Navigating the journey of pregnancy can be both exhilarating and overwhelming, which is why having a solid obstetric care plan is essential. A well-structured care plan not only ensures that expectant mothers receive the best medical support but also empowers them to participate actively in their own health decisions. In this article, we will outline a letter template that can help you communicate effectively with your healthcare provider regarding your specific needs and preferences. So, let's dive in and explore how you can create a personalized obstetric care plan that works for you!

Patient Demographics
Patient demographics serve as a foundational element in the obstetric care plan, encompassing critical information such as maternal age (e.g., 28 years), geographic location (e.g., Los Angeles, California), medical history (e.g., previous pregnancies or chronic conditions), and socio-economic factors (e.g., income level, education) that influence patient care. Additional identifiers may include ethnicity (e.g., Hispanic), marital status (e.g., married), and language preference which facilitate efficient communication and culturally sensitive care. Accurate capture of these demographics ensures tailored obstetric management and fosters a supportive healthcare environment throughout pregnancy.
Medical and Obstetric History
A comprehensive obstetric care plan should include a detailed medical and obstetric history to ensure informed decision-making throughout pregnancy. This history typically includes previous pregnancies or complications, such as gestational diabetes or preeclampsia, which may impact current care. Additionally, chronic health conditions, such as hypertension or thyroid disorders, must be documented as they can influence maternal and fetal health. Past surgical procedures, including cesarean deliveries, should be noted for potential implications on delivery options. Family medical history, especially genetic disorders or heritable conditions, can guide screening decisions. Tracking immunization status, particularly for rubella and varicella, is crucial for protecting both mother and baby. Each of these components plays a vital role in tailoring individual prenatal care, ensuring the safety and well-being of both the mother and child.
Current Pregnancy Details
The current pregnancy details provide critical insights into maternal and fetal health, encompassing essential information such as gestational age, typically measured in weeks since the last menstrual period, which influences prenatal care protocols. The estimated due date (calculated from the first day of the last menstrual period or via ultrasound measurements) is important for assessing developmental milestones and necessary interventions. Maternal weight gain trends, monitored against recommended guidelines by organizations like the American College of Obstetricians and Gynecologists, help evaluate nutritional status. Any notable medical history, including pre-existing conditions such as hypertension or diabetes, requires careful monitoring and management to ensure optimal outcomes. Additionally, information related to previous pregnancies, such as live births, complications like preeclampsia, or cesarean deliveries, provides a context for individualized care plans. Routine assessments like blood pressure readings and fetal heart rate monitoring contribute to ongoing evaluations of wellness throughout the trimesters of pregnancy.
Antenatal Care Schedule
Antenatal care schedules are crucial for expecting mothers, outlining essential medical appointments and tests during pregnancy. Typical schedules begin during the first trimester (weeks 1-12), emphasizing critical assessments such as blood tests, ultrasound scans, and early health screenings to identify any risks. As pregnancy progresses into the second trimester (weeks 13-26), routine visits occur every four weeks, including detailed anatomical scans (especially around 20 weeks) to monitor fetal development and maternal health. In the third trimester (weeks 27-40), visits become more frequent, typically every two weeks initially and then weekly as the delivery date approaches. Topics covered during these appointments include gestational diabetes screening, blood pressure monitoring, and discussions on labor plans. Special attention is needed for high-risk pregnancies, requiring additional consultations and possibly specialized ultrasounds. By adhering to this comprehensive antenatal care schedule, expectant mothers can better ensure the well-being of both themselves and their babies.
Labor and Delivery Preferences
Labor and delivery preferences outline essential choices regarding childbirth, reflecting the expectant mother's values and desires. Key areas include pain management options, such as epidural analgesia which can significantly relieve labor pain, or natural methods like breathing techniques and hydrotherapy (using water to ease discomfort). Environment preferences within the delivery room may involve dim lighting and music to create a calming atmosphere, enhancing emotional well-being. Positions for labor and delivery offer choices like upright, squatting, or on hands and knees, which can promote better fetal positioning and reduce labor duration. Interventions, including continuous fetal monitoring or limited vaginal exams, outline expectations for medical involvement. Postpartum preferences can additionally address skin-to-skin contact (immediate bonding with the newborn), breastfeeding intentions, and visitor guidelines to facilitate a supportive recovery environment.
Letter Template For Obstetric Care Plan Outline Samples
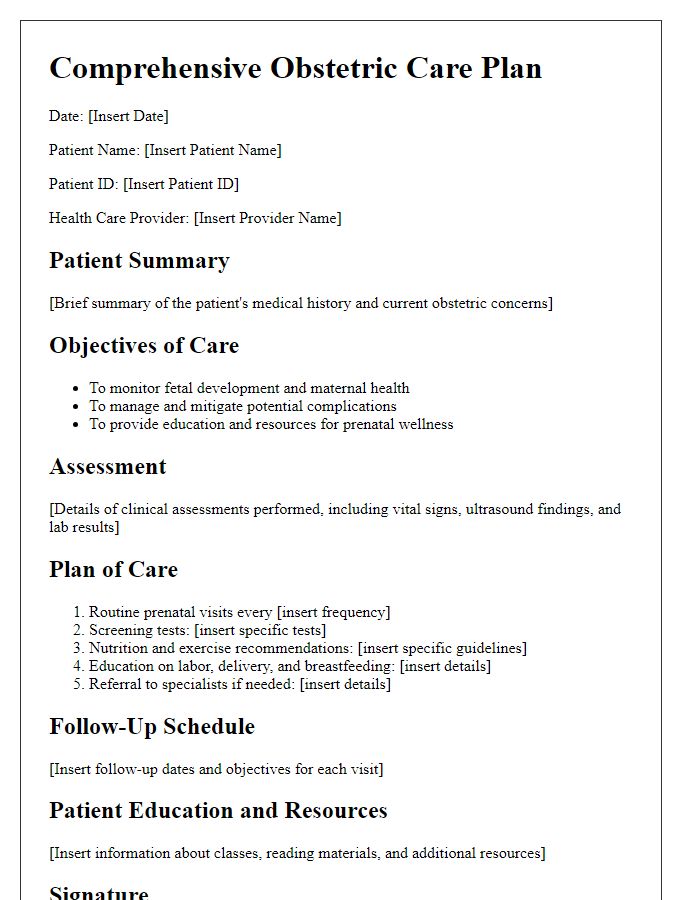
Letter template of comprehensive obstetric care plan for prenatal patients
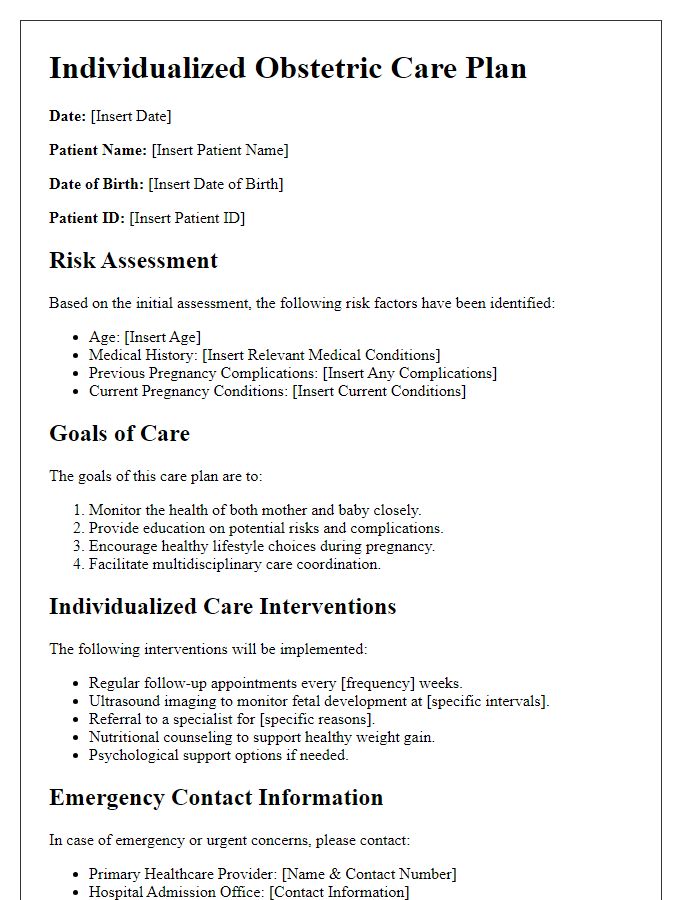
Letter template of individualized obstetric care plan for high-risk pregnancies
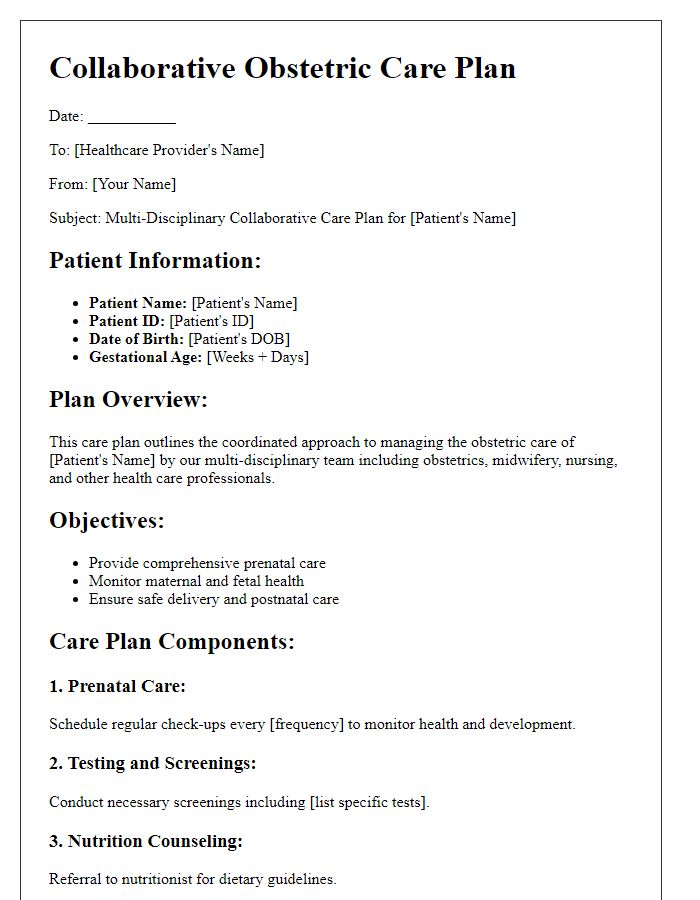
Letter template of collaborative obstetric care plan for multi-disciplinary teams
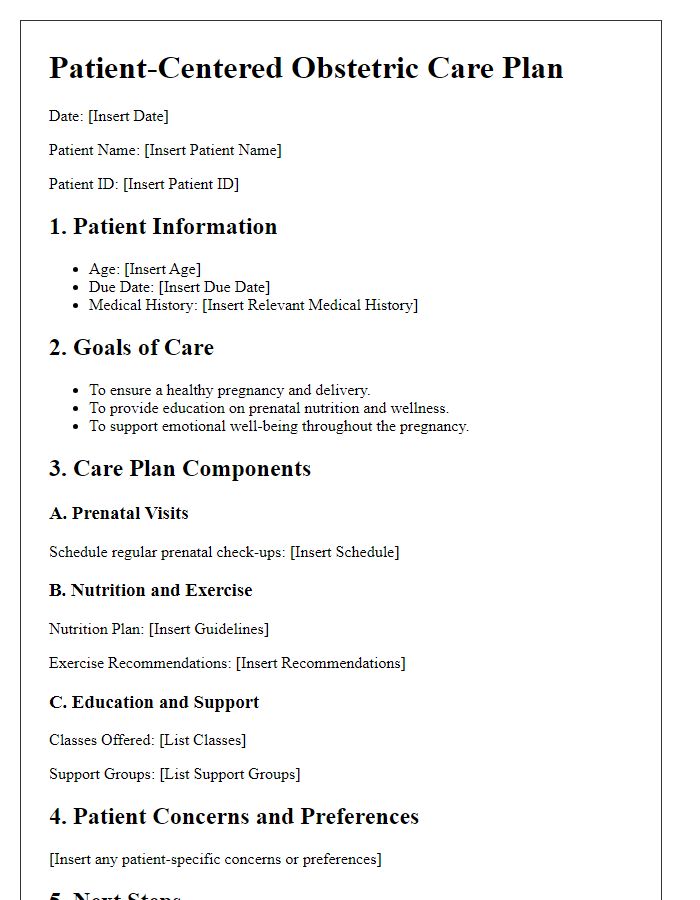
Letter template of patient-centered obstetric care plan for expectant mothers
Letter template of educational obstetric care plan for first-time parents
Letter template of customized obstetric care plan for managing pregnancy complications
Letter template of follow-up obstetric care plan for ongoing maternal health


Comments