Are you curious about how a personalized care plan can transform your health journey? In today's world, where one-size-fits-all solutions often fall short, tailoring your care to meet your unique needs is more important than ever. A personalized care plan not only addresses your specific health concerns but also empowers you to take an active role in your well-being. Keep reading to discover how you can benefit from a customized approach to healthcare!
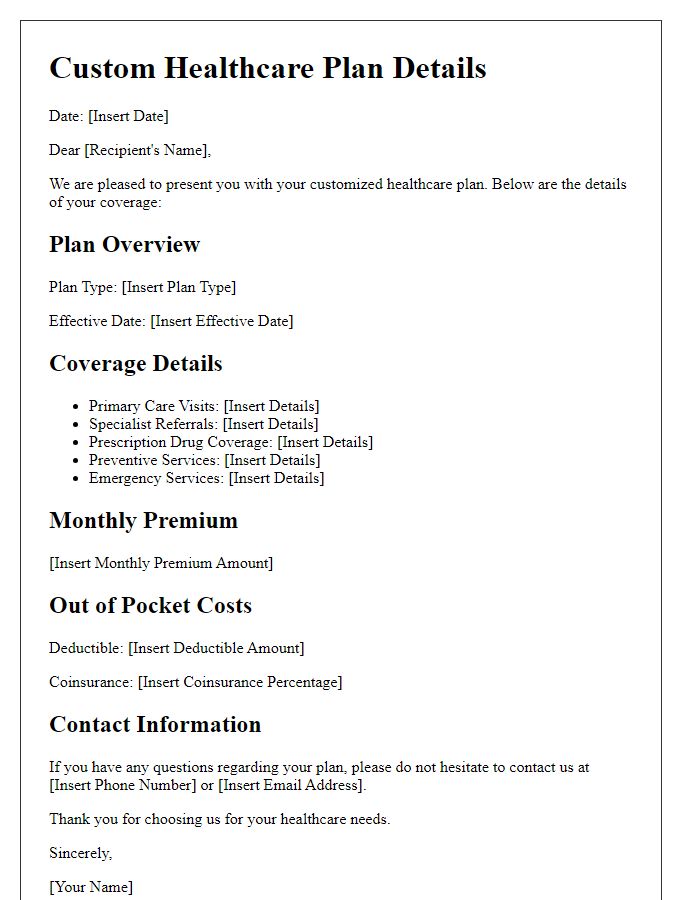
Patient's medical history and current health status
Patient's medical history reveals a range of significant conditions, including Type 2 Diabetes, diagnosed at age 45, and Hypertension, noted since age 50. Current health status indicates a recent HbA1c level of 8.2%, showing suboptimal blood sugar control. Additionally, Blood Pressure readings average 150/90 mmHg, suggesting the need for monitoring and potential adjustments in medication. Current medication regimen includes Metformin for diabetes management and Lisinopril for hypertension. Patient reports symptoms such as occasional fatigue and dizziness, which may indicate the need for further assessment of both medication efficacy and lifestyle factors, including diet and physical activity levels. Regular check-ups are essential for evaluating ongoing effectiveness of the personalized care plan to enhance overall well-being.
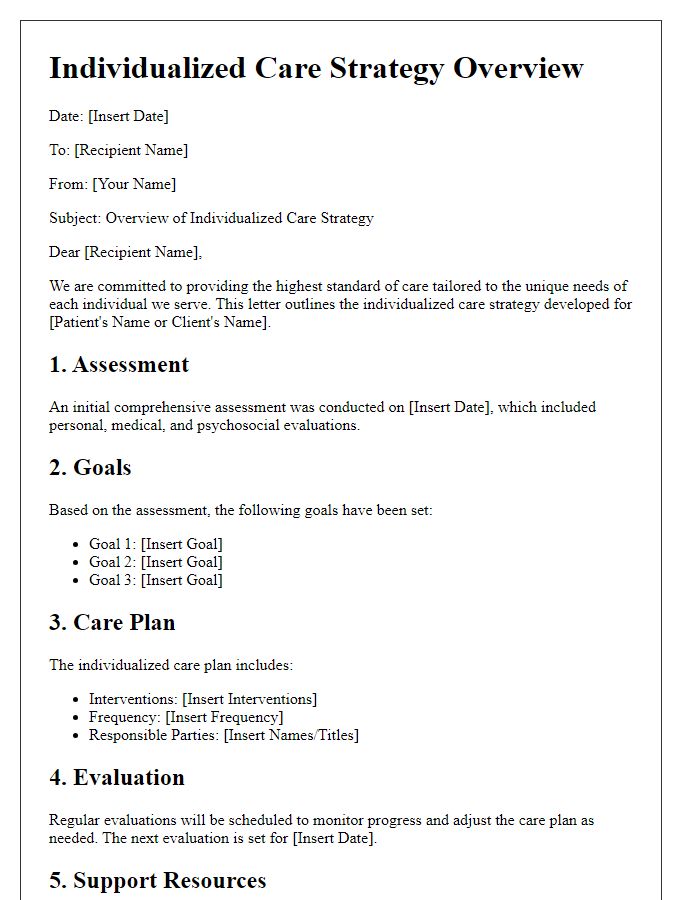
Individualized treatment goals and objectives
An individualized care plan emphasizes personalized treatment goals and objectives tailored to each patient's unique needs. This plan might include specific health conditions, such as diabetes management or post-operative recovery, along with measurable outcomes like achieving blood sugar levels below 130 mg/dL or improving mobility to a certain distance (e.g., 100 meters) within a fixed timeframe (like three months). Key components involve regular assessments (e.g., weekly check-ups), tailored therapeutic interventions (such as physical therapy sessions or dietary modifications), and continuous engagement with healthcare providers, ensuring that the care plan evolves with the patient's progress. Furthermore, incorporating emotional support strategies, such as counseling or support groups, can significantly enhance the overall well-being of the patient, facilitating a holistic approach to health management.
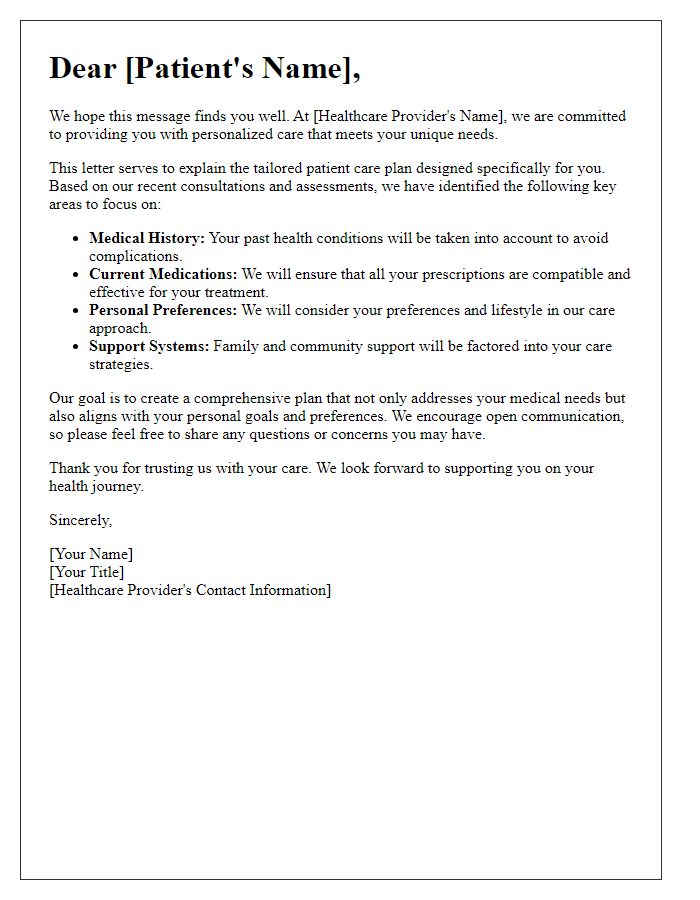
Specific interventions and therapies recommended
A personalized care plan often includes specific interventions and therapies tailored to meet an individual's unique health needs and circumstances. For instance, in the case of diabetes management, recommended interventions may include carbohydrate counting techniques combined with daily blood glucose monitoring practices. In addition, physical activity might be prescribed, such as a structured exercise program offering at least 150 minutes of moderate aerobic activity weekly, tailored to suit the patient's limitations or preferences. Dietary consultations from registered dietitians, especially focusing on nutritious eating habits emphasizing whole grains and vegetables, are often integral. Mental health support through cognitive behavioral therapy may also be beneficial, addressing any coexisting anxiety or depression associated with chronic illness. Each intervention aims to promote improved health outcomes and enhanced quality of life.
Monitoring and follow-up schedule
A personalized care plan is essential for managing health conditions effectively. The monitoring schedule typically involves regular check-ups, often every 4 to 6 weeks, to assess progress and make necessary adjustments. Follow-up appointments may occur at medical facilities like community health clinics or specialty hospitals, ensuring one-on-one support from healthcare professionals. Key health metrics such as blood pressure measurements, glucose levels, or medication adherence are monitored to gauge effectiveness. Communication channels, including telehealth consultations, provide timely updates and adjustments to the treatment plan as required. These measures foster accountability and facilitate early detection of any complications, ensuring optimal patient outcomes.
Patient and caregiver instructions and education
A personalized care plan emphasizes tailored instructions and education for the patient and caregiver, ensuring optimal management of health conditions. Clear guidelines should be provided, detailing medication schedules, including types and dosages, alongside potential side effects to monitor. Nutrition guidelines should specify daily intake recommendations, including portion sizes and food categories, catering to any dietary restrictions, such as gluten-free or low-sodium needs. Furthermore, physical activity recommendations, such as moderate walking for at least 30 minutes five times a week, help promote overall wellness while accounting for mobility limitations. Regular monitoring of vital signs, such as blood pressure (maintaining a target below 130/80 mmHg), should be incorporated, emphasizing the importance of communication with healthcare professionals for any concerning changes. Caregiver education should focus on recognizing symptoms that necessitate immediate medical attention, ensuring support measures, such as emotional and logistical assistance, are in place to enhance quality of life.


Comments