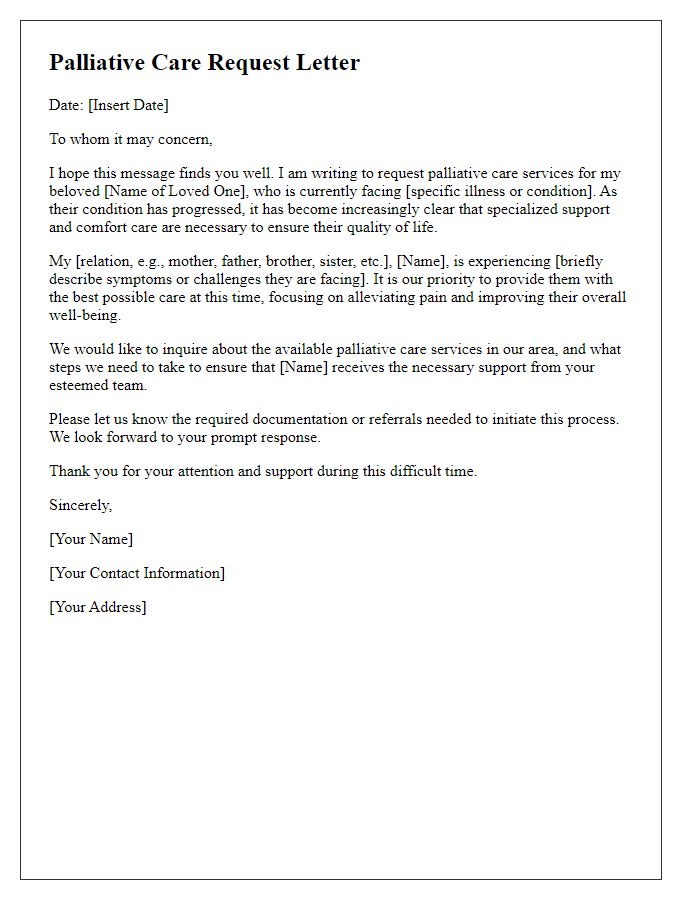
When it comes to making palliative care arrangements, clarity and compassion are key. This essential process not only ensures that individuals receive the best possible care but also brings peace of mind to families during a challenging time. In this article, we'll explore the important elements of crafting a palliative care plan, from communication with healthcare providers to understanding patient preferences. Join us as we delve deeper into this vital topic and equip ourselves with the knowledge to navigate these sensitive discussions effectively!
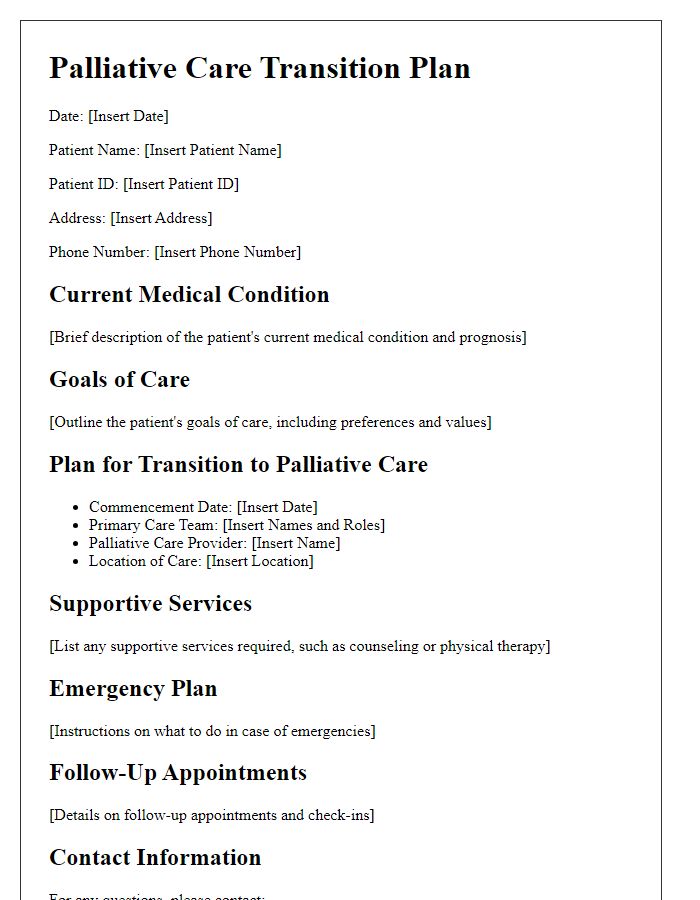
Personalized Patient Information
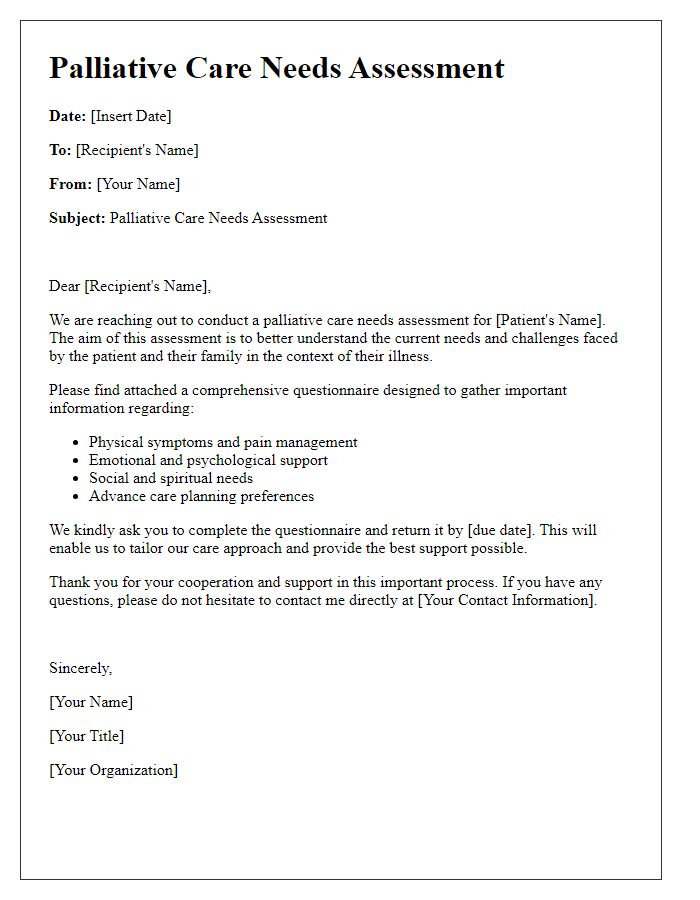
Palliative care arrangements encompass comprehensive support for patients with serious illnesses, emphasizing comfort and quality of life. Detailed patient information includes critical elements such as diagnosis, treatment history, and symptom management preferences. Care plans outline specific interventions tailored to individual needs, ensuring emotional support from caregivers and family members. Locations such as hospitals, in-home care settings, or hospice facilities dictate the necessary resources and support services available. Essential elements in communication involve ongoing discussions regarding patient wishes, including advance directives and end-of-life preferences, fostering a collaborative environment between healthcare professionals, patients, and families. Regular assessments and adjustments in care plans guarantee that patient-centered approaches meet the evolving needs throughout the palliative care journey.
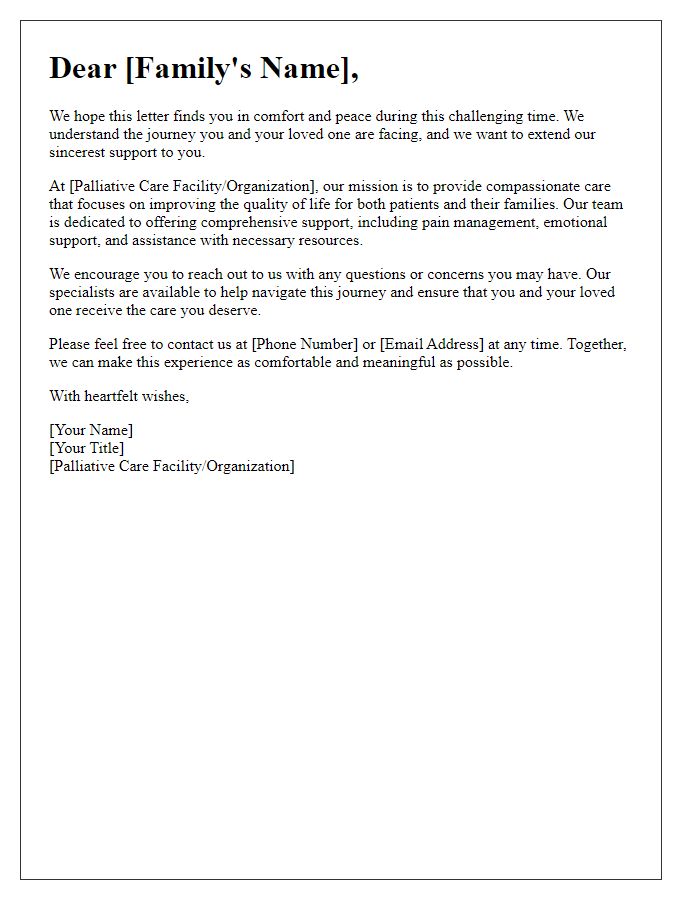
Treatment Goals and Preferences
Palliative care arrangements focus on enhancing the quality of life for patients with serious illnesses, emphasizing comfort and support. Treatment goals encompass symptom management, such as pain relief and emotional support, tailored to individual needs. Preferences for care often include the setting, such as home or hospice environments, where patients can feel at ease. Additionally, advanced care planning discussions frequently involve family members and healthcare providers to ensure alignment on objectives, respecting the patient's wishes and dignity. Regular assessments and adjustments to the care plan are crucial to address changing symptoms and needs, fostering a holistic approach that prioritizes the patient's comfort and well-being.
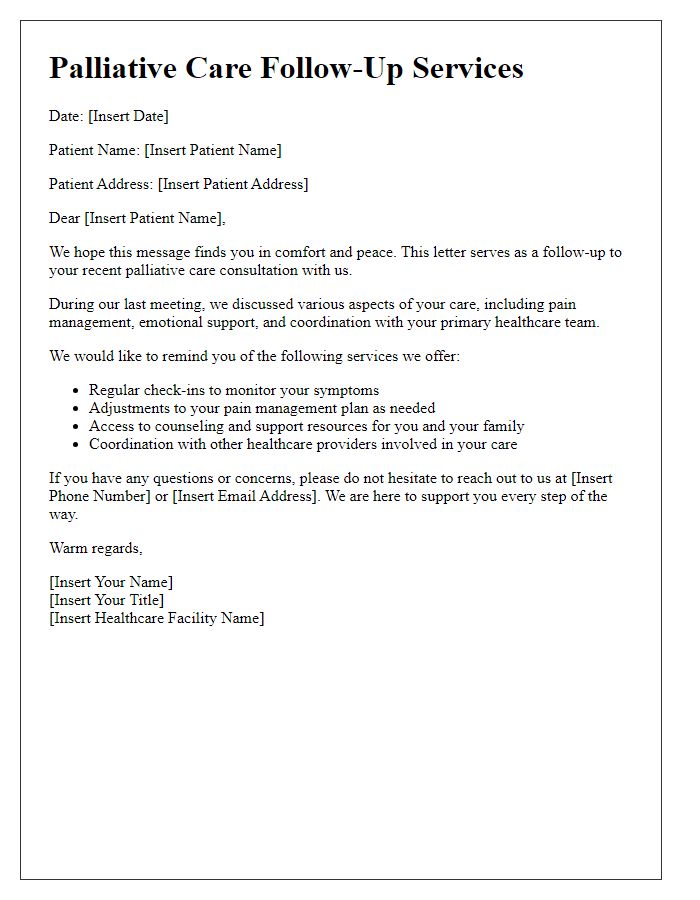
Support Services and Resources
Palliative care arrangements encompass a variety of support services and resources aimed at providing comprehensive care for patients with serious illnesses. These services often include pain management resources such as opioids and alternative therapies (like acupuncture) to enhance the quality of life. Emotional support is facilitated through counseling services and support groups, which are critical for both patients and families navigating the complexities of illness. Additionally, spiritual care, often provided by chaplains or religious leaders, can address the emotional and existential needs during this phase. Various local and national organizations, such as the National Hospice and Palliative Care Organization (NHPCO), provide valuable information and education about available resources, ensuring families have access to necessary support. In-home nursing services and respite care options allow families to maintain comfort in familiar settings, while bereavement services offer continued support following the loss of a loved one. Understanding these resources promotes dignified and compassionate care during challenging times.
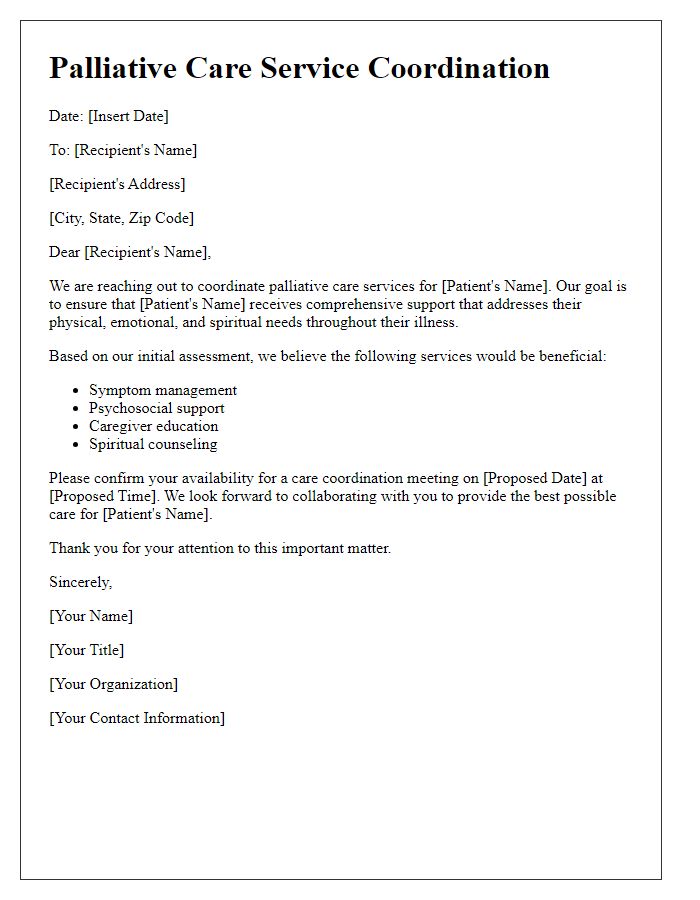
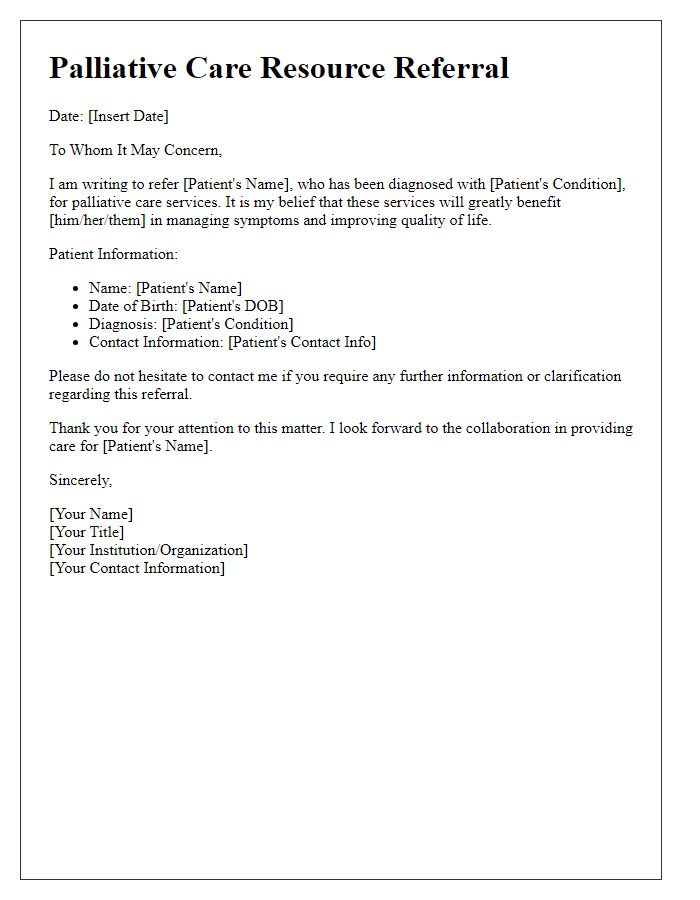
Communication and Coordination Plan
Palliative care arrangements emphasize the importance of communication and coordination to ensure comprehensive and compassionate support for patients and their families. Key components include the establishment of a dedicated interdisciplinary team (such as doctors, nurses, social workers, and chaplains) that collaborates on an individualized care plan tailored to specific patient needs. Regular team meetings should occur, ideally weekly or bi-weekly, to discuss patient progress and adjust care strategies. Effective communication with family members is crucial, incorporating scheduled updates and providing a contact person for ongoing inquiries, ensuring all parties are informed and comfortable with the care process. Clear documentation of care goals, preferences, and any advance directives should be maintained in a centralized electronic health record (such as Epic or Cerner) accessible to all team members. Additionally, community resources (like hospice services and support groups) should be identified and integrated into the care plan to provide further assistance to families during this challenging time.
Legal and Ethical Considerations
Palliative care offers specialized medical support aimed at alleviating symptoms associated with serious illnesses, such as cancer or advanced neurological disorders. Patients often face crucial legal and ethical issues related to their care preferences, including advanced directives, which are vital documents specifying individual healthcare wishes, especially regarding end-of-life options. Key considerations involve the establishment of a healthcare proxy, who will make decisions on behalf of the patient if they become incapacitated. Informed consent is paramount; patients must fully understand treatment options, potential side effects, and the implications of their choices. Ethical dilemmas frequently arise in discussions about life-sustaining treatments, with frameworks like beneficence (acting in the best interest of the patient) and autonomy (respecting patient choices) guiding healthcare providers. Effective communication within multidisciplinary teams, including doctors, nurses, and social workers, ensures that care aligns with the patient's values and goals, fostering a compassionate approach to end-of-life care.


Comments