Navigating medical expenses can often feel overwhelming, especially when it comes to seeking reimbursement for unexpected costs. Whether you've faced a sudden healthcare need or routine treatments, understanding how to effectively communicate with your insurance provider is key. In this article, we'll explore a simple and effective letter template that will guide you through the reimbursement process with ease. So, let's dive in and make the task less dauntingâyour journey to reclaiming those funds starts here!
Patient's Full Name and Contact Information
Medical expense reimbursement requests require detailed documentation for processing. Patients, such as John Doe, must provide their full name and up-to-date contact information, including a valid phone number and email address, to facilitate communication. Additionally, including the patient ID number, insurance policy details, and the date of service are essential for the claims process. Specific charges must be clearly itemized on the invoice, with associated receipts attached, providing complete transparency for the reimbursement amount sought. Timely submissions of these documents, typically required within 30 days post-treatment, ensure a quicker resolution and reimbursement from insurance companies.
Insurance Policy Number and Provider Details
Medical expense reimbursement requires specific documentation, including insurance policy numbers and provider details. Accurate insurance policy numbers (often unique identifiers assigned by insurance companies) expedite the reimbursement process. Provider details encompass the name of the healthcare professional or facility, associated tax identification numbers (TIN), services rendered, and associated dates of service. This information is essential to validate claims with insurance providers, ensuring that incurred medical expenses comply with policy guidelines. Moreover, thorough documentation can lead to a faster approval cycle, reducing delays in reimbursable funds reaching patients.
Detailed Description of Medical Procedures/Services
Medical expense reimbursement claims require a comprehensive breakdown of the medical procedures and services sought. This includes specific treatments, such as surgical interventions, diagnostic tests, and consultations, noting the medical professional's designation (e.g., cardiologist, orthopedic surgeon) and the establishment name (e.g., St. Mary's Hospital), along with treatment dates (e.g., January 15, 2023, for a knee surgery). Itemized bills should reflect costs associated with each service, including diagnostic imaging (like MRIs or X-rays) and any prescribed medications, specifying the pharmacy or provider. Detailed explanations of diagnoses, such as chronic pain or inflammation, as well as the necessity for treatments imposed by the healthcare professional, enhance the justification for reimbursement. Documenting follow-up visits or therapy sessions, including physical therapy sessions that occurred bi-weekly for recovery, is also crucial in providing a complete overview of incurred expenses.
Itemized List of Expenses with Original Receipts
Submitting an itemized list of medical expenses for reimbursement requires careful documentation. Original receipts serve as proof of payment for services rendered, such as visits to healthcare providers like doctors or specialists. Each entry on the itemized list should detail specific expenses, including date of service, description of service (consultation, surgery, etc.), name of healthcare provider, and total amount charged. In the United States, medical expenditures can encompass a range of items, from prescription medications (with costs averaging around $1,200 annually for individuals) to outpatient treatments at licensed facilities in various states (average $1,500 for minor procedures). Accurate submission is crucial to ensure timely reimbursement from insurance companies or employers, which often require adherence to specific guidelines set forth in their medical reimbursement policies.
Statement of Medical Necessity and Referral Documentation
Medical expense reimbursement often requires a Statement of Medical Necessity (SMN) to justify the need for specific treatments or procedures. This document is typically prepared by healthcare providers, detailing the patient's medical condition, the prescribed services, and their essential role in managing that condition. Common examples include surgeries, physical therapy sessions, and specialized medications that align with guidelines set forth by insurance companies. Referral documentation may accompany the SMN, showing the continuity of care, especially if the patient was referred to a specialist or required a unique treatment plan. These documents provide crucial support for reimbursement requests, ensuring that all necessary protocols and validations are met according to policies effective in fiscal year 2023.
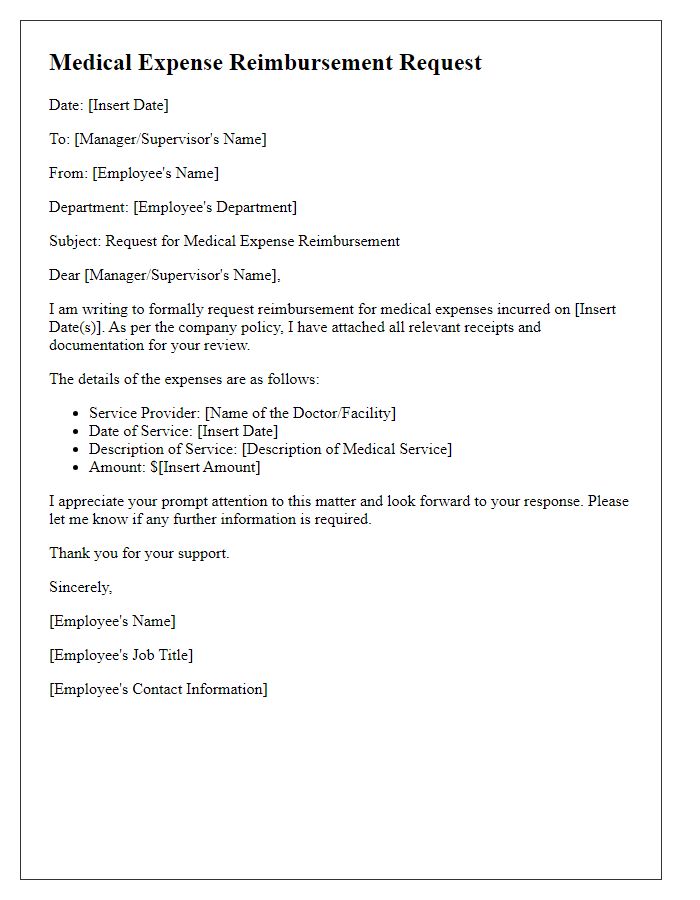
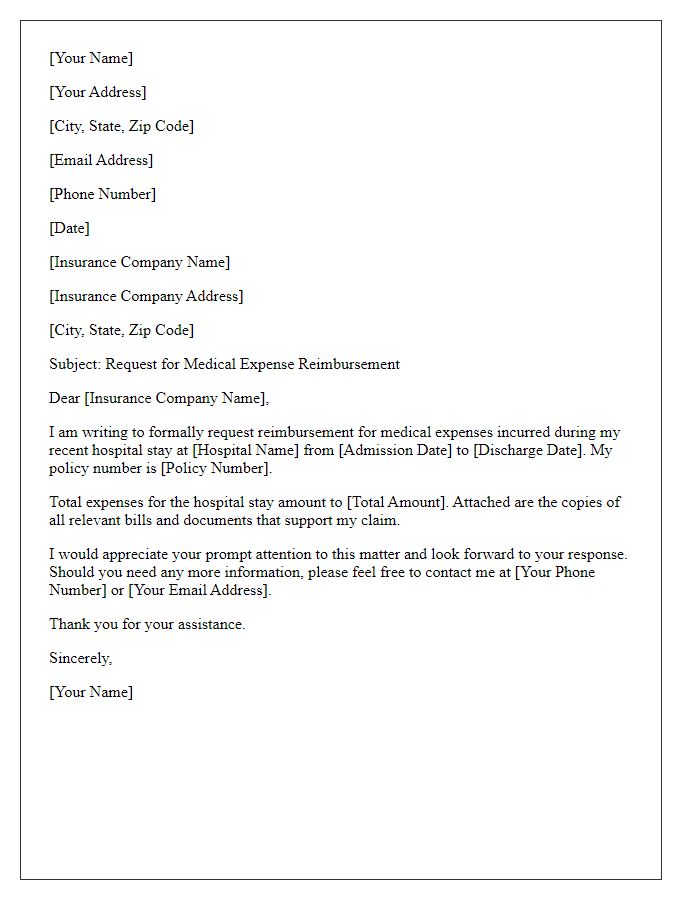
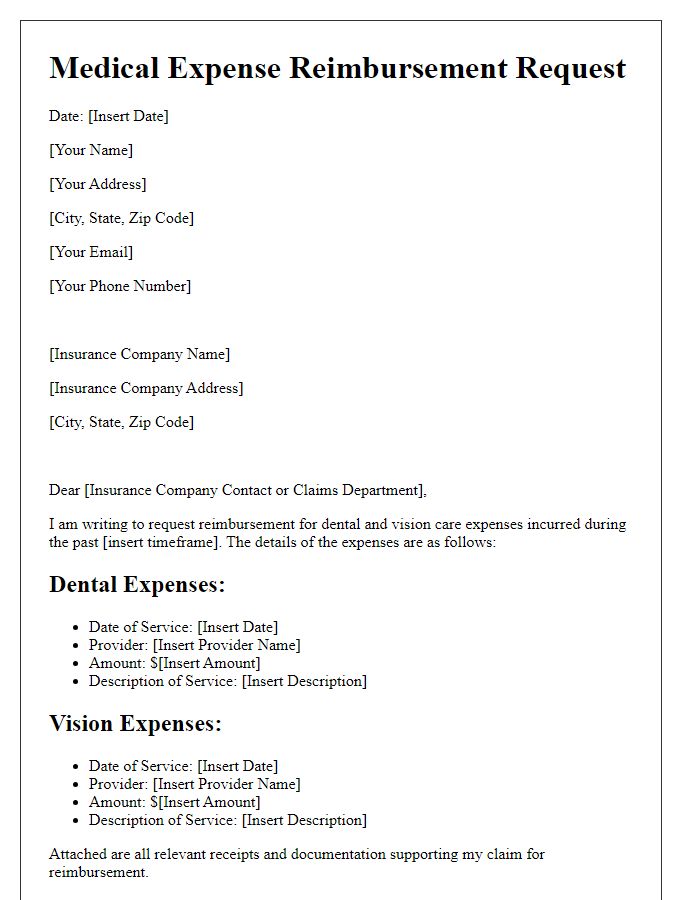
Letter Template For Medical Expense Reimbursement Samples
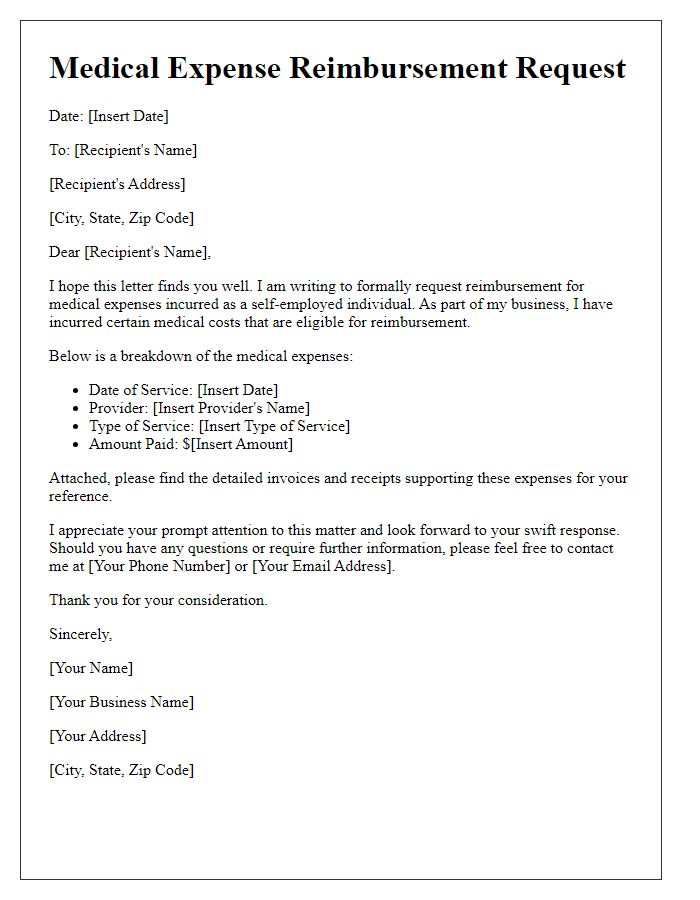
Letter template of medical expense reimbursement for self-employed individuals.
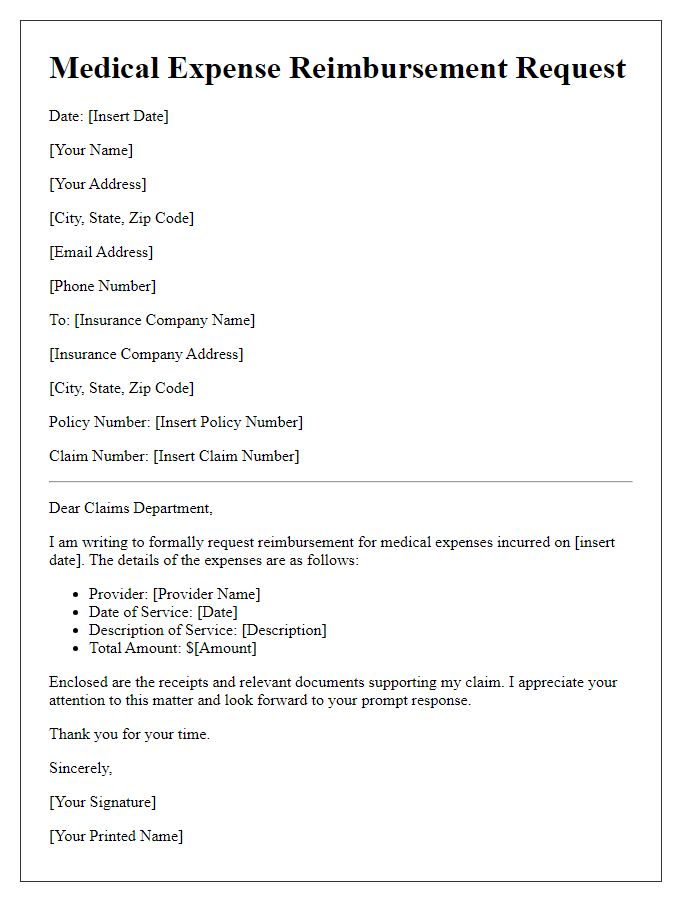
Letter template of medical expense reimbursement for health insurance claims.
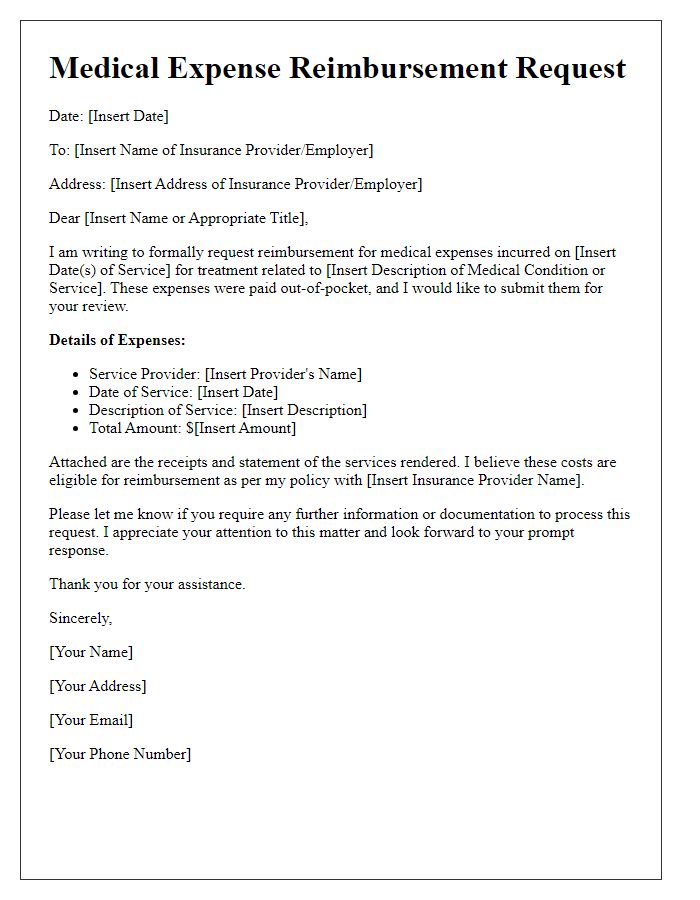
Letter template of medical expense reimbursement for out-of-pocket expenses.
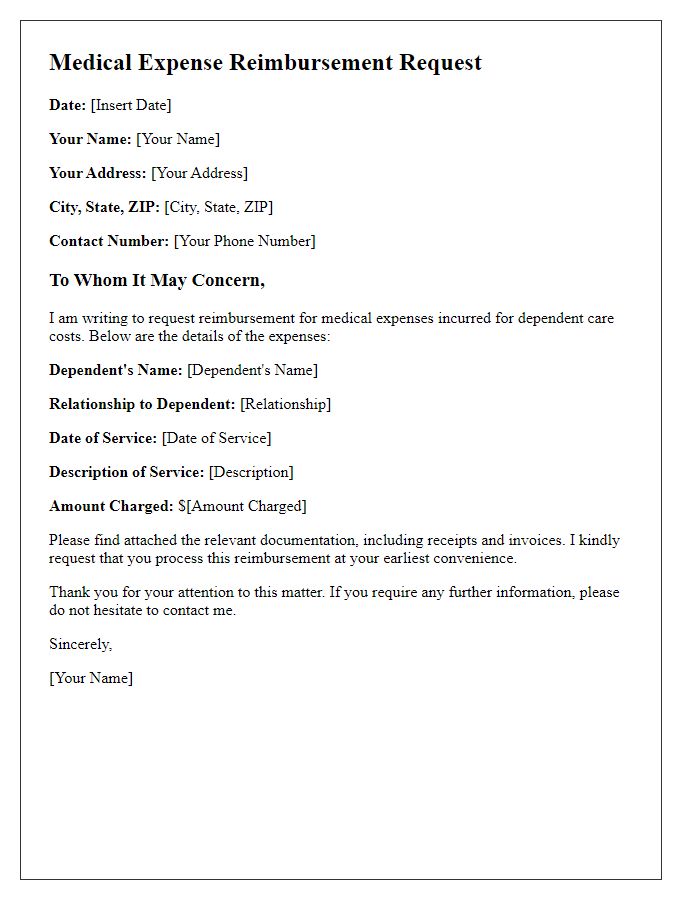
Letter template of medical expense reimbursement for dependent care costs.
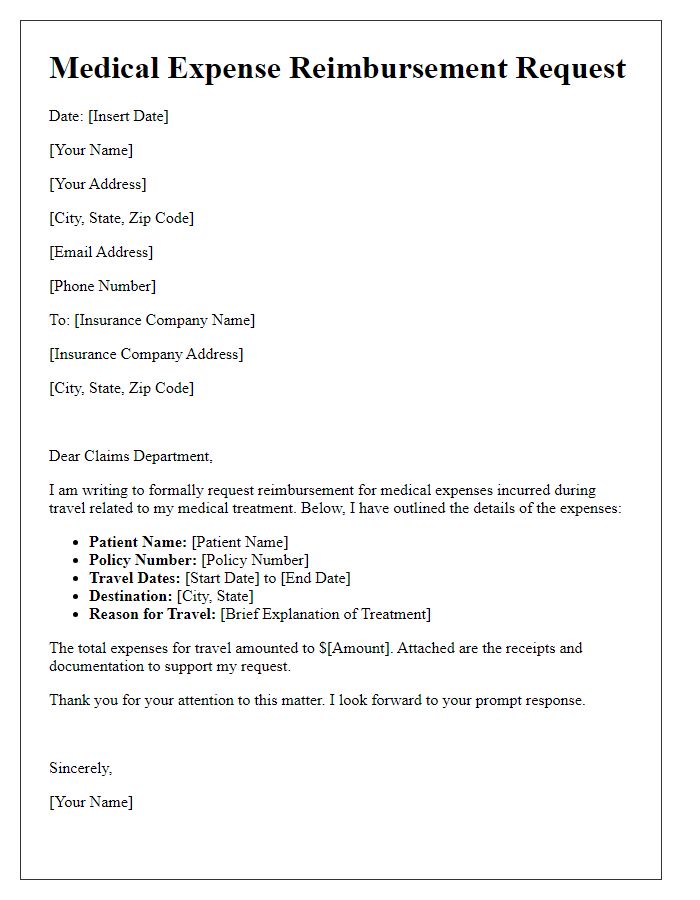
Letter template of medical expense reimbursement for travel related to medical treatment.
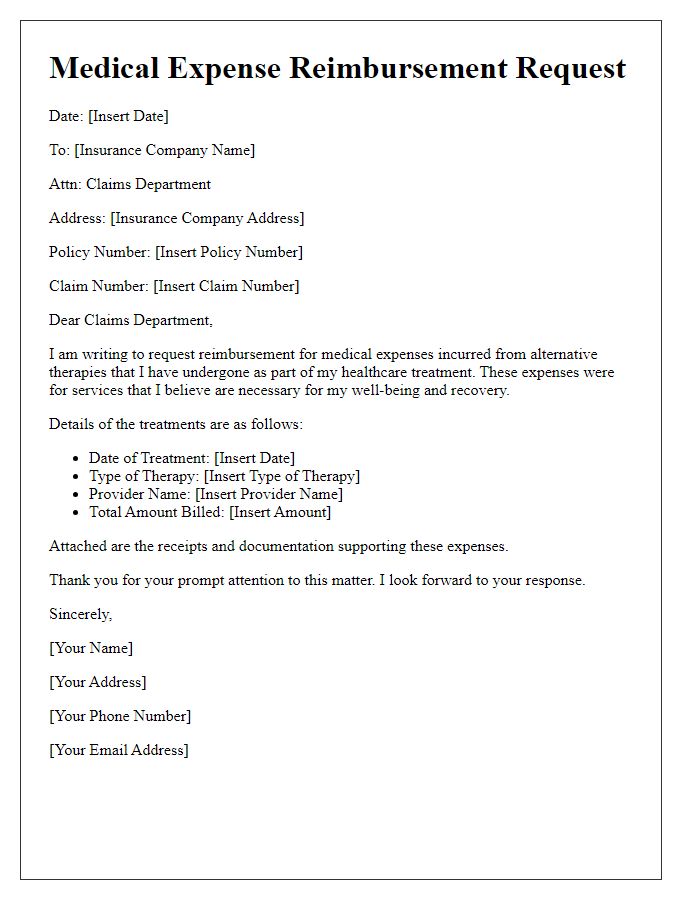
Letter template of medical expense reimbursement for alternative therapies.
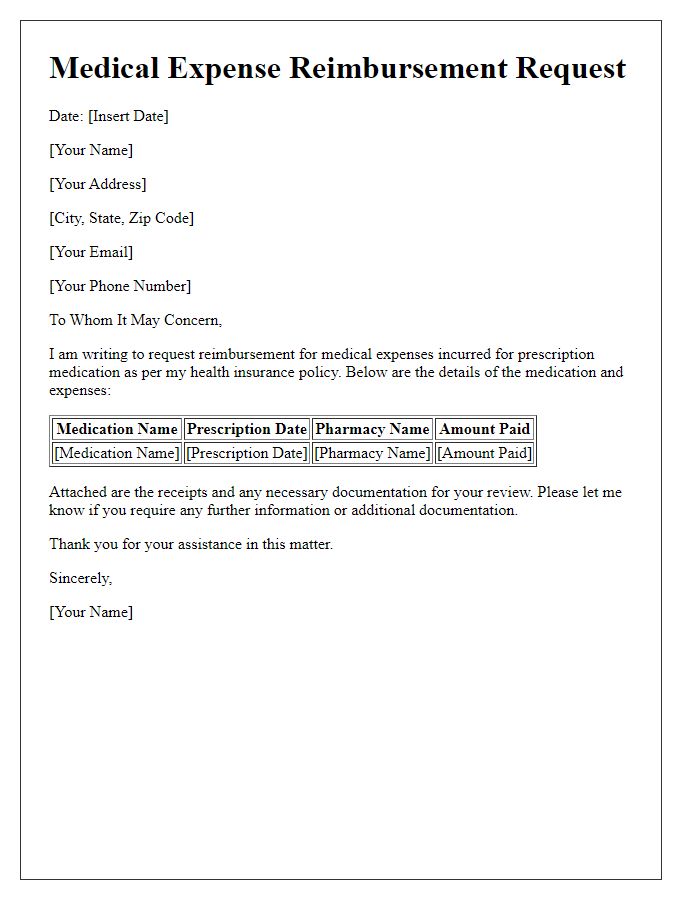
Letter template of medical expense reimbursement for prescription medication.


Comments