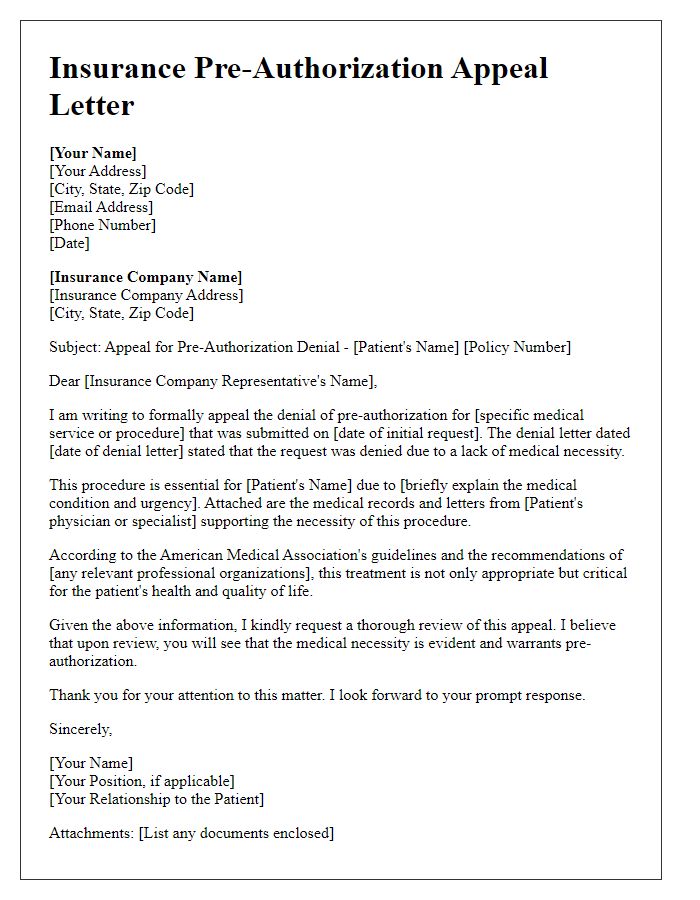
Letter template of insurance pre-authorization appeal for medical necessity
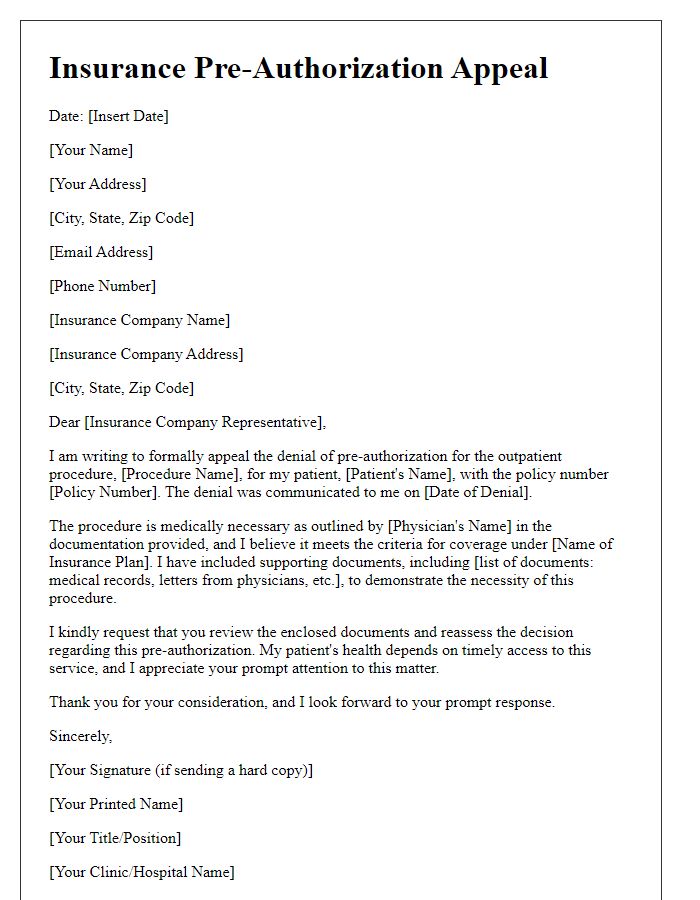
Letter template of insurance pre-authorization appeal for outpatient procedure


Comments