When it comes to medical procedures, understanding the ins and outs is crucial for both the provider and the patient. A well-crafted consent form not only ensures that patients are informed but also strengthens the relationship between doctors and those they treat. Navigating the complexities of medical consent can feel overwhelming, but it doesn't have to be. Ready to dive deeper into the essentials of a medical procedure consent form? Let's explore together!
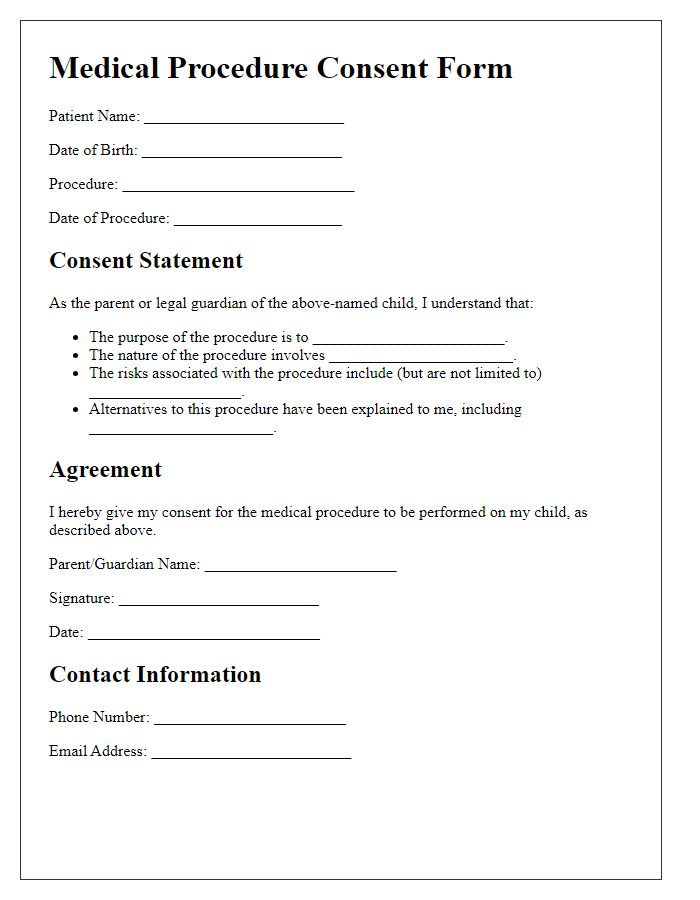
Patient Identification and Demographics
Patient identification is crucial in ensuring the accuracy and safety of medical procedures. Key details include full name (first, middle, last), date of birth (DD/MM/YYYY), gender, and identification number (such as Social Security Number or hospital ID). Additionally, contact information is essential: current address, phone number, and email address. Insurance information should specify provider name, policy number, and group number if applicable. Emergency contact details must include the name, relation, and phone number of a designated person who can be reached if needed. Thorough collection of these demographics aids in accurate medical record-keeping and enhances communication between healthcare providers and patients, facilitating informed decisions regarding procedures.
Description of the Procedure
The medical procedure known as laparoscopic cholecystectomy involves the surgical removal of the gallbladder (a small organ located beneath the liver that stores bile) using minimally invasive techniques. The operation is typically performed using small incisions in the abdomen, often with the assistance of a camera (laparoscope). This technique generally results in reduced recovery time (approximately one week compared to several weeks for open surgery) and minimized scarring. The procedure is indicated for individuals with symptomatic gallstones or gallbladder disease, often presenting with pain, nausea, or digestive issues. Risks include infection, bleeding, and injury to nearby organs, such as the bile ducts. Monitoring usually occurs in a hospital setting, with discharge typically within 24 hours if no complications arise. Post-operative guidelines recommend light physical activity and a gradual return to a normal diet within days following the procedure.
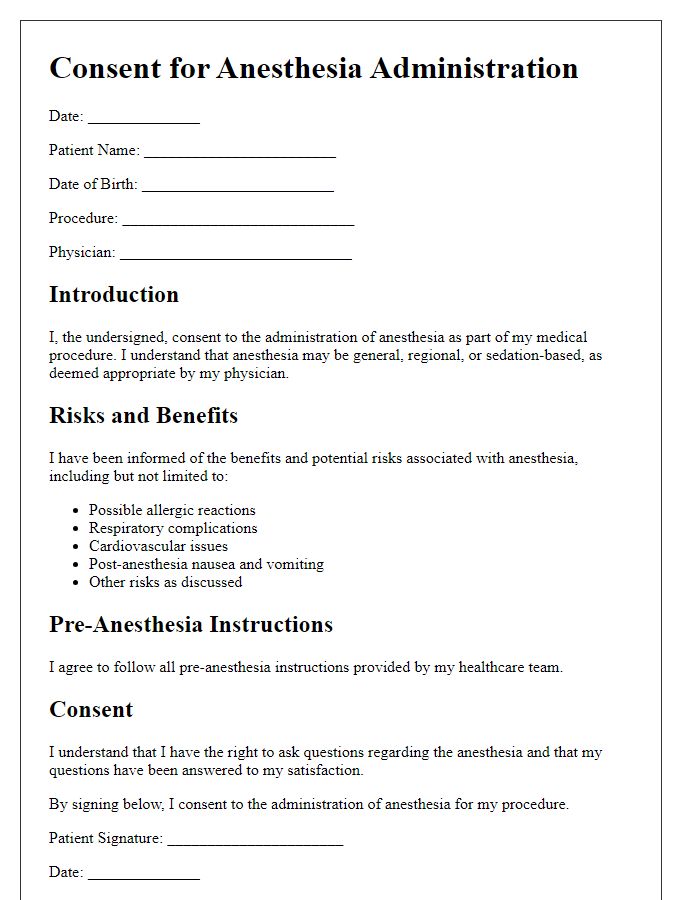
Risks and Potential Complications
Medical procedures, such as surgeries or diagnostic tests, carry inherent risks and potential complications that patients must be informed about prior to consent. Common risks may include infection, which affects surgical sites or body systems, and can occur in approximately 3-5% of cases. Bleeding may also be a concern, particularly with procedures involving the incision of blood vessels, where blood loss could exceed 500 milliliters. Anesthesia reactions, though rare, can pose serious threats, with about 1 in 100,000 patients experiencing adverse effects. Other complications include blood clots, which can lead to deep vein thrombosis (DVT) in around 1-2% of surgical patients, and organ damage, which varies depending on the specific procedure but can have long-term ramifications. Understanding these risks aids in making informed decisions regarding health treatments.
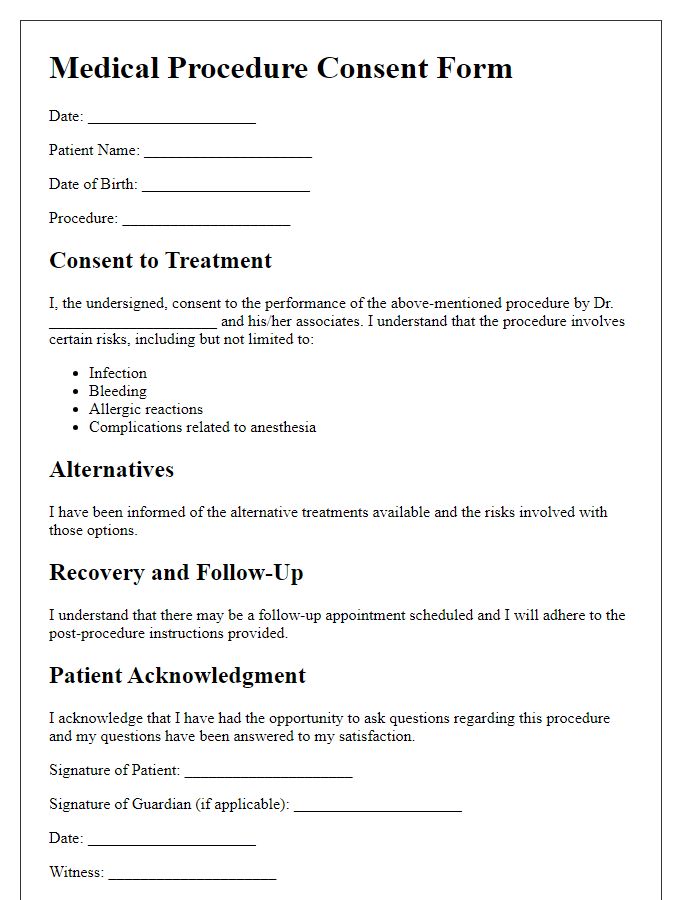
Benefits and Alternatives
Medical procedure consent forms outline essential information, including the benefits and alternatives associated with the proposed treatment. Understanding the benefits, such as improved health outcomes, relief from symptoms, and enhanced quality of life, helps patients make informed decisions. For example, a knee replacement surgery can result in significant pain reduction and increased mobility for patients suffering from osteoarthritis. Alternatives, such as physical therapy, medication, or minimally invasive procedures, should be presented clearly, enabling patients to weigh their options effectively. This process promotes patient autonomy while emphasizing the importance of thorough discussions with healthcare providers to ensure alignment with individual health goals.
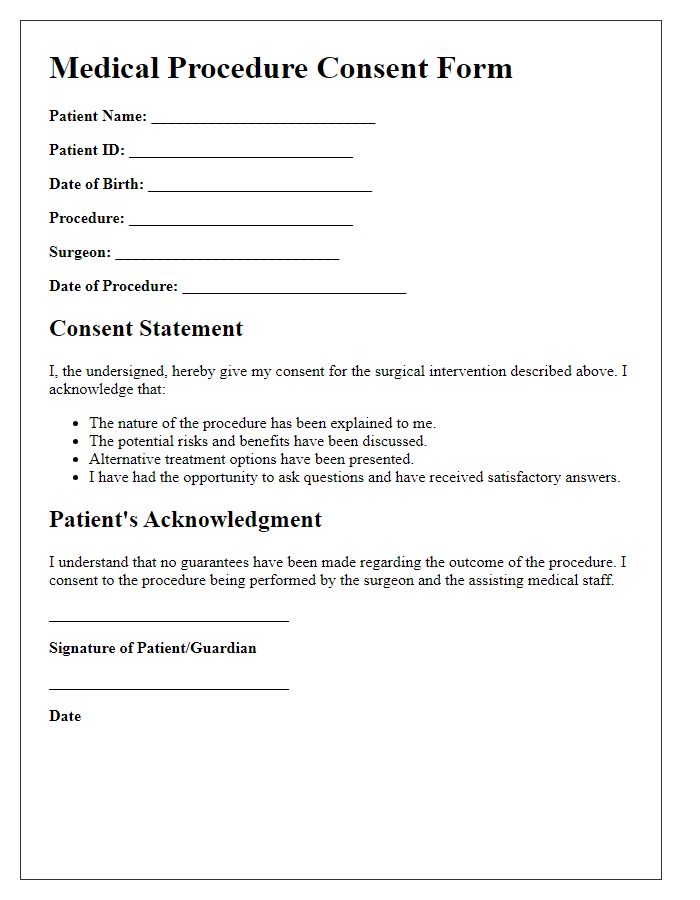
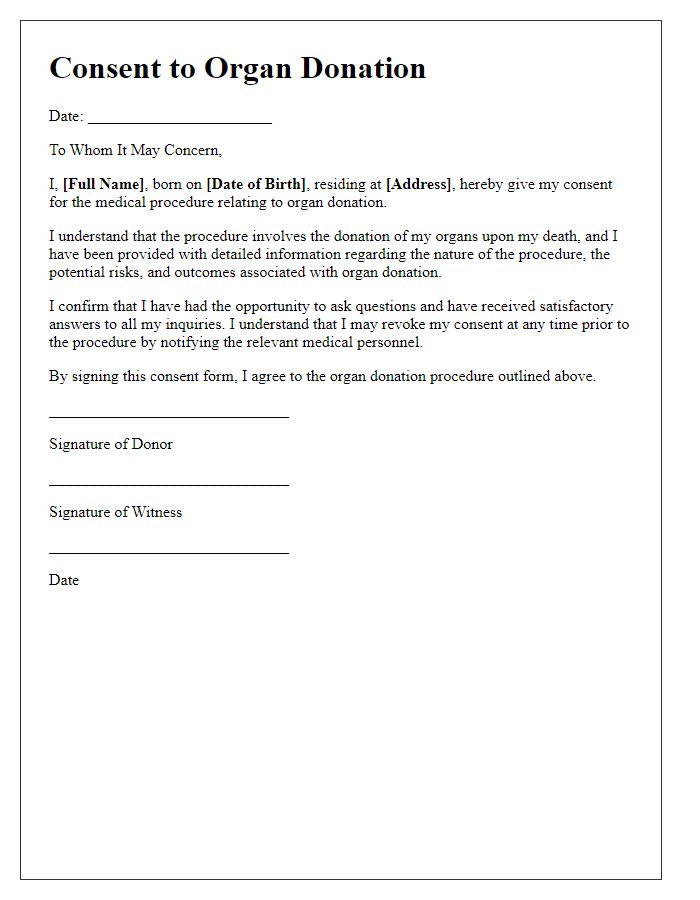
Patient Acknowledgement and Signature
Consent for medical procedures is a crucial step in ensuring patient autonomy and understanding. When patients review consent forms, they acknowledge the risks, benefits, and alternatives associated with their specific interventions, such as surgery or diagnostic procedures. The form typically includes sections detailing the procedure's name, purpose, and potential complications. By signing, patients affirm their comprehension of the information presented and agree to proceed, often noting the date and any specific questions discussed with their healthcare provider. This signature not only signifies informed consent but also promotes communication about expectations regarding the procedure and recovery.
Letter Template For Medical Procedure Consent Form Samples
Letter template of medical procedure consent form for surgical intervention
Letter template of medical procedure consent form for anesthesia administration
Letter template of medical procedure consent form for outpatient procedure
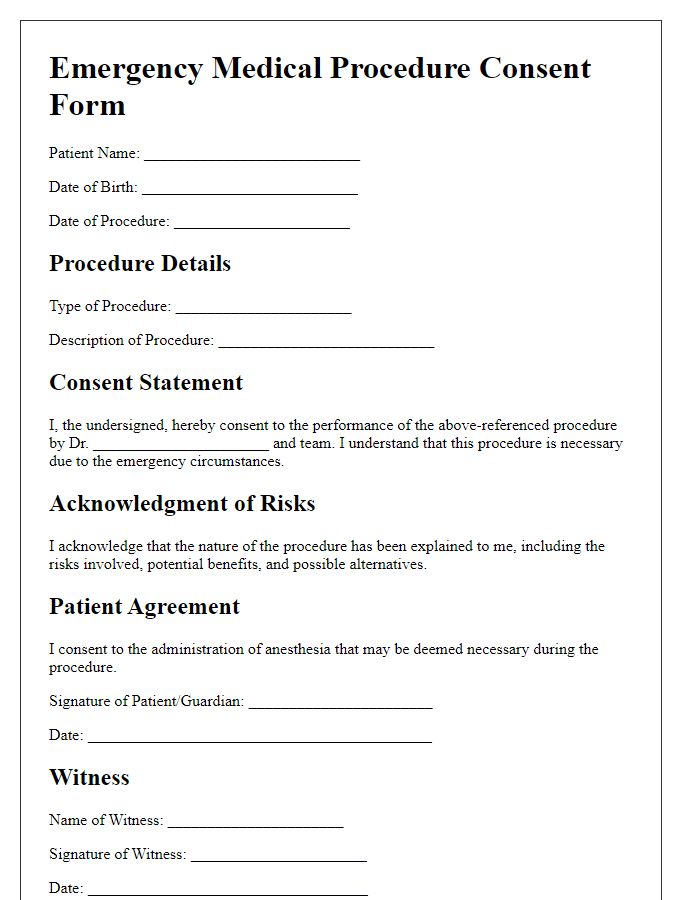
Letter template of medical procedure consent form for emergency procedures
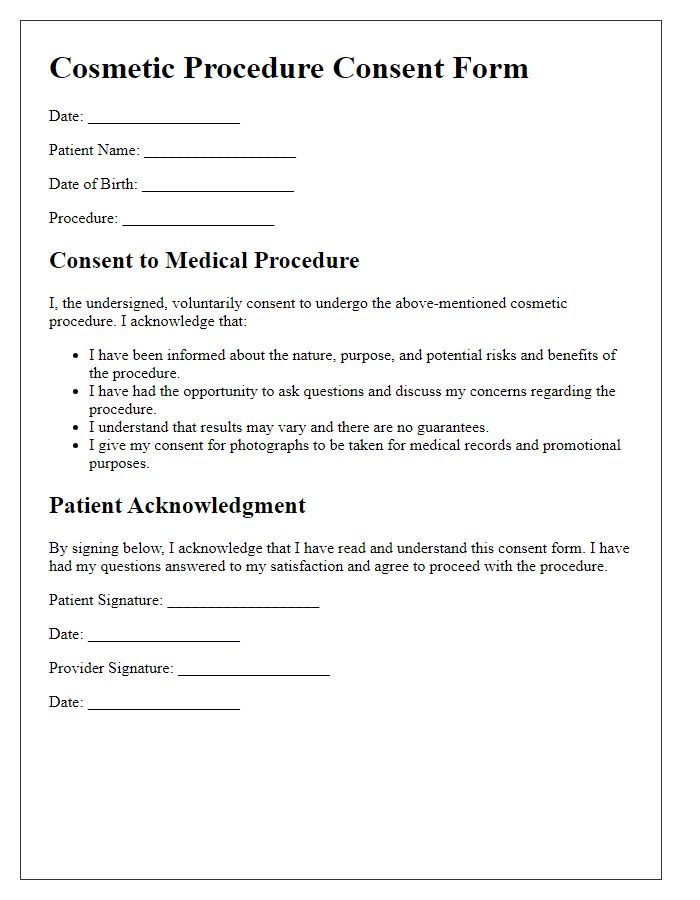
Letter template of medical procedure consent form for cosmetic procedures
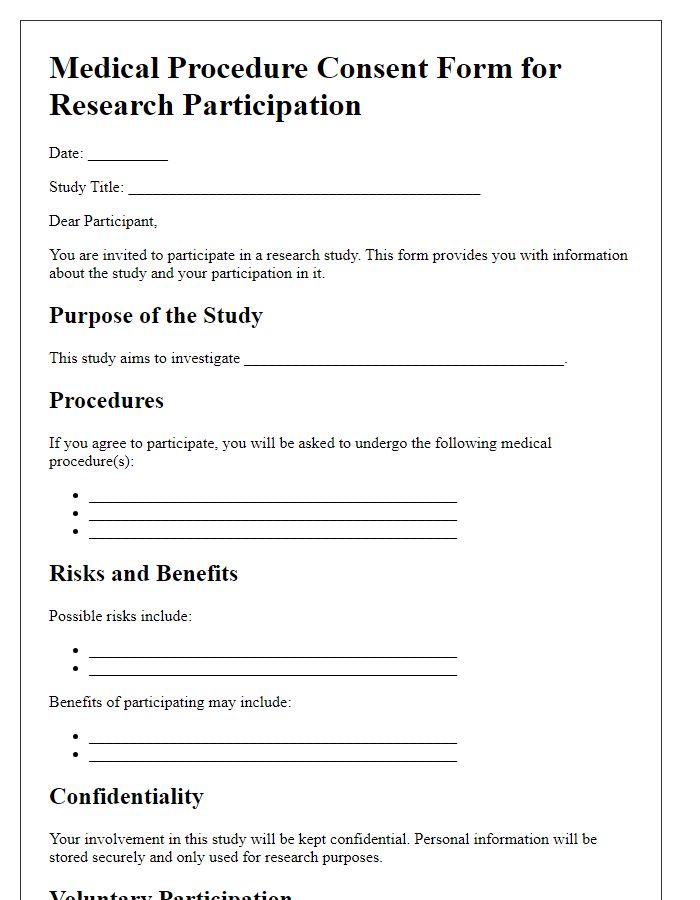
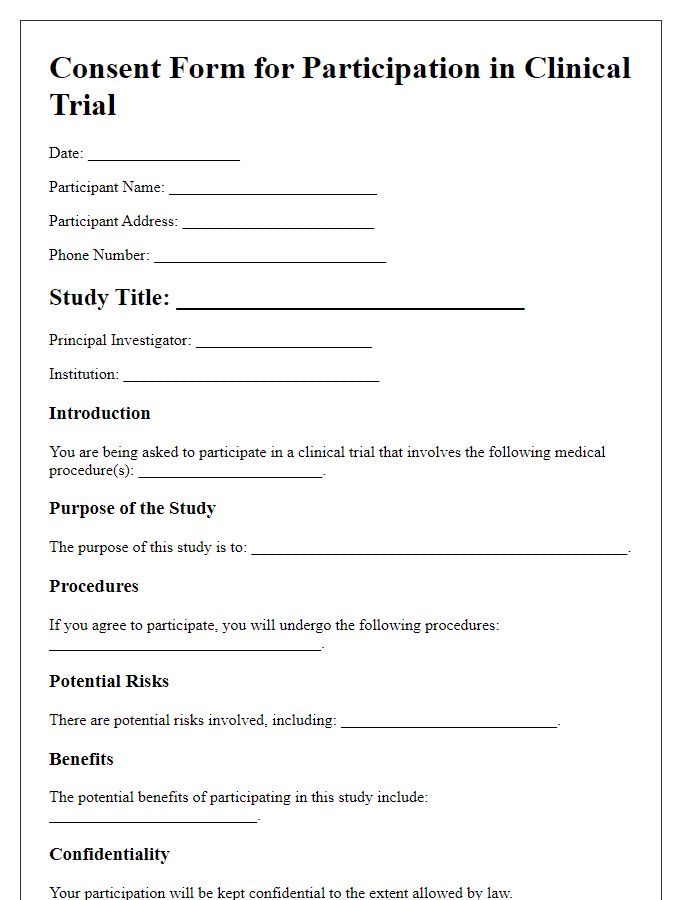
Letter template of medical procedure consent form for research participation


Comments