Managing diabetes can feel overwhelming, but a well-structured care routine can make all the difference. By incorporating simple lifestyle changes and consistent monitoring, you can take control of your health without sacrificing enjoyment in your daily life. It's all about finding what works best for you and adapting your approach as needed. Ready to dive deeper into crafting your personalized diabetic care routine? Keep reading!
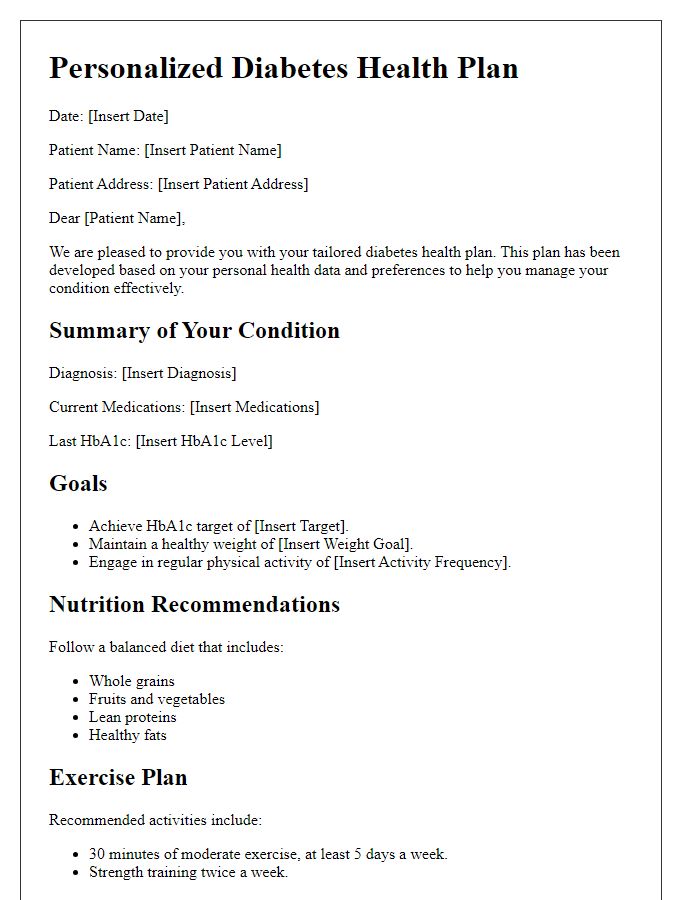
Personalization with patient's health history
Creating a personalized diabetic care routine requires a comprehensive understanding of the patient's health history. This includes details such as previous blood glucose readings (e.g., maintaining levels between 70-130 mg/dL before meals), incidents of hypoglycemia (e.g., low blood sugar episodes below 70 mg/dL), and the patient's medication regimen (including insulin types like Rapid-acting and Long-acting). Lifestyle factors such as dietary preferences (e.g., low-carb foods), exercise habits (e.g., at least 150 minutes of moderate aerobic activity per week), and psychological wellbeing (incorporating stress management techniques) also play critical roles. Regular monitoring strategies, including A1C tests twice a year to assess long-term glucose control, can further guide adjustments in meal planning, physical activity, and medication as necessary. Tailoring a routine based on these specific elements enhances adherence and improves overall health outcomes in managing diabetes effectively.
Comprehensive dietary guidelines
Adopting a comprehensive dietary plan is essential for individuals managing diabetes, particularly Type 1 and Type 2 diabetes. Specific guidelines focus on nutrient-dense foods, including whole grains such as brown rice and quinoa, lean proteins like chicken breast or fish, and healthy fats from sources like avocados and nuts. Carbohydrate counting can play a vital role, with recommended daily intake typically ranging from 45% to 60% of total calories, emphasizing low glycemic index foods to maintain stable blood sugar levels. Regular meal timing, ideally spaced every 4 to 5 hours, can help in preventing spikes and dips in insulin levels. Hydration is crucial; water should be the primary beverage choice, while monitoring the intake of caffeinated drinks. Portion control remains key, utilizing tools such as measuring cups and food scales, as well as understanding serving sizes to prevent overconsumption. Comprehensive education on reading food labels assists in making informed food choices, enhancing overall dietary adherence.
Incorporation of exercise recommendations
Regular physical activity plays a crucial role in managing diabetes mellitus, significantly affecting blood sugar levels and overall health. The American Diabetes Association recommends at least 150 minutes of moderate aerobic exercise weekly, such as brisk walking, swimming, or cycling, to help improve insulin sensitivity. Resistance training exercises, like weight lifting or bodyweight workouts, should be integrated at least twice a week to strengthen muscles and enhance glucose metabolism. These activities help maintain a healthy weight, reducing the risk of complications associated with diabetes. Consultation with healthcare providers is essential to tailor an exercise regimen that considers individual health conditions and fitness levels, ensuring safety and effectiveness in achieving health goals. Incorporating movement into daily routines can include simple changes, such as taking the stairs instead of elevators or engaging in leisure activities that promote physical wellness.
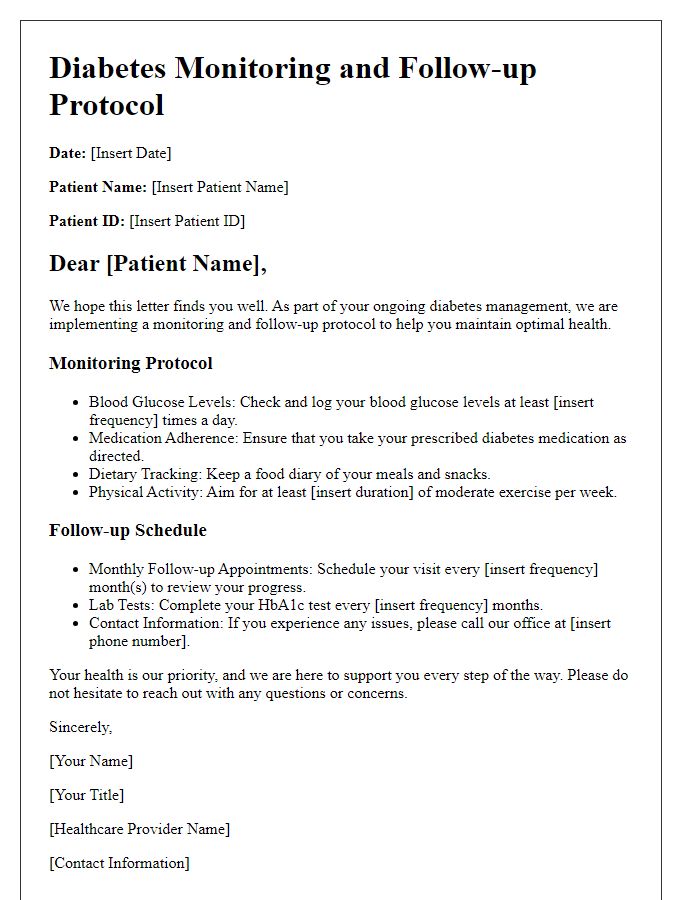
Monitoring and tracking blood sugar levels
Monitoring and tracking blood sugar levels is essential for effective diabetes management, particularly in individuals diagnosed with Type 1 and Type 2 diabetes. Regular checking, ideally at least four times a day, can provide valuable insights into glucose patterns. Utilizing a continuous glucose monitor (CGM), such as the Dexcom G6, allows individuals to receive real-time readings, reducing the occurrence of both hyperglycemia (blood sugar above 130 mg/dL) and hypoglycemia (blood sugar below 70 mg/dL). Keeping a detailed logbook or using mobile apps like MySugr enables tracking of food intake, insulin doses, and physical activity, which helps in identifying trends and making necessary dietary adjustments. Collaborating with healthcare professionals, such as endocrinologists or certified diabetes educators, is crucial for tailoring specific strategies that align with personal lifestyle and health goals. Regular assessments, ideally every three months through an A1C test, measure long-term glucose control, providing a comprehensive view of one's diabetic care routine.
Medication and insulin administration instructions
A diabetic care routine requires meticulous attention to medication and insulin administration for optimal blood glucose management. Medications such as Metformin or Sulfonylureas are typically prescribed to manage blood sugar levels. Insulin therapy, often essential for Type 1 diabetes patients, may involve types like rapid-acting (e.g., Lispro), long-acting (e.g., Glargine), or mixed insulin formulations. Administration techniques can vary by device; for example, insulin pens and syringes enable subcutaneous injections aimed at abdominal fat pads or thigh areas, with recommended rotation every injection to prevent lipodystrophy. Key monitoring includes regular blood glucose readings--ideally four to six times daily--using glucometers, capturing fasting levels around 80-130 mg/dL, and postprandial levels below 180 mg/dL. Additionally, understanding carbohydrate counting and the glycemic index's impact on blood sugar is crucial for meal planning and avoiding extreme fluctuations. Regular consultations with healthcare professionals, like endocrinologists or diabetes educators, ensure that adjustments to the care routine are made based on individual progress and glucose patterns.



Comments